PowerPoint - Tennessee Psychological Association
advertisement

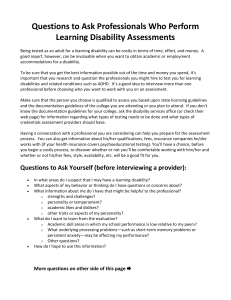
Disability Models, Stereotypes, and Clinical Implications ERIN N. ARMOUR, PSY.D. JAMES H. QUILLEN VA MEDICAL CENTER MOUNTAIN HOME (JOHNSON CITY), TN PRIVATE PRACTICE GRAY, TN TENNESSEE PSYCHOLOGICAL ASSOCIATION CONVENTION OCTOBER 31, 2015 Learning Objectives Attendees will be able to identify various demographics, risk factors, and psychosocial stressors associated with disability. Attendees will be able to define four models of disability. Attendees will be able to identify at least two disability stereotypes. Attendees will be able to describe at least three clinical implications for working with persons with disabilities. Exercise: The Disability Quiz Handout: The Disability Quiz Place an X next to the conditions you think represent a disability. College committee for diversity, equity, and affirmative action. (2014). A booklet of interactive exercises to explore our differences. Retrieved October 1, 2015 from http://intraweb.stockton.edu/eyos/affirmative_action/content/docs/Interactive%20Div ersity%20Booklet%2010-14-2011.pdf Discussion: Processing The Disability Quiz • How did you determine your answers? • Do some traits/disabilities seem less socially acceptable than others? • Do we think of some traits as making us less able to function in society? • Does disability depend on how well society adjusts to meet peoples’ needs? • How do you define disability? Disability Defined Americans with Disabilities Act (1990): “Disability: (A) a physical or mental impairment that substantially limits one or more of the major life activities of such individual; (B) a record of such impairment; or (C) being regarded as having such impairment (Section 1630.2). TABs = Temporarily Able-Bodied Persons; PwDs= Persons with Disabilities No single definition; disability exists on continuum Olkin, Rhoda. (1999). What psychotherapists should know about disability. New York: Guilford Press. Risk Factors Who is at risk to become seriously ill or disabled? We are all at risk for becoming seriously ill or disabled. Which behaviors increase and/or decrease that risk? PwDs are more likely than TABs to be obese, smoke, or binge drink. TN leads the nation in the number of persons who smoke and report at least one disability (Stoddard, 2014). Handout: What’s your Personal Disability Quotient (PDQ)? Risk Factors Higher rates of depression, anxiety, intimate partner violence (women with disabilities), and substance abuse (including tobacco) compared to TABs. Nosek, M. A., Foley, C. C., Hughes, R. B. & Howland, C. A. (2001). Vulnerabilities for abuse among women with disabilities. Sexuality and Disability, 19, 177-189. Disability Prevalence PwDs are the largest minority group in the United States. In 2013, 12.6% of persons of all ages in the United States reported 1+ disabilities. Other estimates are as high as 18.7% of civilians. Stoddard, S. (2014). 2014 Disability statistics annual report. Durham, NH. University of New Hampshire. Disability Prevalence (By): Type: ambulatory disabilities are most common. Visual disabilities are least common. Gender: disability more common in adult females than adult males (12.7% vs. 12. 4% ); reversed in children. Age: 26% of persons ages 65-74; 50% of persons ages 75+ State: TN: 14.4%; WV: 19.2%; Kentucky: 16.1%; Ohio 12.3%; Georgia 11.3%; Virginia: 9.3% Stoddard, S. (2014). 2014 Disability statistics annual report. Durham, NH. University of New Hampshire. Disability Prevalence (By): Race: 4.6% Asians; 10.7% Caucasians; 14.1% African Americans; and 18.4% Native Americans Stoddard, S. (2014). 2014 Disability statistics annual report. Durham, NH. University of New Hampshire. Employment & Economic Demographics Employment: Only 33.9% of PwDs of working age are employed at least part-time compared to 74.2% of TABs. Employment rates are highest for those w/ hearing disabilities; lowest for those w/ self-care and independent living disabilities. Almost 30% of PwDs of working age live in poverty; compared to 13.6% of TABs. Stoddard, S. (2014). 2014 Disability statistics annual report. Durham, NH. University of New Hampshire. Education Demographics Only 34.4% of PwDs complete high school; 12.4% complete a bachelor’s degree or higher. Erickson, W., Lee, C., & von Schrader, S. (2014). 2012 Disability Status Report: United States. Ithaca, NY : Cornell University Employment and Disability Institute (EDI). Exercise 2: Privilege Checklist How many of these items apply to you? Why or why not? What reactions do you have? Psychosocial Stressors Items on privilege checklist (see handout) Secondary health conditions Lower than average income and economic resources can limit access to medical and mental health care. Stigma can also serve as a barrier to PWDs accessing quality medical care. Higher than average cost of living, often due to higher than average medical costs. Home and vehicle accessibility and modification. Disability Models 4 Socially Constructed Disability Models Moral Model Medical Model Functional/Environmental Model Social/Minority Model Moral Model Disability is the result of the sins of the PwD and/or his or her family. The disability is considered to be a test of the family’s strength or faith (Olkin, 1999). Disability is “treated” with religious education classes or spiritual healings (repentance; Smart & Smart, 2006). “God has a plan.” “He doesn’t give us more than we can handle.” Medical Model Disability is the result of abnormality or pathology that can, and should be “fixed.” Healthcare providers are the “expert,” the recommendations of whom PwDs should follow (Smart & Smart, 2006). Environmental/Functional Model Recognizes that the environment, including societal attitudes, can contribute to or exaggerate limitations. Disability results from the functional requirements of the environment. PwDs are ascribed a “sick” role, or a subservient position in society, and society “functions properly” when they remain in that role. (Smart & Smart, 2006, pp. 12-13). Social or Minority Model The most progressive and disability affirmative model. The “problem” is disability stereotypes and prejudice. Disability is the interaction of the social and physical environments (Lutz & Bowers, 2003). PwDs have the right to define their disability, their role in society, and the outcome of their lives. Depression and anxiety can, but does not always, occur as a result of disability, but rather as a result of disability stereotypes, prejudice, and discrimination (Hahn, 1997). TED Talk: Stella Young and “Inspiration” http://youtu.be/8K9Gg164Bsw Aimee Mullins TED Talk: Social Model Clip: http://youtu.be/mWkdyMg-_Fk Disability Stigma Disability is a central characteristic. Beliefs about disability can “spread” to describe other characteristics, positively or negatively. Disability hierarchy: acquired disabilities are more socially accepted than congenital or lifelong ones. Some have theorized that disabilities that affect communication are less accepted than those that do not Olkin, Rhoda. (1999). What psychotherapists should know about disability. New York: Guilford Press. Disability Stereotypes Admiration; inspiration; “supercrip” Pity, embarrassment, resentment toward PWDs. Perceived special privileges can lead to social isolation for PWDs (Yuker, 1994). Asexual Prescription of affect: Cheerfulness expected. Anger is often not permitted; may be seen as a symptom of a disorder, rather than as a result of oppression. Requirement of mourning: TABs expect depression Disability Stereotypes Visibility/Invisibility: The disability is visible; the PERSON (personality) is invisible. Chronic visibility can feel like an invasion of privacy. Invisibility can feel disrespectful and neglectful. Infantilization: The assumption that PwDs need soothing, need to be protected, and cannot make informed decisions. Olkin, Rhoda. (1999). What psychotherapists should know about disability. New York: Guilford Press. Disability Stereotypes Parentification of children of Parents with Disabilities: Parents with disabilities are often extremely cautious NOT to rely on their children for caregiving. Olkin, Rhoda. (1999). What psychotherapists should know about disability. New York: Guilford Press. Clinical Implications General Considerations Assessment Diagnosis Case Conceptualization Interventions General Considerations Awareness about personal beliefs about and reactions to various disabilities. More likely to engage with providers from other disciplines. Consider office accessibility and scheduling to allow for “crip time.” Tone of voice and language: person-first language vs. disability identity language. Practitioners should use person-first language, unless given permission by PwD to use disability identity language. Clinical Implications: Assessment Assessment: Asking about disability, even if not visible. Assessing presenting problem Assess perceived social support; not necessarily actual support. Asses the disability model(s) to inform case conceptualization and intervention (See “Questions to Assess Disability Model” Handout). Asking About Disability Does the PWD identify as having a disability? What messages has he/she received from society/family? Ask the PwD about his/ her disability. “What is the nature of your disability? How does it affect you in your daily life?” Failure to conform to/internalize stereotypes is not necessarily denial of disability status. (Use your clinical judgment here). Olkin, Rhoda. (1999). What psychotherapists should know about disability. New York: Guilford Press. Clinical Implications: Diagnosis How might a particular model of disability inform the presenting problem? Higher levels of anxiety following acute disability onset; can look like a panic disorder, etc. Anger expressed toward discrimination/oppression should not be over-pathologized. Over/underreporting symptoms of depression. Do not attribute symptoms of depression directly to a medical diagnosis or disability. Lifetime of self-advocacy can result in what appears to be grandiosity/narcissism Case Conceptualization Frameworks to Consider: Social Model of Disability Disability culture and biculturalism of PwDs. Family Systems Theories Disability as a social construct Presume competence first. Disability may or may NOT be part of treatment. Olkin, Rhoda. (1999). What psychotherapists should know about disability. New York: Guilford Press. (pp. 154-5). Clinical Implications: Intervention Consider traditional treatment interventions, but also: Focus on validating experiences of oppression, NOT reinforcing stereotypes and stigma. Empower the PwD by emphasizing personhood, resiliency, and abilities. Treatment goals should center around PwDs personal values, and ideally, move them “through” disability models to integrate disability identity. Contain disability “spread” effect; intrinsic values become more salient. Handout: Case Example Mr. J. is a an 68-year-old, Caucasian male who is a very experienced military and civilian pilot. A few years ago, he and his co-pilot survived a plane crash. His co-pilot has, for the most part, fully recovered. He even recently got a tattoo reading, “In the arms of God,” to memorialize his survival of the crash. Mr. J., however, sustained a complete spinal cord injury, such that he now has quadriplegia, and requires around-the-clock care. He and his wife are able to afford quality in-home care most days of the week. Mr. J ambulates via motorized wheelchair. He utilizes a ventilator to breathe, but the machine renders his speech inaudible. With his consent, you have been asked by his primary care provider to assist him in adjusting to his disability. Mr. J. admits that he feels very depressed most of the time. He is currently prescribed sertraline (Zoloft) with some perceived positive benefit. Mr. J. reflects on his accident often. He says, “I thought I was a better pilot than that.” His wife and children, however, have expressed their gratitude that Mr. J. is still alive. Mr. J. is in the process of writing his memoir, but his assistive typing technology is unreliable, and produces multiple typing errors, such that he becomes frustrated and forgoes the task after a few sentences. Moreover, although he was recently fitted with a new wheelchair, the cushions have caused pressure ulcers on various parts of his body. His wife also suspects that he may be experiencing early signs and symptoms of C. diff ( a serious bacterial infection of the intestines). Mr. J. Discussion Questions What are some general considerations, logistically, that you should be aware of and/or plan for as Mr. J.’s psychologist? What feelings of countertransference do you have toward Mr. J.? Are there any particular questions you would like to ask Mr. J and his wife regarding his disability or other areas of clinical importance? Are there any questions you hesitate to ask? How would you define the presenting problem/problems? What would you address first? How might you involve other treatment providers, if possible? What are your treatment goals? How might your treatment plan be similar or different to that of able-bodied patients with depression? Can you tell which disability model Mr. J. or his wife subscribe to? If not, what additional information do you need? What questions might you ask? What about his co-pilot? Does he subscribe to a particular disability model? How might this be relevant to treatment? Questions/Comments? Contact Information: Erin N. Armour, Psy.D. erinnarmour@gmail.com References College committee for diversity, equity, and affirmative action. (2014). A booklet of interactive exercises to explore our differences. Retrieved October 1, 2015 from http://intraweb.stockton.edu/eyos/affirmative_action/content/docs/Interactive%20Div ersity%20Booklet%2010-14-2011.pdf Council for disability awareness. (2015). What’s your personal disability quotient? Retrieved October 25, 2015 form http://www.disabilitycanhappen.org/pdfs/Paper_PDQ.pdf Erickson, W., Lee, C., & von Schrader, S. (2014). 2012 Disability Status Report: United States. Ithaca, NY : Cornell University Employment and Disability Institute (EDI). Hahn, H. (1997). Advertising the acceptable employment image: Disability and capitalism. In L. J. Davis (Ed.), The disability studies reader (pp.172-186). New York: Routledge. Johnson, A. (2006). Privelege, power, and difference. (2nd ed). Boston: McGraw-Hill. Lutz, B. & Bowers, B. (2003). Understanding how disability is defined and conceptualized in the literature. Rehabilitation Nursing, 28, 74-78. Nosek, M. A., Foley, C. C., Hughes, R. B. & Howland, C. A. (2001). Vulnerabilities for abuse among women with disabilities. Sexuality and Disability, 19, 177-189. Olkin, Rhoda. (1999). What psychotherapists should know about disability. New York: Guilford Press. References Smart, J. F. & Smart, D. W. (2006). Models of disability: Implications for the counseling profession. Journal of Counseling and Development, 84, 29-40. Stoddard, S. (2014). 2014 Disability statistics annual report. Durham, NH. University of New Hampshire. Yuker, H. E. (1994). Variables that influence attitudes towards persons with disabilities: Conclusions from the data. Psychosocial Perspectives on Disability, A Special Issue of the Journal of Social Behavior and Personality, 9, 3-22.