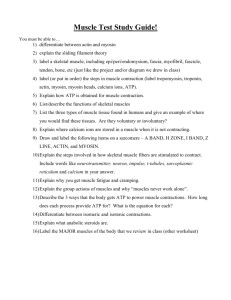
Muscle Physiology
advertisement

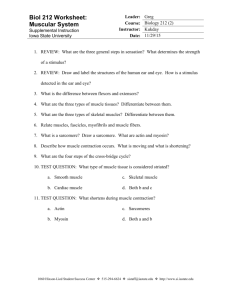
Muscle Physiology Muscle Tissue • Muscle accounts for nearly half of the body’s mass Muscles have the ability to change chemical energy (ATP) into mechanical energy • Three types of Muscle Tissue – differ in structure, location, function, and means of activation • Skeletal Muscle • Cardiac Muscle • Smooth Muscle Skeletal Muscle • Skeletal muscles attach to and cover the bony skeleton • Is controlled voluntarily (i.e., by conscious control) • Contracts rapidly but tires easily • Is responsible for overall body motility • Is extremely adaptable and can exert forces ranging from a fraction of an ounce to over 70 pounds • Has obvious stripes called striations • Each muscle cell is multinucleated Microscopic Anatomy - Skeletal Muscle Fiber • • Sarcoplasm contains glycosomes (granules of glycogen) and the oxygen-binding protein called myoglobin In addition to the typical organelles, fibers have • • • • Sarcoplasmic reticulum T tubules - modifications of the sarcolemma Myofibrils Each muscle fiber is made of many myofibrils, 80% of the muscle volume, that contain the contractile elements of skeletal muscle cells Myofibrils - Striations • Myofibrils are made up of 2 types of contractile proteins called myofilaments • Thick (Myosin) filaments • Thin (Actin) filaments • The arrangement of myofibrils creates a series of repeating dark A (anisotropic) bands and light I (isotropic) bands Myofibrils - Striations • The A band has a light stripe in the center called the H (helle) zone • The H zone is bisected by a dark line, the M line • I band has a darker midline called the Z disc (or Z line) Sarcomere • Smallest contractile unit of a muscle • Myofibril region between two successive Z discs, has a central A band and partial (half) I bands at each end Thick Filaments (16 nm diam) Myosin • Each myosin molecule (two interwoven polypeptide chains) has a rodlike tail and two globular heads • During muscle contraction, the Heads link the thick and thin filaments together, forming cross bridges Thin Filaments - Actin • Thin filaments are mostly composed of the protein actin. • Provides active sites where myosin heads attach during contraction. Tropomyosin and Troponin are regulatory subunits bound to actin. Ultrastructure of Muscle Sarcomere A band (c) Z disk Z disk Myofibril M line I band H zone (d) Titin Z disk M line Z disk M line Thin filaments Thick filaments (f) (e) Myosin heads Hinge Myosin tail region Myosin molecule Titin Tropomyosin Troponin Nebulin G-actin molecule Actin chain Figure 12-3c–f Arrangement of Filaments in a Sarcomere Sarcoplasmic Reticulum (SR) • SR - an elaborate, smooth ER that surrounds each myofibril. Perpendicular (transverse) channels at the A band - I band junction are the Terminal Cisternae (Lateral Sacs) SR regulates intracellular Ca2+ • T tubules at each A band/I band junction - continuous with the sarcolemma. Conduct electrical impulses to the throughout cell (every sarcomere) - signals for the release of Ca2+ from adjacent terminal cisternae Triad – 2 terminal cisternae and 1 T tubule • T tubules and SR provide tightly linked signals for muscle contraction • Interaction of integral membrane proteins (IMPs) from T tubules and SR Interaction of T-Tubule Proteins and SR Foot Proteins • T tubule proteins (Dihydropyridine) act as voltage sensors • SR foot proteins are (ryanodine) receptors that regulate Ca2+ release from the SR cisternae • Action potential in t-tubule alters conformation of DHP receptor • DHP receptor opens Ca2+ release channels in sarcoplasmic reticulum and Ca2+ enters cytoplasm (b) DHP receptor SR Foot Protein (Ca++ release channel) Ca2+ Ca2+ released Sliding Filament Model of Contraction • Contraction refers to the activation of myosin’s cross bridges – the sites that generate the force • In the relaxed state, actin and myosin filaments do not fully overlap • With stimulation by the nervous system, myosin heads bind to actin and pull the thin filaments • Actin filaments slide past the myosin filaments so that the actin and myosin filaments overlap to a greater degree (the actin filaments are moved toward the center of the sarcomere, Z lines become closer) Sliding Filament Model of Contraction Sliding Filament Model of Contraction Skeletal Muscle Contraction • For contraction to occur, a skeletal muscle must: • Be stimulated by a nerve ending • Propagate an electrical current, or action potential, along its sarcolemma • Have a rise in intracellular Ca2+ levels, the final stimulus for contraction • The series of events linking the action potential to contraction is called excitation-contraction coupling Depolarization and Generation of an AP • The sarcolemma, like other plasma membranes is polarized. There is a potential difference (voltage) across the membrane • When Ach binds to its receptors on the motor end plate, chemically (ligand) gated ion channels in the receptors open and allow Na+ and K+ to move across the membrane, resulting in a transient change in membrane potential - Depolarization • End plate potential - a local depolarization that creates and spreads an action potential across the sarcolemma Excitation-Contraction Coupling • E-C Coupling is the sequence of events linking the transmission of an action potential along the sarcolemma to muscle contraction (the sliding of myofilaments) • The action potential lasts only 1-2 ms and ends before contraction occurs. • The period between action potential initiation and the beginning of contraction is called the latent period. • E-C coupling occurs within the latent period. Regulatory Role of Tropomyosin and Troponin (b) Initiation of contraction 1 Ca2+ levels increase in cytosol. 2 Ca2+ binds to troponin. 3 Troponin-Ca2+ complex pulls tropomyosin away from G-actin binding site. 4 Power stroke 3 Tropomyosin shifts, exposing binding site on G-actin Pi ADP TN 4 Myosin binds to actin and completes power stroke. 5 2 5 Actin filament moves. G-actin moves 1 Cytosolic Ca2+ Figure 12-10b, steps 1–5 Excitation-Contraction Coupling 1 Somatic motor neuron releases ACh at neuromuscular junction. 2 (a) Net entry of Na+ through ACh receptor-channel initiates a muscle action potential. 1 Axon terminal of somatic motor neuron ACh Muscle fiber potential K+ 2 Action potential Na+ Motor end plate Sarcoplasmic reticulum T-tubule Ca2+ DHP receptor Tropomyosin Z disk Troponin Actin M line Myosin head Myosin thick filament Figure 12-11a, steps 1–2 Excitation-Contraction Coupling • The action potential is propagated along (across) the sarcolemma and travels through the T tubules • At the triads, the action potential causes voltage sensitive T tubule proteins to change shape. This change, in turn, causes the SR foot proteins of the terminal cisternae to change shape, Ca2+ channels are opened and Ca2+ is released into the sarcoplasm (where the myofilaments are) T tubule Terminal button Surface membrane of muscle cell Acetylcholine Acetylcholinegated cation channel Tropomyosin Actin Troponin Cross-bridge binding Myosin cross bridge Excitation-Contraction Coupling • Some of the Ca2+ binds to troponin, troponin changes shape and causes tropomysin to move which exposes the active binding sites on actin • Myosin heads can now alternately attach and detach, pulling the actin filaments toward the center of the sarcomere (ATP hydrolysis is necessary) Excitation-Contraction Coupling • The short calcium influx ends (30 ms after the action potential ends) and Ca2+ levels fall. An ATP-dependent Ca2+ pump is continually moving Ca2+ back into the SR. • Tropomyosin blockage of the actin binding sites is reestablished as Ca2+ levels drop. Cross bridge activity ends and relaxation occurs The Molecular Basis of Contraction Myosin filament 1 Tight binding in the rigor state. The crossbridge is at a 45° angle relative to the filaments. Myosin binding sites 1 45° ATP binding site 2 3 4 2 ATP binds to its binding site on the myosin. Myosin then dissociates from actin. G-actin molecule ADP 1 2 3 4 ATP 1 5 6 At the end of the power stroke, the myosin head releases ADP and resumes the tightly bound rigor state. 1 2 3 4 3 Pi Contractionrelaxation 5 Sliding filament Actin filament moves toward M line. Release of Pi initiates the power 5 stroke. The myosin head rotates on its hinge, pushing the actin filament past it. 90° 1 2 3 4 The ATPase activity of myosin hydrolyzes the ATP. ADP and Pi remain bound to myosin. ADP Pi 1 2 3 4 Pi 2 3 4 4 The myosin head swings over and binds weakly to a new actin molecule. The crossbridge is now at 90º relative to the filaments. Figure 12-9 Sequential Events of Contraction Motor Unit • Motor unit - One motor neuron and the muscle fibers it innervates • Number of muscle fibers varies among different motor units • Number of muscle fibers per motor unit and number of motor units per muscle vary widely • Muscles that produce precise, delicate movements contain fewer fibers per motor unit • Muscles performing powerful, coarsely controlled movement have larger number of fibers per motor unit Electrical and Mechanical Events in Muscle Contraction A twitch is a single contraction-relaxation cycle Figure 12-12 Muscle Twitch • A muscle twitch is the response of the muscle fibers of a motor unit to a single action potential of its motor neuron. The fibers contract quickly and then relax. Three Phases: • Latent Period – the first few ms after stimulation when excitation-contraction is occurring • Period of Contraction – cross bridges are active and the muscle shortens if the tension is great enough to overcome the load • Period of Relaxation – Ca2+ is pumped back into SR and muscle tension decreases to baseline level Graded Muscle Responses • Graded muscle responses are: • Variations in the degree or strength of muscle contraction in response to demand • Required for proper control of skeletal movement • Muscle contraction can be graded (varied) in two ways: • Changing the frequency of the stimulus • Changing the strength of the stimulus Muscle Response to Stimulation Frequency • A single stimulus results in a single contractile response – a muscle twitch (contracts and relaxes) • More frequent stimuli increases contractile force – wave summation - muscle is already partially contracted when next stimulus arrives and contractions are summed Muscle Response to Stimulation Frequency • More rapidly delivered stimuli result in incomplete tetanus – sustained but quivering contraction • If stimuli are given quickly enough, complete tetanus results – smooth, sustained contraction with no relaxation period Summation and Tetanus Factors Affecting Force of Muscle Contraction • Number of motor units recruited, recruitment also helps provide smooth muscle action rather than jerky movements • The relative size of the muscle fibers – the bulkier the muscle fiber (greater cross-sectional area), the greater its strength • Asynchronous recruitment of motor units -while some motor units are active others are inactive - this pattern of firing provides a brief rest for the inactive units preventing fatigue • Degree of muscle stretch Length – Tension Relationship Muscle Tone • The constant, slightly contracted state of all muscles • Does not produce active movements • Keeps the muscles firm and ready to respond to stimulus • Helps stabilize joints and maintain posture • Due to spinal reflex activation of motor units in response to stretch receptors in muscles and tendons Contraction of Skeletal Muscle Fibers • The force exerted on an object by a contracting muscle is called muscle tension, the opposing force or weight of the object to be moved is called the load. • Two types of Muscle Contraction: • When muscle tension develops, but the load is not moved (muscle does not shorten) the contraction is called Isometric • If muscle tension overcomes (moves) the load and the muscle shortens, the contraction is called Isotonic Isometric Contractions No change in overall muscle length In isometric contractions, increasing muscle tension (force) is measured Isotonic Contraction • In isotonic contractions, the muscle changes length and moves the load. Once sufficient tension has developed to move the load, the tension remains relatively constant through the rest of the contractile period. • Two types of isotonic contractions: • Concentric contractions – the muscle shortens and does work • Eccentric contractions – the muscle contracts as it lengthens Isotonic Contraction This illustrates a concentric isotonic contraction In isotonic contractions, the amount of shortening (distance in mm) is measured Energy Sources for Contraction • ATP is the only energy source that is used directly for contractile activity • As soon as available ATP is hydrolyzed (4-6 seconds), it is regenerated by three pathways: • Transfer of high-energy phosphate from creatine phosphate to ADP, first energy storehouse tapped at onset of contractile activity • Oxidative phosphorylation (citric acid cycle and electron transport system - takes place within muscle mitochondria if sufficient O2 is present • Glycolysis - supports anaerobic or high-intensity exercise CP-ADP Reaction • Transfer of energy as a phosphate group is moved from CP to ADP – the reaction is catalyzed by the enzyme creatine kinase • Creatine phosphate + ADP → creatine + ATP • Stored ATP and CP provide energy for maximum muscle power for 10-15 seconds Anaerobic Glycolysis • Glucose is broken down into pyruvic acide to yield 2 ATP • When oxygen demand cannot be met, pyruvic acid is converted into lactic acid • Lactic acid diffuses into the bloodstream – can be used as energy source by the liver, kidneys, and heart • Can be converted back into pyruvic acid, glucose, or glycogen by the liver Glycolysis and Aerobic Respiration • Aerobic respiration occurs in mitochondria - requires O2 • A series of reactions breaks down glucose for high yield of ATP • Glucose + O2 → CO2 + H2O + ATP Muscle Fatigue • Muscle fatigue – the muscle is physiologically not able to contract • Occurs when oxygen is limited and ATP production fails to keep pace with ATP use • Lactic acid accumulation and ionic imbalances may also contribute to muscle fatigue • Depletion of energy stores – glycogen • When no ATP is available, contractures (continuous contraction) may result because cross bridges are unable to detach Muscle Fiber Type: Speed of Contraction • Speed of contraction – determined by how fast their myosin ATPases split ATP • Oxidative fibers – use aerobic pathways • Glycolytic fibers – use anaerobic glycolysis • Based on these two criteria skeletal muscles may be classified as: • Slow oxidative fibers (Type I) contract slowly, have slow acting myosin ATPases, and are fatigue resistant • Fast oxidative fibers (Type IIA)contract quickly, have fast myosin ATPases, and have moderate resistance to fatigue • Fast glycolytic fibers (Type IIB)contract quickly, have fast myosin ATPases, and are easily fatigued Smooth Muscle • Occurs within most organs • Walls of hollow visceral organs, such as the stomach • Urinary bladder • Respiratory passages • Arteries and veins • Helps substances move through internal body channels via peristalsis • No striations • Filaments do not form myofibrils • Not arranged in sarcomere pattern found in skeletal muscle • Is Involuntary • Single Nucleus Smooth Muscle • Composed of spindle-shaped fibers with a diameter of 2-10 m and lengths of several hundred m • Cells usually arranged in sheets within muscle • Organized into two layers (longitudinal and circular) of closely apposed fibers • Have essentially the same contractile mechanisms as skeletal muscle Smooth Muscle • Cell has three types of filaments • Thick myosin filaments • Longer than those in skeletal muscle • Thin actin filaments • Contain tropomyosin but lack troponin • Filaments of intermediate size • Do not directly participate in contraction • Form part of cytoskeletal framework that supports cell shape • Have dense bodies containing same protein found in Z lines Contraction of Smooth Muscle • Whole sheets of smooth muscle exhibit slow, synchronized contraction • Smooth muscle lacks neuromuscular junctions • Action potentials are transmitted from cell to cell • Some smooth muscle cells: • Act as pacemakers and set the contractile pace for whole sheets of muscle • Are self-excitatory and depolarize without external stimuli Stimuli Influencing Smooth Muscle Contractile Activity Smooth Muscle • Muscle fiber stimulated • Ca2+ released into the cytoplasm from ECF • Ca2+ binds with calmodulin • Ca2+/Calmodulin activates mysoin kinase • Myosin kinase phosphorylates myosin • Myosin can now bind with actin Smooth Muscle Contraction ECF Ca2+ Sarcoplasmic reticulum 1 Intracellular Ca2+ concentrations increase when Ca2+ enters cell and is released from sarcoplasmic reticulum. 1 Ca2+ Ca2+ CaM Pi 2 Pi Ca2+ 2 Ca2+ binds to calmodulin (CaM). CaM Inactive MLCK 3 3 Ca2+–calmodulin activates myosin light chain kinase (MLCK). Active MLCK ATP 4 ADP + P Active myosin ATPase Inactive myosin P 4 MLCK phosphorylates light chains in myosin heads and increases myosin ATPase activity. Actin 5 Increased muscle tension 5 Active myosin crossbridges slide along actin and create muscle tension. Figure 12-28, steps 1–5 Comparison of Role of Calcium In Bringing About Contraction in Smooth Muscle and Skeletal Muscle Cardiac Muscle Tissue • Occurs only in the heart • Is striated like skeletal muscle but but has a branching pattern with intercalated Discs • Usually one nucleus, but may have more • Is not voluntary • Contracts at a fairly steady rate set by the heart’s pacemaker • Neural controls allow the heart to respond to changes in bodily needs