Acid Peptic Disease : Therapeutic Concepts
advertisement
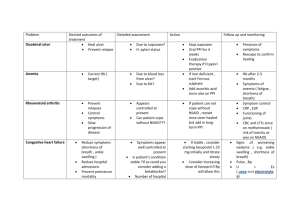
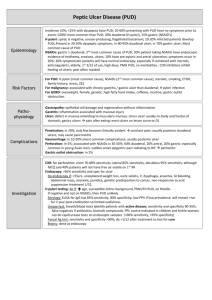
Acid Peptic Diseases Clinical Management Course February 2007 Walter Smalley, MD MPH Acid - Peptic Diseases • Drugs • Antacids • H2RAs (“H-2 blockers”) • Proton Pump Inhibitors (PPI’s) • Selective COX-II inhibitors • Conditions Covered • Heartburn • Gastroesophageal Reflux (GERD) • Peptic Ulcer Disease • H. Pylori • NSAIDs Antacids • • • • Immediate effect on gastric pH Effect is short-lived Typical dose 30-60 cc Frequent use may cause diarrhea H-2 Receptor Antagonists • • • • • • Inhibit H-2 receptors (competitive inhibition) Partially inhibit acid production Relatively safe drugs Less effective than PPI’s Less expensive than PPI’s Available over the counter: at prices more expensive than prescription costs Cimetidine : Safety Considerations • Brand name Tagamet • Induces cytochrome p450 system • Drug interactions with coumadin, theophylline, dilantin and others • Rarely clinically relevant • But “why not use ranitidine” • Confusion in the elderly • Thrombocytopenia H2 blockers : No difference in efficacy within group Ulcer treatment Cimetidine (Tagamet) Ulcer GE Reflux maintenance treatment (BID to QID) 800 - 900mg QHS 300 mg QHS > 1200 mg QD Ranitidine (Zantac) 300 mg QHS 150 mg QHS > 300 mg QD Nizatidine (Axid) 300 mg QHS 150 mg QHS > 300 mg QD Famotidine (Pepcid) 40 mg QHS 20 mg QHS > 40 mg QD Proton Pump Inhibitors • • • • Raise gastric pH to > 5 for several hours Binds covalently to H+/K+ pump Prodrugs: bioavailable at acid pH Maximal effectiveness • After several doses • When taken before meals • After a long fast • (Prior to breakfast) Proton Pump Inhibitors • Omeprazole • (generic cost about 80% of prescription costs ) • Immediate release omeprazole • Lansoprazole • Rabeprazole • Pantoprozole – oral and IV form • Esomeprazole • Very effective, no important predictable differences in efficacy • Very expensive ($2-4/day) • ~ $1 per day generic Case 1 • • • • 35 year old healthy man Occasional heartburn Occurs only with large meals, EtOH ingestion No dysphagia Heartburn : Summary • How soon does the patient want relief ? • How long does it need to last ? • How much are they willing to pay ? Heartburn : Summary • Prevention • Antacids are effective immediately in reducing acid work for 1-2 hours • H2-blockers are effective in 1-2 hours - they work for > 6-8 hours • Available over the counter Case 1 • Consider not eating large meals • Consider PRN antacids • Consider OTC H2 blockers • On the horizon ? • Immediate release omeprazole – • Direct to consumer marketing • Marginal benefit vs other PPIs Case 2 • 50 yo with frequent nocturnal heartburn • No dysphagia • Trial of lifestyle modification only minimally effective • Antacids ineffective GERD: When to perform diagnostic tests • Endoscopy • Dysphagia • Weight loss • Age > 50 • Failure of medical therapy • Motility : prior to fundoplication • pH monitoring: might resolve diagnostic uncertainty in absence of esophagitis Gastroesophageal Reflux • Reflux of gastroduodenal contents • Acid ( gastric) • Alkaline (biliary, pancreatic) • Decreased lower esophageal sphincter (LES) tone • Decreased rate of gastric emptying • Increased intra-abdominal pressure • Decreased salivary clearance GERD: Lifestyle Modification • • • • weight loss, avoid tight-fitting clothes NPO 3-4 hours before bedtime elevate head of bed 8'' avoid foods and drugs that decrease LES pressure or gastric emptying rate • fat, EtOH, tobacco , peppermint, garlic, onions, chocolate, Ca++channel blockers, nitrates, theophylline, antidepressants • No strong RCT evidence to support important effect of lifestyle modification Case 2 • 50 yo with frequent nocturnal heartburn • No dysphagia • Trial of lifestyle modification only minimally effective • Antacids ineffective • EGD - distal esophageal erosions GERD : Overview • Antacids: temporary relief • H2-antagonists: • high (“double”) doses, frequent dosing • Prokinetics: as effective as H2RA’s • Metoclopramide • Proton pump inhibitors: • most effective • most expensive GERD: H2-antagonists • NO BETWEEN - DRUG DIFFERENCES IN EFFICACY • symptomatic relief < 60 - 70% cases • endoscopic improvement < symptomatic relief • higher doses (>2X ulcer doses) improve efficacy slightly GERD : Prokinetic Agents • Metoclopramide • As effective as H2RAs • Adverse reactions: – fatigue, lethargy, extrapyramidal symptoms occur in 10% - 30%. Case 2 • Continue lifestyle modification • Trial of H2 blockers at high doses Case 3 • Patient #2 returns after 8 week trial of H2 blockers • Therapy only minimally effective GERD : Proton Pump Inhibitors • Causes healing and resolution of symptoms in 80% of patients with disease resistant to H2-blockers • Expensive, single source drugs ($ 2 - 4 / day) • Over the counter more expensive than prescription • Not on Wal-mart list • Generic omeprazole still > $1 per day Case 3 • Proton pump inhibitor Case 4 • • • • Patient from Case 3 returns Symptoms well controlled on omeprazole Symptoms recur immediately after stopping drug “Hates taking meds” GERD: Anti - Reflux Surgery • Indications: • patient preference over drug treatment • young patients with severe esophagitis • difficult to dilate strictures • recurrent esophageal ulcers • GER-respiratory/ENT syndromes • 80 - 90% of cases have some improvement GERD: Anti - Reflux Surgery • Side effects: about 10 % cases • "gas bloat" • dysphagia • strictures • other • Usually won’t work if PPI’s don’t work Utilization of GERD pharmaceuticals in patients treated medically and surgically Acid suppression days per quarter Most fundoplication patients end up taking some acid meds after operation Khaitan et al, Arch Surgery 2003 Endoscopic therapies for GERD • Stretta: radiofrequency destruction of GEJ myenteric plexus • Endoscopic Plication: sewing gastric cardia mucosa to augment GEJ • Injection of GEJ with plastic (removed from market) • All should be considered experimental at this point Case 4 • Consider anti reflux procedure • Weighing potential benefits of not taking medication vs. risk of side effects from surgery (probably 1- 3% in experienced hands) Case 5 • 40 yo with epigastric pain “ALARM FEATURES” •unexplained weight loss • anorexia • early satiety • vomiting • progressive dysphagia • odynophagia • bleeding • anemia • jaundice • abdominal mass • lymphadenopathy • family history of upper GI cancer • history of peptic ulcer, previous gastric surgery or malignancy. ACG dyspepsia management guidelines Case 5 • 40 yo with epigastric pain • Relieved with meals • No clinical signs of bleeding • No vomiting • Reasonable approaches • Empiric trial of acid suppression • “Test and treat” for H pylori • Refer for endoscopy Case 5 • 40 yo with epigastric pain • 8 week trials of PPI fails • EGD : duodenal ulcer • H pylori positive • no NSAIDs confirmed Ulcer Disease : Basic Concepts • • • • • H. pylori is associated with GU and DU NSAID use is associated with GU and DU Most ulcers are not the result of excess acid Acid suppression aids in healing ulcers Prior to the H pylori era: most of the cost of ulcer disease had been in “maintenance” therapy H pylori : Concepts • • • • H pylori infection is chronic Prevalence in US adults = 50 - 80% Lifetime risk of ulcer disease = 10% Associated with chronic gastritis - a histological diagnosis • H pylori is a risk factor for gastric adenocarcinoma H pylori - Diagnosis • EGD – • Biopsy for histology and CLO • Breath Tests – • commercially available • big hassle • Serology – • widely available, • followup is problematic (positivity persists months after eradication) • Stool antigen test: • problem = it’s stool. H pylori. treatment - Efficacy • For treatment of duodenal ulcer > gastric ulcer • Eradication of H.pylori alone = treatment with H2blockers alone • For preventing recurrent duodenal ulcer: • Eradication of H.pylori >> continuous H2-blocker therapy • Marginal (if any) benefit in treating non ulcer dyspepsia H pylori. treatment - Options • • • • Many different regimens No "standard of care" Best therapy yet to be determined Big problems • compliance • resistance • Current (2/07) favorite combination • Amoxicillin, PPI, Clarithromycin • Metrondazole, PPI, Clarithromycin Peptic Ulcer: Treatment Outcomes Efficacy : 8 weeks Efficacy : 1 year chronic acid suppression Efficacy : 1 year without acid suppression Sucralfate 70 - 90% NA 60 - 70% H2-antagonists 70 - 90% 70 - 90% 50 - 75% Omeprazole > 95% 70 - 90% 50 - 75% H. pylori eradication > 95% >90% > 90% Case 5 • Treatment with acid suppression • QD H2 blockers, or • proton pump inhibitor • Treat H pylori • Amoxicillin 1000 BID • Clarithromycin 500 BID • Omeprazole 20 BID Case 6 • • • • 65 yo male with osteoarthritis with recent ulcer On ibuprofen 1800 mg per day Ulcer has healed H pylori negative NSAIDs and Ulcers - Concepts • Higher doses ---> greater risk • Long time users still have increased risk after 12 months • Absolute risk is high • about one ulcer hospitalization per 100 person years in the elderly • About 2/3 of ulcers in NSAID users are due to the NSAID use • By far our most important complication of pharmaceutical use NSAIDs and PUD : Treatment • Stop NSAIDs • Acid suppression Drug • Omeprazole • H2-Blockers • Misoprostol • Sucralfate Healing at 6 - 8 weeks > 90% 70-90% 70-90% not effective NSAIDs and Ulcers - Prevention • Does the patient really need NSAIDs ? • objective = pain control • NSAIDs do not prevent progression in osteoarthritis • little evidence demonstrating superiority of NSAIDs over acetaminophen in osteoarthritis patients. • No NSAID is "safe". NSAIDs and Ulcers - Prevention • Misoprostol - a synthetic PGE analog • Prevents GU and DU • Expensive therapy - for prevention. • Debate on cost effectiveness continues. • Side effects: diarrhea (10%), abdominal pain (10 20%) • Causes spontaneous abortions - do not use in potentially fertile women NSAIDs and Ulcers - Prevention • H-2 blockers at high doses may be reliable preventive agents for DU prevention • Misoprostol is very effective in preventing ulcers in clinical trials. • PPI’s are as probably as effective as misoprostol and better tolerated • Eradicating H pylori is helpful in preventing recurrence (RCT evidence) Selective COX-II Inhibitors: COXIBs • Celecoxib, rofecoxib, valdecoxib, etoricoxib and lumiracoxib • NO more effective than traditional NSAIDs • Potential benefit is GI safety • Still have renal toxicity, other toxicities ? • Large trials demonstrate decreased ulcer rate • Decrease of about 50% • Do high-risk patients still need acid suppression ? • Risk of cardiac events has led to the removal of rofecoxib and valdecoxib Results from a polyp prevention trial Case 6 • Consider alternatives to NSAIDs • • • • narcotics non-narcotics physical therapy topical therapy • Consider misoprostol • Consider acid suppression with PPI • For now would not consider any COXIB drugs left on the market Peptic Ulcer Disease • Stop NSAIDs. • Acid suppression acutely • Test for H pylori and treat if present. Case 7 • 75 yo admitted with hematemesis, shock • Intubated for airway protection (NPO) • EGD reveals gastric ulcer with visible vessel • Treatment with heater probe controls bleeding Acid Suppression • There is evidence that acid suppression may decrease rebleeding rates, surgical rates, and hospital days • There is no evidence that it saves lives • (studies would have to be huge) • Most IV PPI data is based on trials using IV OMEPRAZOLE which is not available in the US • Most studies involved bleeding ulcers requiring endoscopic therapeutic interventions (injection therapy or heater probe) Proton pump inhibitor (IV or PO) Moderate effects on: •reduced rebleeding (table left) •OR 0.46, 95%CI 0.33 to 0.64 •NNT =12 •surgery •OR 0.59 95%CI 0.46 to 0.76 •NNT = 20 treatment had no significant effect on mortality •OR 1.11, 95%CI 0.79 to 1.57 •NNT = incalculable Lancet 2005 PPI’s Summary • In the select group of patients who require endoscopic therapy the few published studies demonstrated potential advantage for IV Omeprazole • In our settings most endoscopies will be done quite early - there is little advantage in starting IV PPI’s prior to EGD in most cases • Oral PPIs may have some protective effect compared to placebo Case 7 • Start IV Pantoprazole (80 mg bolus followed by 8 mg per hour) • Start PPI of choice after patient is taking oral meds