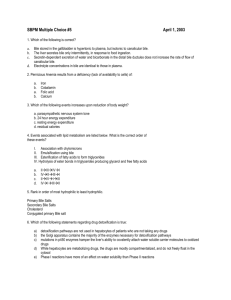
Physiology Ch 64 p773-788 [4-25
advertisement
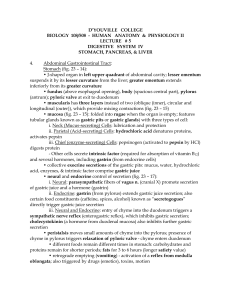
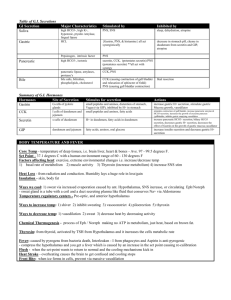
Physiology Ch 64 p773-788 Secretory Functions of the Alimentary Tract -Secretory glands serve two primary functions in the GI tract: 1. Digestive enzymes secreted between the mouth and the ileum 2. Mucus secretion for lubrication and protection of GI tract -Most secretions formed in precise amounts needed in response to amount of food -Some parts of the GI tract secrete specific enzymes in response to a particular type of food General principles of Alimentary Tract Secretion -Single cell mucous glands (mucous cells) line surface of the epithelium in most parts of the alimentary tract, look like goblets -extrude mucus directly onto epithelial surface as a lubricant in response to local irritation of epithelium and protects it from excoriation (abrasion) -Many surface areas of GI tract lined by pits in submucosa (crypts of Lieberkuhn in small intestine) -Stomach and upper duodenum contain large numbers of specialized tubular glands which act to secrete compounds like acid and pepsinogen (from oxyntic gland) -Several associated glands exist – salivary, pancreas, liver that provide secretions for digestion -salivary and pancreatic glands are compound acinous glands that secrete into series of ducts which empty into GI tract Mechanism of Stimulation of GI Glands – mechanical presence of food in a particular segment of GI tract causes glands of that region to secrete moderate to large amount of juices/mucus -Results (particularly mucus) from direct contact of gland cells by food -Local epithelial stimulation activates enteric nervous system of gut through tactile stimulation, chemicals, and distention, stimulating mucous cells on gut epithelial surface and deep glands of gut wall Autonomic Stimulation of Secretion – parasympathetic stimulation increases gland secretion. Salivary, esophageal, gastric, pancreas, and Brunner’s glands in duodenum (innervated by CN IX and X) in upper GI tract -Also pelvic parasympathetics innervating distal portion of large intestine -Secretion in rest of small intestine + large intestine is in response to local neural and hormonal stimuli -Sympathetic stimulation has a dual effect on GI gland secretion -Cause slight – moderate increase in local gland secretion -Cause vasoconstriction to vessels supplying glands -Therefore, if parasympathetics in play, sympathetics will decrease secretion due to vasoconstriction, but increase secretion if working alone Regulation of Secretion by Hormones – gastrointestinal hormones regulate volume and character of secretions. Hormones released from GI mucosa in response to food and absorbed into blood to be carried to glands particularly useful for gastric juice and pancreatic juice secretion -GI hormones are polypeptides Mechanism of Secretion by Glandular Cells 1. Organic Substances – a. Nutrient needed for formation of secretion diffuses by blood into base of gland. b. Mitochondria inside cell use oxidative energy to form ATP c. ATP + substrates from nutrients synthesizes secretory organics in ER and Golgi d. Secretions are transported through tubules of ER to golgi for modification and packaging e. Vesicles on apical side of cell are stored until nerve/hormonal signal causes Ca to influx, fusing vesicles with plasma membrane and releasing contents by exocytosis 2. Water and Electrolyte Secretion – we need H2O and electrolytes to be secreted with organics a. Secretion by salivary glands is an example of how nervous stimulation causes water and salts to pass through glandular cells in great profusion, washing organics through secretory border of cells at same time Lubricating and Protective Properties of Mucus – mucus is thick secretion composed of H2O, electrolytes, and glycoproteins -Different composition in various parts of GI, but still excellent lubricant -Properties of Mucus: 1. Adherent qualities that make it adhere to food and spread like film over the surface 2. Has sufficient body that it coats wall of gut and protects mucosa from physically touching food 3. Low resistance for slippage, so particles can slide along epithelium with ease 4. Causes fecal particles to adhere to one another to form feces for expulsion 5. Strongly resistant to digestive enzymes from GI tract 6. Glycoproteins of mucus have amphoteric properties (capable of buffering either acids or bases) a. Contains some bicarb to neutralize acids -person can become aware of lubricating quality if salivary glands fail to secrete saliva, hard to swallow Secretion of Saliva – Saliva contains a serous secretion and a mucus secretion -Glands involved in salivation are parotid gland, submandibular and sublingual glands, tiny buccal glands -Daily saliva ranges between 800-1500mL -Two types of protein secretion: 1. Serous Secretion containing ptyalin (alpha-amylase) – works at pH between 6.0 and 7.0 2. Mucus Secretion containing mucin for lubrication -Parotid glands secrete serous secretions almost entirely -Submandibular and sublingual glands secrete both serous and mucus -Buccal glands only secrete mucus Secretion of Ions in Saliva – saliva contains K+ and bicarb, and less Na and Cl. -Submandibular gland is a compound gland with acini and salivary ducts, and secretion is in 2 steps 1. First stage involves a primary secretion by acini that contains ptyalin and/mucin in ion solution a. As primary secretion flows through ducts, two major active transport processes happen i. Na+ ions actively reabsorbed from all salivary ducts and K+ ions secreted ii. Bicarb ions secreted by ductal epithelium into lumen of duct by passive exchange of bicarb for Cl2. During Maximal Salivation, salivary ionic concentrations change dramatically because rate of formation of primary secretion by acini can increase 20-fold Function of Saliva for Oral Hygiene – some saliva of mucus type is secreted every minute but stops during sleep. Mouth is loaded with pathogenic bacteria that cause damage that saliva helps prevent -Flow of saliva helps wash away pathogenic bacteria as well as food -Saliva contains factors to destroy bacteria, such as thiocyanate and proteolytic enzymes (lysozyme) that attack bacteria, help thiocyanate to enter bacteria and kill it, digest food particles -Saliva contains antibodies to destroy oral bacteria, including those that cause dental caries -Without salivation, oral tissues become ulcerated and infected Nervous Regulation of Salivary Secretion – salivary glands are controlled by parasympathetic nervous signals all the way from superior and inferior salivatory nuclei in brain stem -Excited by taste and tactile stimuli from tongue and other areas of mouth and pharynx -Many tastes, especially sour (caused by acids) elicit large secretion of saliva -Can also be stimulated or inhibited by nervous signals from higher CNS, such as when person smells or eats favorite foods as opposed to when someone eats disliked food -Salivation also occurs in response to reflexes originating in stomach and small intestine when irritating foods are swallowed or during nausea because of GI abnormality -The saliva helps remove irritant by diluting or neutralizing irritant substances -Sympathetic stimulation can increase salivation slightly from superior cervical ganglia -Blood supply to glands affects salivary secretion because glands require nutrients to produce saliva -Parasympathetic nerve that stimulates salivation also dilates blood vessels -Kallikrein – secreted by active salivary glands acts to split blood protein α2-globulin to bradykinin, a vasodilator Esophageal Secretion – entirely mucus and provide lubrication for swallowing -Esophagus lined with simple mucous glands, and compound ones exist near stomach (to protect from gastric juice reflux) Gastric Secretions – in addition to mucous glands, stomach also has tubular glands Oxyntic Glands and Pyloric Glands. -Oxyntic produce HCl, pepsinogen, intrinsic factor, and mucus (inside of body and fundus of stomach) -Pyloric glands secrete gastrin and mucus to protect pyloric mucosa from stomach acids Oxyntic Gland Secretion – gland is composed of 3 cell types: 1. Mucous Neck cells – secrete mainly mucus 2. Peptic (chief) cells – secrete pepsinogen 3. Parietal (oxyntic) cells – secrete intrinsic factor and HCl -Parietal cells can secrete HCl at 160mmol/L and pH of 0.8, 3 million times higher than arterial blood -At the same time that H+ is secreted, HCO3 diffuses into blood so gastric venous blood has higher pH than arterial blood when stomach is secreting acid -The parietal cell (oxyntic cell) contains large branching (canaliculi) and HCl is formed in villi around it -Main driving force for HCl secretion is hydrogen-potassium pump (an ATPase) -Steps of HCl Synthesis: 1. H2O in cell dissociates into H+/OH-, H+ is secreted into canaliculus in exchange for K+ catalyzed by H+/K+ ATPase (on the apical side). a. On the basal side, K+ transported back into cell by Na/K ATPase, which creates low intracellular Na, contributing to Na reabsorption form lumen of canaliculus 2. Pumping of H+ out of cell by pump permits OH- to accumulate and form HCO3 from CO2 during metabolism, catalyzed by carbonic anhydrase enzyme. HCO3 transported across basal surface in exchange for Cl- ions, which enter the cell and pass through to the apical side canaliculus through chloride channels 3. H2O passes into canaliculus by osmosis since extra ions are secreted into it -Ability of stomach to prevent HCl leaking back is the gastric barrier due to formation of basic mucus and tight junctions on epithelium. Damage to barrier can cause leaking and damage to stomach mucosa Factors Stimulating Gastric Secretion – acetylcholine, gastrin, and histamine -Acetylcholine released by parasympathetic stimulation excites pepsinogen by peptic cells, HCl by parietal cells, and nucus by mucus cells -Gastrin and histamine strongly stimulate acid by parietal cells but do not affect other cells -Several types of pepsinogen are secreted by peptic and mucus cells -No digestive activity until it comes in contact with HCl, when it is activated to form pepsin -Pepsin functions as a proteolytic enzyme in low pH medium Intrinsic Factor is necessary for absorption of vitamin B12 in the ileum, and is secreted by parietal cells with HCl -If acid cells of stomach are destroyed, person develops achlorhydria (lack of stomach acid) and pernicious anemia (failure of red blood cells to mature due to lack of vitamin B12) Pyloric Glands – Secretion of Mucus and Gastrin – similar to oxyntic glandsbut contain few peptic cells and no parietal cells. -Mostly mucus cells that help lubricate environement, small amount of pepsinogen -Secrete Gastrin which plays a role in gastric secretion Surface Mucous cells – entire surface of stomach mucosa between glands has continuous layer of mucous cells that secrete large amounts of Viscid Mucus – coats stomach mucosa protecting stomach -Mucous is alkaline so that stomach wall is not exposed to stomach acid -Slightest contact with food or irritation stimulates surface mucus cells Stimulation of Gastric Acid Secretion – parietal cells are the only cells secreting HCl, under control by nervous system and hormones -Function in close association with enterochromaffin-like cells (ECL Cells), which secrete histamine -ECL cells lie in deep recesses of oxyntic glands, directly regulate rate of HCl secretion by parietal cells, and ECL cells are stimulated to secrete histamine by Gastrin formed in antral portion of stomach. -ECL cells may also be stimulated by enteric nervous system Stimulation of Acid Secretion by Gastrin – gastrin is a hormone secreted by gastrin cells (G cells) in pyloric glands in distal stomach. Heterodimer with smaller (G-17) monomer more abundant 1. Meats or protein-foods reach antrum and stimulate gastrin cells to release gastrin into blood 2. Gastrin transported to ECL causing release of histamine directly into oxyntic glands, stimulating HCl secretion Regulation of Pepsinogen Secretion – pepsinogen is secreted from peptic cells in oxyntic glands in response to 2 signals: 1. Stimulation by acetylcholine released from vagus nerves or gastric enteric nervous system 2. Stimulation of peptic cell secretion in response to acid in the stomach a. Acid indirectly elicits enteric nervous system reflexes, influencing pepsinogen secretion Phases of Gastric Secretion – Occurs in 3 phases 1. Cephalic Phase – while food is being eaten before entering stomach, results from sight, smell, thought, or taste. Originating in cerebral cortex in appetite centers in amygdala and hypothalamus. Transmitted through dorsal motor nuclei of vagus nerves – 30% of secretion 2. Gastric Phase – Once food enters stomach, excites long vagovagal reflexes from stomach to brain and back, local enteric reflexes, and the gastrin mechanism to secrete gastric juices and accounts for 60% of secretion 3. Intestinal Phase – presence of food in upper duodenum will cause stomach to secrete gastric juice due to small amounts of gastrin released by duodenal mucosa accounting for 10% of secretion Inhibition of Gastric Secretion – intestinal chyme can slightly increase gastric secretion and also decrease it at other times. Inhibition results from 2 influences 1. Reverse enterogastric reflex transmitted through myenteric nervous system and extrinsic sympathetic and vagus nerves to inhibit stomach secretion a. Triggered through distention, acid in intestine, protein breakdown products, or irritation 2. Presence of fat, acid, protein, hyper/hyposmotic fluids releases hormones such as secretin, gastric inhibitory peptide, vasoactive intestinal polypeptide, and somatostatin to inhibit gastric secretions -inhibition exists to slow passage of chyme into small intestine when intestine is already filled -emotional stimuli can increase secretion of gastric acid Chemical Composition of Gastrin and other GI Hormones -CCK, gastrin, and secretin are large polypeptides with some similarities. -Gastrin’s functional AA are terminal 4 amino acids -CCK’s functional AA are terminal 8 amino acids -All secretin amino acids are essential -Pentagastrin is a synthetic gastrin composed of terminal 4 amino acids + alanine, same properties Pancreatic Secretion – pancreatic enzymes secreted by pancreatic acini, and lots of HCO3 secreted by small ductules from acini. Enzymes and HCO3 flow through pancreatic duct and into duodenum through papilla of Vater, surrounded by sphincter of Oddi. -secreted mainly in response to chyme in duodenum, and pancreatic juice varies based on food Pancreatic Digestive Enzymes – pancreas secretes enzymes digesting proteins, carbs, and fats as well as bicarb ions to neutralize acid in intestine -Trypsin, chymotrypsin, carboxypeptidase secreted by pancrease – trypsin is most abundant -Trypsin/chymotrypsin split proteins into peptides, and carboxypeptidase splits into individual AA -Pancreatic Amylase digests starches, glycogen, and most other carbs to form disaccharides -Pancreatic Lipase hydrolyzes fat into fatty acids and monoglycerides -Cholesterol Esterase – hydrolysis of cholesterol esters -Phospholipase splits fatty acids from phospholipids -Proteolytic enzymes secreted are non-functional at first in the form of trypsinogen, chymotrypsinogen, and procarboxypolypeptidase -Trypsinogen activated by enterokinase secreted by intestinal mucosa in response to chyme -can also be autocatalytically activated by trypsin -Chymotrypsinogen and procarboxypolypeptidase activated by trypsin Secretion of Trypsin Inhibitor Prevents Digestion of Pancreas Itself – proteolytic enzymes of pancreatic juice shouldn’t activate until reaching duodenum because they can digest pancreas. -Trypsin inhibitor is secreted by pancreatic cells that also secrete the proteolytic enzymes to prevent activation of trypsin both inside secretory cells and in acini and ducts. -If pancreas is damaged and duct is blocked, pancreatic secretion overwhelms trypsin inhibitor and the proteins digest the pancreas in a few hours resulting in Acute Pancreatitis Secretion of Bicarbonate Ions – secreted by epithelial cells of ductules that lead from acini, making pancreatic juice alkaline to neutralize HCl Mechanism for secretion of NaHCO3: 1. CO2 diffuses into to interior of cell from blood and combines with H2O using carbonic anhydrase to form H2CO3, which dissociates into HCO3 and H+. HCO3 is actively transported in association with Na ions through apical border of cell into lumen 2. H+ ions formed by dissociation of carbonic acid are exchangd for Na ions thorugh blood border by active transport. This supplied the Na ions transported through luminal border into pancreatic duct to provide neutrality for secreted bicarb 3. Overall movement of Na and HCO3 from blood into duct lumen creates osmotic pressure that causes osmosis of H2O also into duct forming isosmotic HCO3 solution Regulation of Pancreatic Secretion 1. Acetylcholine – released from parasymp. Vagus nerve endings and from cholinergic nerves of enteric nervous system 2. CCK – secreted by duodenal and upper jejunal mucosa when food enters 3. Secretin – secreted by duodenal and jejunal mucosa when acidic food enters -Ach and CCK stimulate acinar cells for digestive enzymes, secretin stimulates HCO3 and H2O secretion -When all stimuli affect pancreas, total secretion is greater than each one separately, therefore stimuli multiple and potentiate Phases of Pancreatic Secretion 1. Cephalic Phase – cause Ach from vagal nerve endings in pancreas releases 20% of enzymes 2. Gastric Phase – nerve stimulation continues- 5-10% of enzymes, little fluid, same with cephalic 3. Intestinal Phase – after chyme leaves stomach, pancreatic secretion is increased by secretin a. Secretin – stimulates HCO3 ions to neutralize chyme released by S cells from duodenum, results from acid chyme with pH 4-5 entering duodenum i. Absorbed into blood, only HCl in chyme stimulates its release ii. Causes this reaction in duodenum HCl + NaHCO3 NaCl + H2CO3 iii. Carbonic acid dissociates into CO2 and H2O -Pancreatic enzymes work at pH 7-8, which is what bicarb does in duodenum Cholecystokinin – released from presence of food in upper duodenum causes CCK release from I cells in duodenum and jejunum, especially from presence of proteases and peptones (peptide digestion) and long-chain fatty acids -passes by blood to pancreas but only causes secretion of enzymes from acinar cells accounting for 7080% of enzyme secretion Secretion of Bile by the Liver – liver secretes bile, almost 1L/day, and has 2 functions: 1. Fat digestion and absorption due to bile acids which emulsify fats to be attacked by lipases, and absorption of digested fat through intestinal mucosa 2. Bile serves as a means of excretion of waste products from blood, include bilirubin which is an end-product of hemoglobin destruction and excesses of cholesterol -bile secreted by hepatocytes containing bile acids, cholesterol, and organics into bile canaliculi -bile flows toward interlobular septa, where it empties into terminal bile ducts hepatic duct common bile duct -bile can then enter duodenum directly or get stored in the gallbladder via the cystic duct -Na and HCO3 ions from liver added to bile as it travels through ducts stimulated by secretin Storing and Concentrating Bile in Gallbladder – Bile secreted continually by liver, but most is stored in gallbladder until needed (12 hours of bile secretion can be stored) -H2O, Na, Cl, and small electrolytes can be absorbed through gallbladder mucosa to concentrate bile salts, cholesterol, lecithin, and bilirubin -Gallbladder absorption is caused by active transport of Na through epithelium followed by secondary absorption of Cl, H2O. Composition of Bile: H2O, Bile salts, bilirubin, cholesterol, fatty acids, lecithin, Na, K, Ca, Cl, HCO3 Emptying of Gallbladder – gallbladder begins to empty as soon as food begins being digested in upper GI tract, especially when fatty foods reach duodenum 30 minutes after a meals -Rhythmic contractions of gallbladder wall with simultaneous relaxation of sphincter of Oddi causes emptying -CCK is most potent stimulus for gallbladder contractions, stimulated by fatty foods entering duodenum -Also stimulates by Ach-secreting nerves from vagi and enteric nervous systems -When fat is not in food, gallbladder poorly empties Function of Bile Salts in Fat Digestion and Absorption – cholesterol ingested or synthesized by liver is the precursor to bile salts -Cholesterol cholic acid chenodeoxycholic acid combine with glycine to form glyco- and tauroconjugated bile acids. Salts from these acids, mainly sodium salts are secreted in bile -Two important functions: 1. Detergent action on fat particles in food, decreases surface tension and allows intenstinal tract to break fat into small sizes (called emulsifying) 2. Help absorb fatty acids, monoglycerides, cholesterol, and other lipids from intestines by forming small physical complexes with lipids called micelles; lipids use these to get ferried to intestinal mucosa to be absorbed in the blood a. Without bile salts, 40% of the fat is secreted in feces and develops deficiency Enterohepatic Circulation of Bile Salts – 94% of bile salts reabsorbed into blood from small intestine, by diffusion and active transport in intestinal mucosa and ileum, entering portal blood and back to liver. The pass through venous sinusoids and absorbed back into hepatocytes and resecreted as bile. -recirculation of bile is called enterohepatic circulation -daily rate of bile secretion is controlled by availability of bile salts in enterohepatic circulation -Secretin, the hormone that stimulates pancreatic HCO3 secretion, also stimulates bile secretion, sometimes doubling after a meal (secretes HCO3 from bile ductules and ducts) Liver Secretion of Cholesterol and Gallstone Formation – cholesterol is insoluble in pure water unless combined with bile salts and lecithin to form micelles. When bile becomes concentrated in gallbladder, bile salts and lecithin become concentrated with cholesterol, keeping cholesterol in solution -cholesterol may precipitate in gallbladder under abnormal conditions forming cholesterol gallstones -amount of cholesterol in bile related to how much fat a person eats because liver synthesizes bile based on fat intake -people on high-fat diet may develop gallstones for this reason -inflammation of gallbladder from chronic infection changes absorptive properties of gallbladder, sometimes exceeding absorption of water and leaving cholesterol, precipitating to crystals Secretions of the Small Intestine – Brunner’s glands in the wall of the duodenum between pylorus and papilla of Vater secrete alkaline mucus in response to tactile or irritating stimuli on duodenal mucosa, vagal stimulation, or GI hormones such as secretin -function of the mucus is to protect wall of duodenum from acidic gastric juice emptying from stomach, also has excess bicarb to neutralize HCl -Brunner’s glands inhibited by sympathetic stimulation, which can cause peptic ulcers in excitable people in this area in 50% of ulcer patients Secretion of Intestinal Digestive Juices by Crypts of Lieberkuhn – crypts lie between the villi and are composed of goblet cells that secrete mucus and enterocytes which secrete H2O and electrolytes and reabsorb them -intestinal secretions formed by enterocytes at 2L/day and alkaline pH 7.5-8 -primary function of small intestine is to absorb nutrients into the blood -secretion of the watery fluid happens by active secretion of Cl into crypts and active secretion of HCO3, movement of all these ions cause osmotic movement of H2O as well Digestive Enzymes in Small Intestine – enterocytes of mucosa covering villi have digestive enzymes that digest food while they are being absorbed through epithelium -peptidases for splitting small peptides into amino acids -sucrase, maltase, isomaltase, and lactase for splitting disaccharides into monosaccharides -intestinal lipase for splitting neutral fats into glycerol and fatty acids -epithelial cells in base of crypts undergo mitosis and push epithelium toward villi (rapid 5 day repair) -Regulation of small intestine secretion is through local enteric reflexes from tactile/irritative stimuli Secretion of Mucus by Large Intestine – mucosa of large intestine has crypts of Lieberkuhn but no villi. Secrete no digestive enzymes, and secrete only mucus with some HCO3 ions by non-mucus secreting epithelial cells. -Regulated by local enteric reflexes from tactile, direct stimulation -Stimulation of pelvic nerves from spinal cord carrying parasympathetic innervation to distal 2/3rds of colon can cause increase in mucus secretion -occurs with peristaltic motility of colon -During extreme parasymp. Stimulation during emotional disturbances, so much mucus can be secreted that person has bowel movement every 30 minutes -Mucus in large intestine protects intestinal wall against excoriation and provides adherent medium for holding fecal matter together -Protects against bacterial activity taking place in feces Diarrhea Caused by Excess Secretion of H2O and Electrolytes in Response to Irritation – when large intestine becomes irritated (bacterial infection or enteritis), mucosa secretes lots of H2O and electrolytes in addition to alkaline mucus, diluting irritating factors and cause rapid movement of feces toward anus. -Results in diarrhea with large loss of H2O, promoting earlier recovery of disease