Roadmap to Integrated Care - Burrell Behavioral Health
advertisement

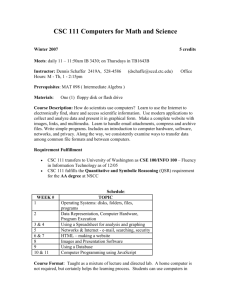
Research and Integrated Care Presented at the Roadmap to Integrated Care Conference Chateau on the Lake, Branson, MO June 4, 2015 Paul Thomlinson, PhD Objectives for Presentation 1. List the key components of the RAISE study and how this relates to treatment of patients with serious mental illness (SMI); 2. List and describe how to implement the empirically supported treatment program from RAISE; and 3. Demonstrate how to access current research findings and translate those into practice. Burrell is a National Institute of Mental Health Outreach Partner. This workshop is part of our ongoing efforts to promote empirically supported treatment and evidence-based research. A Prefatory Word (or Two) about EvidenceBased Practices… National Institute of Mental Health (NIMH): Recovery After an Initial Schizophrenia Episode (RAISE) • Two different RAISE projects: – Early Treatment Program (ETP) • With the Feinstein Institute for Medical Research, the research branch of the North Shore-LIJ Health System in Manhasset, NY. The Principal Investigator is John Kane, MD. – Connection • With Columbia University and provider organizations from NY state. The Principal Investigator is Lisa Dixon, MD, MPH. Developed/evolved into OnTrackNY. What is RAISE ETP? • “The goal of the RAISE Early Treatment Program randomized clinical trial is to compare NAVIGATE (a multifaceted intervention) to Community Care in individuals with early phase schizophrenia in order to investigate whether NAVIGATE can change the outcome and prognosis of individuals during a two-year treatment period.” Aims 1. To conduct an RCT in community clinical settings that will compare NAVIGATE, a comprehensive and integrated treatment intervention, to Community Care in the treatment of first episode psychosis. 2. To assess the overall clinical impact and costeffectiveness of NAVIGATE and Community Care on functional outcomes, symptom remission, recovery and cost. What is So? • “Schizophrenia is a major mental illness characterized by psychosis, negative symptoms (e.g., apathy, social withdrawal, anhedonia), and cognitive impairment.” • “…in 2001 approximately one-third of all spending for mental health treatment in the U.S. was accounted for by schizophreniaapproximately $34 billion…” So What? • RAISE ETP sought to change the trajectory and prognosis of schizophrenia through coordinated and aggressive treatment in early stages of the illness. • To reduce the likelihood of long-term disability, and increase the chances of helping individuals suffering from this disorder to lead productive, independent lives. • to reduce the costs related to treatment (both medical and behavioral health) and other supports (e.g., housing, disability, transportation, etc.). So? • We’re not sure yet… • We’re just starting to get word of publications and outcomes. Key Components of RAISE Services • The Coordinated Specialty Care (CSC) approach was used when developing the treatment model for both RAISE projects. – CSC is a team-based, collaborative, recovery-oriented approach to treating first episode psychosis (FEP) that involves relatives and clients as active participants in treatment. • Emphasizes shared decision-making, collaborative treatment planning, establishing positive therapeutic alliances, and integration (with primary medical care). • Evidence of effectiveness from broad implementation in Australia, UK, Scandinavia, and Canada. Key Components of RAISE Services • Components of care include: – – – – – Assertive case management, Individual and/or group therapy, Supported employment and education, Family education and support, and Low doses of select antipsychotic drugs. • Ideally designed for younger populations (15-25), with non-organic, non-affective psychotic disorders, who have been ill for five years or fewer. CSC & ETP NAVIGATE Protocol • Participants received any combination of: – – – – Medication Management – monthly visits Individual Resiliency Training (IRT) – weekly Family Education (FE) – weekly Supported Employment and Education (SEE) – weekly – Any other ‘standard’ community care services that may be necessary • E.g., community support/case management, substance abuse treatment, trauma-informed care, etc. RAISE ETP NAVIGATE Protocol • Project Director/Team Leader – Coordinated/Supervised RAISE team members (weekly or biweekly supervisions) – Facilitated weekly RAISE team meetings to discuss each clients’ needs, service utilization/ engagement, treatment plans/goals, crises, and successes. – Outreach to stimulate referrals – Screened, consented, & enrolled new clients into RAISE (and other Burrell services, through internal referral mechanisms) – Coordinated with Evaluation and Administrative staff for data collection and administrative purposes. RAISE ETP NAVIGATE Protocol • Medication Management – Monthly medication management visits (30 min) with an online decision-support tool (Compass) to collect data on symptoms, side effects, perceptions and use of meds. • The tool utilized algorithms (from Texas) to make recommendations on prescriptions. – Performed physical evaluation for movement disorders, reviewed results of tests for monitoring side effects, participation in weekly team meetings and treatment planning RAISE ETP NAVIGATE Protocol • Individual Resiliency Training (IRT) – Provided motivational enhancement interventions: motivational interviewing, weighing pros & cons of behavior change, breaking goals into smaller steps, etc. – Provided psycho-education: information about psychiatric disorders & treatment. – Provided cognitive behavioral therapy: social skills training, relaxation training, coping strategies for persistent symptoms, psychiatric relapse prevention training, cognitive restructuring, & behavioral tailoring (incorporating medications into daily routine). – Providing cognitive behavioral therapy for substance abuse: teaching social skills, drug/ alcohol refusal, relaxation, coping with persistent symptoms, relapse prevention & cognitive restructuring – Participation in treatment planning: short-term & long-term goals (every 6 months) – Providing assessments: both standardized (PTSD checklist) and nonstandardized – Participated in weekly team meetings – Participated in family meetings (as needed) RAISE ETP NAVIGATE Protocol • Family Education (FE) – Provided education to family members about the client’s psychiatric illness – Encouraged family members to be supportive of the client in obtaining desired goals – Helped elicit strengths, preferences, and history, helped develop shared understanding of desired goals – Gathered important information, problem-solving, developed family coping skills strategies – Provided motivational interviewing interventions to build family support – Taught family members symptom management strategies – Enhanced family communication styles & problem solving skills – Provided Cognitive- Behavioral strategies to help families assist clients to better manage symptoms – Participated in weekly team meetings – Participated in family meetings RAISE ETP NAVIGATE Protocol • Supported Employment and Education (SEE) Specialists – Performed assessments: gathered information about functional impairments from psychosis as they relate to education &/ or employment goal attainment – Provided psychoeducation about psychosis as it relates to attaining education &/ or employment goals – Provided social skills & relapse prevention training for managing symptoms as they relate to goals for education &/ or employment – Provided guidance and education related to employment as it relates to eligibility for Medicaid and other entitlements, etc. – Provided job development, due to functional limitations – Provided assistance with enrollment in education – Provided follow-along supports, social skills training, relapse prevention skills – Participated in weekly team meetings – Participated in family meetings (as needed) Implementing EBP for FEP • H.R. 3547 - Consolidated Appropriations Act, 2014 • Provided funds to the Substance Abuse and Mental Health Services Administration (SAMHSA) to support the development of early psychosis treatment programs. National Institute of Mental Health is collaborating with SAMHSA to ensure fidelity to EBP models and to develop input for states about promising first episode psychosis (FEP) treatment models. • Coordinated Specialty Care (CSC) resources and program development materials—including treatment manuals, videos, educational handouts, and worksheets—are available to assist in efforts to initiate or expand CSC services for youth and young adults with FEP. • Resources are available at: – http://www.nimh.nih.gov/health/topics/schizophrenia/raise/coordinat ed-specialty-care-for-first-episode-psychosis-resources.shtml – White Paper • Evidence-Based Treatments for First Episode Psychosis: Components of Coordinated Specialty Care Implementing EBP for FEP • Components to consider for CSC: – Components of care & staffing needs, – Training and supervision requirements, – Quality assurance, and – Financing Implementing EBP for FEP • Components of Care and Staffing Needs – CSC Team Leader • Provides ongoing consultation to team members, coordinates key services (screening, leads weekly meetings, treatment planning, referral sources, etc.), – Case Management • Assists clients with problem solving, coordinates social services across multiple areas of need. Regular community-based meetings. – Supported Employment and Education • Facilitates return to work or school through goalsetting, coaching, and integrating vocational and mental health services. Implementing EBP for FEP • Components of Care and Staffing Needs – Psychotherapy • Based on CBT principles, emphasizes resilience training, illness and wellness management, and general coping skills. • One-on-one and/or group therapy – Family Education and Support • Teaches relatives and other natural supports about psychosis and treatment. Strengthens supports’ capacity to aide in the client’s recovery Implementing EBP for FEP • Components of Care and Staffing Needs – Medication Management & Primacy Care Coordination • Uses evidence-based medication management practices to guide the prescription (selection and dosing) of antipsychotic and other psychopharmacological agents. • Monitors of symptoms, side effects, and attitudes toward medications at every visit. • Monitors cardiometabolic risk factors and maintains close contact with primary care providers. Implementing EBP for FEP • Components of Care and Staffing Needs – Community Outreach • To identify and engage clients as early as possible, to reduce the duration of untreated psychosis – Client and Family Engagement • Clients and natural supports can be difficult to engage. Specific techniques and language is necessary to help increase clients and supports feel comfortable. – Mobile Outreach and Crisis Intervention Services • To engage clients who have difficulty with clinic-based services, or who need assistance in addressing complex needs. • 24-hour crisis line can effectively avert many emergency department visits and hospitalizations Implementing EBP for FEP • Components of Care and Staffing Needs – Transition of Care • Highly coordinate, gradual transition to standard behavioral health services. • Evidence suggests that continuity of care for up to five years after psychosis begins can improve the durability of effects of early intervention CSC services. • Step-down in care should involve ongoing connection with one member of the CSC team for an additional 1-3 years. CSC Role Services Coverage Status Team Leadership Cultivate referral networks; facilitate access to care; outreach to patients and family members; coordinate clinical services among team members; provide ongoing clinician supervision Not Covered Psychotherapy Provide individual and group psychotherapy sessions, including integrated substance abuse sessions when needed Billable via CPT 90832; 90834; 90853 Case Mgmt Perform assertive case mgmt functions in clinic and community settings Inconsistently covered (may only include Medicaid) Family Education & Support Provide psychoeducation, relapse prevention counseling, and crisis intervention services. Billable via CPT 90846; 90847; 90849 SEE Implement IPS model of supported employment and supported education; provide ongoing client support following job or school placement Inconsistently covered (may only include Medicaid) Med Mgmt & Primacy Care Coordination Medication management; coordination with primary medical care Billable via CPT 99214 CSC Team-Level Activity Team meetings, coordination of services among team members, CSC training, clinical supervision, 24-hour phone coverage for managing crisis situations Not Covered *Note – this table was taken originally printed in the Evidence-Based Treatments for First Episode Psychosis: Components of Coordinated Specialty Care document, pp-14-15; http://www.nimh.nih.gov/health/topics/schizophrenia/raise/coordinated-specialty-care-for-first-episode-psychosis-resources.shtml Implementing EBP for FEP • Training and Supervision Requirements – Training for EBP in FEP is necessary to ensure fidelity and efficacy – Two levels: • Philosophy of team-based care for FEP – For all team members – Includes: » Theoretical framework of CSC » Recovery potential for FEP clients » Developmental issues specific to adolescents/young adults experiencing FEP » Concepts of shared decision-making » Concepts of person-centered care » Maintaining optimistic therapeutic perspective » Engagement barriers and strategies » Co-occurring substance use problems » Suicide risk during early years of treatment • Specialized services that support recovery after FEP – Specific to each specialized role on the team Implementing EBP for FEP • Training and Supervision Requirements – Ongoing supervision and continuing education for all staff – Weekly case reviews to reinforce CSC treatment principles and ensure competence in FEP care • Training materials developed by both RAISE ETP and Connection programs – – – – Rational for early intervention Principles of team-based care Providers’ roles and related clinical services Core competencies related to specific treatment modalities Implementing EBP for FEP • Quality Assurance and Performance Improvement – Primary questions: • Are CSC team members implementing interventions as intended? • Are providers delivering what was promised in the service contract? • Have CSC services achieved desired clinical and functional outcomes for clients with FEP? Implementing EBP for FEP • Quality Assurance and Performance Improvement – Assuring Fidelity • Through records reviews, surveys, and interviews. • Routine Service Logs, EHR, medical records. • ID indicators or proxies for primary principles in clinical documentation and track over time. • Client satisfaction surveys • Staff Perception, Engagement, or Satisfaction Surveys Implementing EBP for FEP • Quality Assurance and Performance Improvement – Outcomes measurement • Functioning/ functional indicators (school/ work involvement, ER visits, hospitalizations, drug use, arrests/ legal involvement, etc.), symptoms, quality of life, etc. CSC Program Development Resources • http://www.nimh.nih.gov/health/topics/schizophrenia/raise/coordi nated-specialty-care-for-first-episode-psychosis-resources.shtml • NIMH White Paper – Evidence-Based Treatments for First Episode Psychosis: Components of Coordinated Specialty Care • RAISE Connection – CSC for FEPT Psychosis Manuals • Manual I: Outreach and Recruitment • Manual II: Implementation – Video Series: Voices of Recovery – Performance, Quality, and Fidelity Indicators – Additional resources: http://practiceinnovations.org/OnTrackUSA/tabid/253/Default.aspx CSC Program Development Resources • RAISE ETP – NAVIGATE Team Members Guide – NAVIGATE Team Leader Manual – IRT Manual & Demo/Training Videos – Family Education Manual – SEE Manual – Medication Management Manual – http://navigateconsultants.org/materials/ Conclusions and Q&A