Introduction to Microbiology
advertisement

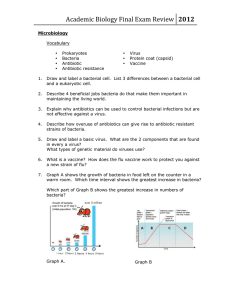
Introduction to Microbiology I. OVERVIEW • Microorganisms are everywhere • Associate with other multicellular organisms • Normal flora Initiation of disease • Pathogens Spread • Most infectious diseases is initiated by colonization • Proliferating on the mucus membrane / skin Major exceptions Directly to blood / internal organs • Microbial Colonization may result Elimination Immunity Infection Disease Figure 1. Some possible outcomes following exposure to microorganisms. II. PROKARYOTIC PATHOGENS • Bacteria Prokaryotic eubacteria • Prokaryotic Organisms archaebacteria Figure 2. Comparison of prokaryotic and eukaryotic cells. 1Some bacteria have more than one circular molecule as their genome. Vibrios, for example, have two circular chromosomes. Borrellia have linear chromosomes and a wide array of different sized plasmids. Rigid cell wall surrounding the cell membrane Gram positive (+ve) or gram negative (-ve) Flagella, pili, and/or a capsule Binary fission division Plasmids A Gram stain of mixed Staphylococcus aureus (Staphylococcus aureus ATCC 25923, Gram positive cocci, in purple) and Escherichia coli (Escherichia coli ATCC 11775, Gram negative bacilli, in red), the most common Gram stain reference bacteria A. Typical bacteria Bacteria shapes Prokaryotic cells < eukaryotic cells Bacterial cellular morphologies Figure 4. Bacterial morphology diagram B. Atypical bacteria Mycoplasma, Chlamydia, and Rickettsia Prokaryotic Characteristic structural components or metabolic capabilities Figure 5. Rickettsia rickettsii III. FUNGI Nonphotosynthetic, generally saprophytic, eukaryotic Molds and yeasts Sexual reproduction , asexual, or both All fungi produce spores Pathogenic fungi diseases Figure 6. Fungi collage IV. PROTOZOA Single-celled, nonphotosynthetic, eukaryotic Various shapes and sizes Many are free living, but others are among the most clinically important parasites Infect all major tissues and organs Intracellular parasites Extracellular Blood Urogenital region Intestine Ingestion of an infective stage of the parasite or by insect bite Protozoa cause a variety of diseases Figure 7. Giardia lamblia V. HELMINTHS Groups of parasitic worms Multicellular, eukaryotic organisms with complex body organization 3 main groups: tapeworms (cestodes) flukes (trematodes) roundworms (nematodes) Receiving nutrients by ingesting or absorbing digestive contents or body fluids or tissues Almost any organ in the body can be parasitized Figure 8. Ascaris lumbricoides VI. VIRUSES Obligate intracellular parasites that do not have a cellular structure DNA virus or RNA virus, surrounded by a protein coat May also have an envelope Contain genetic info for replication but require the host’s cellular structures and enzymatic machinery The fate of the host cell following viral infection varies Figure 9. EM of influenza virus Normal Flora I. OVERVIEW Our bodies are continuously inhabited by many different microorganisms They are harmless and may even be beneficial Microorganisms are termed “normal flora” They are also termed commensals The internal organs and systems are sterile Newborn are rapidly acquires normal flora Food Environment Other humans II. DISTRIBUTION OF NORMAL FLORA IN THE BODY Most common sites inhabited by normal flora A. Skin B. Eye C. Mouth and nose D. Intestinal tract E. Urogenital tract A. Skin Can acquire any bacteria in the immediate environment Transient flora either dies or is removable by washing Skin supports a permanent bacterial population Resident flora resides in multiple layers of the skin The resident flora regenerate even after vigorous scrubbing Staphylococcus epidermidis account for 90% of the skin aerobes Anaerobic organisms, such as Propionibacterium acnes, reside in deeper skin layers hair follicles sweat and sebaceous glands Sometimes, skin inhabitants resulting in serious bloodstream infections B. Eye The conjunctiva of the eye is colonized primarily by S. epidermidis S. aureus Aerobic corynebacteria (diphtheroids) Streptococcus pneumoniae Organisms that normally inhabit the skin are present but at a lower frequency Tears lysozyme, help limit the bacterial population of the conjunctiva C. Mouth and nose Harbor many microorganisms, both aerobic and anaerobic Among the most common are Corynebacterium diphtheroids Staphylococcus aureus Staphylococcus epidermidis Teeth and surrounding gingival tissue are colonized by their own particular species Streptococcus mutans S. mutans can lead to potentially fatal infective endocarditis Some normal residents of the nasopharynx can also cause disease S. pneumoniae, can cause acute bacterial pneumonia Pneumonia is frequently preceded by an upper or middle respiratory viral infection D. Intestinal tract Density of microorganisms in the stomach is relatively low ( 103 - 105 / gram of contents) Gastric enzymes Acidic pH The density of organisms increases along the alimentary canal 108 to 1010 bacteria per gram of contents in the ileum 1011 per gram in large intestine 20% of the fecal mass consists of different species of bacteria More than 99% of which are anaerobes Bacteroides sp. constitute a significant percentage of bacteria in the large intestine Escherichia coli, constitutes less than 0.1 percent of the total population of bacteria in the intestinal tract However, this endogenous E. coli is a major cause of urinary tract infections E. Urogenital tract Vagina low pH is maintained by Lactobacillus species Decreased in Lactobacillus population pH rises potential pathogens can overgrow Candida albicans Urine is sterile but can become contaminated in the lower urethra III. BENEFICIAL FUNCTIONS OF NORMAL FLORA Provide some definite benefits to the host The sheer number of harmless bacteria in the lower bowel and mouth Some bacteria of the bowel produce antimicrobial substances A powerful stimulus for the development of the immune system Provide important nutrients, and aid in digestion and absorption of nutrients IV. HARMFUL EFFECTS OF NORMAL FLORA Clinical problems caused by normal flora 1) The organisms are displaced from their normal site 2) Potential pathogens gain a competitive advantage 3) Harmless, commonly ingested food substances are converted into carcinogenic derivatives 4) Normal flora can overgrow and become pathogenic Pathogenicity of Microorganisms I. OVERVIEW A pathogenic microorganism is capable of causing disease Some microorganisms are unequivocally pathogenic An organism may invade an individual without causing infectious disease Can be recognized by the presence of antibody Some infections result in a latent state Some pathogens cause disease only under certain conditions Terms used to describe infections The methods by which bacteria cause disease 1) entry into the host 2) adhesion to host cells 3) propagation of the organism 4) damage to host cells 5) evasion of host secondary defenses Microorganism pathogenicity depends on its success in completing some or all The terms “virulence” and “pathogenicity” are often used interchangeably Figure 3.1 ID50 (I = infectious, D = dose) versus LD50 (L = lethal, D = dose). II. BACTERIAL PATHOGENESIS A. Virulence factors Characteristics that enhance pathogenicity enable a microorganism to establish itself replicate on or within a specific host Some of the more important steps in the infectious process are reviewed next 1. Entry into the host Overcome host defenses before it can establish itself Phagocytosis Stomach acidity Urogenital tract Bacteria that have an outer polysaccharide capsule have a better chance of surviving Streptococcus pneumoniae Neisseria meningitidis 2. Adherence to host cells Some bacteria use pili to adhere to the surface of host cells Escherichia coli Group A streptococci Cell surface adhesion molecules or particularly hydrophobic cell walls Adherence enhances virulence allows each attached bacterial cell to form a microcolony A striking example of the importance of adhesion Neisseria gonorrhoeae strains that lack pili are not pathogenic 3. Invasiveness Invasive bacteria enter host cells penetrate mucosal surfaces spreading from the initial site of infection Invasiveness is facilitated by several bacterial enzymes Collagenase Hyaluronidase These enzymes degrade components of the extracellular matrix, providing the bacteria with easier access to host cell surfaces. Invasion is followed by inflammation Pyogenic Granulomatous The pus of pyogenic inflammations contains mostly neutrophils; Whereas granulomatous lesions contain fibroblasts, lymphocytes, and macrophages 4. Bacterial toxins Some bacteria cause disease by producing toxins Exotoxins Proteins Secreted by both G+ and G- bacteria Endotoxins Lipopolysaccharides Not secreted Integral components of the cell walls of G- bacteria a. Exotoxins These include some of the most poisonous substances known Exotoxin proteins generally have two polypeptide components Diphtheria toxin is an enzyme that blocks protein synthesis Most exotoxins are rapidly inactivated by moderate heating (60°C) Binding the protein to the host cell Responsible for the toxic effect In several cases, the precise target for the toxin has been identified 1µg of tetanus exotoxin can kill an adult human Staphylococcal enterotoxin E. coli heat-stable toxin Dilute formaldehyde Destroys the toxic activity of most exotoxins Does not affect their antigenicity Formaldehyde-inactivated toxins (toxoids) are useful in preparing vaccines Exotoxin proteins are, in many cases, encoded by genes carried on plasmids or temperate bacteriophages b. Endotoxins Heat-stable, lipopolysaccharide (LPS) components of the outer membranes of G- bacteria They are released into the host's circulation following bacterial cell lysis The main physiologic effects of LPS endotoxins are 1- Fever 3- Hypotension 2- Shock 4- Thrombosis Septic Shock These effects are produced indirectly by 1- activation of macrophages 3- activation of complement 2- with the release of cytokines 4- activation of the coagulation cascade Death can result from multiple organ failure G+ bacteria cell wall peptidoglycan can elicit a shock syndrome similar to that caused by LPS but usually not as severe Elimination of the causative bacteria by antibiotics can initially exacerbate the symptoms by causing sudden massive release of endotoxin into the circulation B. Antigenic switching A successful pathogen must evade the host's immune system An evasive strategy for the pathogen is to change its surface antigens This is accomplished by several mechanisms Phase variation Antigenic variation In this manner, the expressed surface antigen can assume many different antigenic structures C. Which is the pathogen? If a particular microorganism is isolated from infected tissue, one cannot conclude that the isolated organism caused the lesion The organism could, for example, be a harmless member of the normal skin flora that happened to be in the vicinity Alternatively, the organism may not be a natural resident of the skin, but an opportunistic pathogen that secondarily infected the necrotic lesion Opportunistic pathogen unable to cause disease in healthy, immunocompetent individuals can infect people whose defenses have been impaired A nineteenth century German microbiologist, Robert Koch, recognized this dilemma, and defined a series of criteria (Koch's postulates) by which the identity of the causative microbial agent of a disease can be confirmed Whereas this protocol has been successful in establishing the etiology of most infections, it fails if the causative organism cannot be cultured in vitro D. Infections in human populations Bacterial diseases may be communicable from person-to-person OR noncommunicable Cholera is highly communicable Botulism is noncommunicable When an epidemic becomes worldwide, it is called a pandemic Pandemics, such as the 1918 influenza pandemic human population has never been exposed to has no immunity against, the specific strain of influenza virus III. Viral Pathogenesis Viruses can replicate ONLY inside living cells First pathogenic manifestations of viral infection are seen at the cellular level Following initial exposure to some viruses Rapid onset of observable symptoms (acute infection) Mild Asymptomatic Following the initial infection Cleared completely from the body by the immune system For some viruses the initial infection is followed by Persistent infection Latent infection A. Viral pathogenesis at the cellular level Different responses to viral infection Cell type Virus Many viral infections cause no apparent morphologic functional changes When changes do occur, several responses can be recognized 1. Cell death A cell can be directly killed by the virus Inhibition of synthesis of cellular DNA, RNA, Protein Specific genes responsible for this inhibition Dead or dying cells release a brood of progeny viruses Repeat the replication process Adenovirus Poliovirus 2. Transformation Some viruses transform normal cells into malignant cells Transformation is an irreversible genetic process Integration of viral DNA into the host's DNA 3. Cell fusion Infection of cells with certain viruses Fuse producing giant multinucleate cells Viruses with this property include Herpesviruses Paramyxoviruses Virus-induced changes in the structure of the cell membrane 4. Cytopathic effect (CPE) CPE refers to any visible change in appearance of an infected cell Cell rounding Patches of stainable viral proteins Cell disintegration B. Initial infections The viral infection may remain localized or become disseminated The infection may be asymptomatic (unapparent) Typical symptoms of disease may occur 1) early symptoms at the primary site of infection 2) delayed symptoms dissemination from the primary site, causing infection of secondary sites Virus transmission can occur before symptoms are apparent making it difficult to control the spread 1. Routes of entry and dissemination to secondary sites Common routes by which viruses enter the body Skin Respiratory tract GI tract Urogenital tract Some viruses remain localized cause disease that is largely restricted to the primary site of infection Other viruses undergo multiplication in cells at the primary site which may be accompanied by symptoms followed by invasion of the lymphatic system and the blood The presence of virus in the blood is termed viremia Virus is disseminated throughout the body Can infect cells at secondary sites characteristic causing the disease typically associated with that species 2. Typical secondary sites of localization Secondary sites of infection determine the nature of the delayed symptoms Usually the major characteristics associated with the resulting disease Viruses frequently exhibit tropism for specific cell types and tissues This specificity is usually caused by the presence of specific host cell surface receptors recognized by particular viruses Whereas any tissue or organ system is a potential target for virus infection, the fetus represents an important site for secondary localization of virus infections Virus from the maternal circulation infects cells of the placenta, thereby gaining access to the fetal circulation, and ultimately to all tissues of the developing fetus Fetal death or developmental abnormalities are often the result Neonatal infection can also occur during birth when the fetus comes in contact with infected genital secretions of the mother or breast-feeds 3. Virus shedding and mode of transmission The mode of transmission of a viral disease is largely determined by Tissues that produce progeny virus • And/Or Fluids into which they are released These are not necessarily the secondary sites of infection Tissues commonly involved in viral shedding Skin Respiratory tract GI tract Bodily fluids 4. Factors involved in termination of acute infection In a typical, uncomplicated, acute infection Virus is totally eliminated from the host in 2 to 3 weeks This outcome is primarily a function of the host's immune system Cell-mediated Humoral responses The relative importance of these two responses depends on Virus Nature of the disease a. Cell-mediated responses The earliest immune system responses to virus infection generalized inflammatory response nonspecific killing of infected cells by natural killer cells This latter activity begins well before the virus-specific immune response Enhanced by interferon and other cytokines,. Later, cytolysis by virus-specific cytotoxic T lymphocytes that recognize virus peptides displayed on the cell surface also eliminates infected cells. These cellular responses are especially significant in that they help limit the spread of the infection by killing infected cells before they have released progeny virus. Cell surface immunodeterminants recognized by T cells are often derived from nonstructural or internal proteins of the virus. Thus, this response complements the inactivation of free virus by humoral antibody, which is directed against capsid or envelope proteins. b. Humoral response Whereas circulating antibodies may be directed against any virus protein, those that are of greatest significance in controlling an infection react specifically with epitopes on the surface of the virion, and result in inactivation of the virus's infectivity. The process is called neutralization. This response is of primary importance in suppressing diseases that involve a viremic stage, but secretory antibodies (IgA) also play an important protective role in primary infections of the respiratory and GI tracts. Humoral antibodies also take part in killing infected cells by two mechanisms: 1) antibody-dependent, cell-mediated cytotoxicity, in which natural killer cells and other leukocytes bearing Fc receptors bind to the Fc portions of antibodies that are complexed to virus antigens on the surface of the infected cell and kill it; and 2) complement-mediated lysis of infected cells to which virus-specific antibody has bound.