Cardiovascular System: The Heart
advertisement
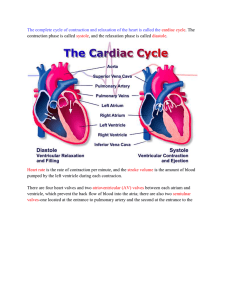
Cardiovascular System: The Heart Dr. Michael P. Gillespie Cardiovascular System Blood Heart Blood vessels Heart Propels the blood through the blood vessels to reach all of cells of the body. It circulates the blood through an estimated 100,000 km (60,000 miles) of blood vessels. Heart It beats 100,000 times every day (35 million beats / year). It pumps about 5 liters (5.3 qt) each minute and 14,000 liters (3,600 gal) each day. Cardiology – the study of the normal heart and diseases associated with it. Size And Shape About the size of a closed fist. Cone-shaped. 12cm (5 in.) Long, 9cm (3.5 in.) Wide, and 6cm (2.5 in.) Thick. 250g (8 oz) in adult females and 300g (10 oz) in adult males. Location Lies in the mediastinum (a mass of tissue between the sternum and the vertebral column). 2/3 of the mass is left of midline. A cone lying on its side. Anatomical Landmarks The apex (pointed end) is directed anteriorly, inferiorly, and to the left. The base (broad portion) is directed posteriorly, superiorly, and to the right. Anterior surface – deep to sternum & ribs. Anatomical Landmarks Inferior surface – rests upon diaphragm. Right border – faces the right lung. Left border (pulmonary border) – faces the left lung. Cardiopulmonary Resuscitation (CPR) External pressure (compression) can be used to force blood out of the heart and into the circulation. CPR is utilized when the heart suddenly stops beating. Cardiac compressions with artificial ventilation of the lungs keeps oxygenated blood circulating until the heart can be restarted. Self CPR (coughing). Pericardium Pericardium – membrane that surrounds and protects the heart. Fibrous pericardium – tough, inelastic, dense irregular CT. Prevents overstretching of the heart. Serous pericardium – thinner, more delicate layer. Parietal layer. Visceral layer (epicardium) – adheres to the heart. Pericardial fluid lies in between these two layers in the pericardial cavity. Layers Of The Heart Wall Epicardium (visceral layer of the serous pericardium). Myocardium – cardiac muscle tissue. Endocardium – smooth lining of the chambers of the heart and valves (continuous with blood vessels). Chambers Of The Heart Atria – superior chambers. Auricle – pouchlike structure. Ventricles – inferior chambers. Sulci – grooves on the surface of the heart that contain blood vessels. Chambers Of The Heart Right atrium – receives blood from three veins: superior vena cava, inferior vena cava, and coronary sinus. Tricuspid valve. Pectinate muscles. Interatrial septum. Fossa ovalis – depression (remnant of foramen ovale). Chambers Of The Heart Right ventricle – receives blood from right atrium. Trabeculae carneae – bundles of cardiac muscle tissue. Chordae tendineae – connects to the cusps of the tricuspid valve which are connected to papillary muscles. Interventricular septum. Pulmonary valve into pulmonary arteries. Chambers Of The Heart Left atrium – receives blood from the lungs through the pulmonary veins. Bicuspid (mitral) valve. Left ventricle – receives blood from left atrium. Trabeculae carneae – bundles of cardiac muscle tissue. Chordae tendineae – connects to the cusps of the bicuspid valve which are connected to papillary muscles. Aortic valve into the ascending aorta (largest artery). Myocardial Thickness The function of the individual chambers determines their thickness. The atria pump blood a short distance and consequently have thinner walls than the ventricles. The left ventricle pumps blood a greater distance than the right at higher pressures and has a thicker wall. Fibrous Skeleton Of The Heart Dense CT rings that surround the valves and prevent overstretching. Provides insertion points for bundles of cardiac muscle fibers. Atrioventricular (AV) Valves Tricuspid and bicuspid valves. When the valve is open, the pointed cusps point into the ventricle. Atrioventricular (AV) Valves When atrial pressure is higher than ventricular pressure the valves open (the papillary muscles are relaxed and the chordae tendinae is slack. When the ventricles contract the pressure forces the AV valves closed. The papillary muscles close concurrently. Damaged valves allow regurgitation (flow back). Semilunar (SL) Valves The aortic and pulmonary valves. The SL valves open when the pressure in the ventricles exceeds the pressure in the arteries. Heart Valve Disorders Stenosis (narrowing) – failure of the heart valve to open fully. Insufficiency (incompetence) – failure of a valve to close fully. Mitral stenosis – due to scar formation of a congenital defect. Heart Valve Disorders Mitral insufficiency – backflow of blood from the left ventricle to the left atrium. Mitral valve prolapse (MVP) – one or both cusps protrude into the left atrium during ventricular contraction. Aortic stenosis – the aortic valve is narrowed. Heart Valve Disorders Aortic insufficiency – backflow of blood from the aorta into the left ventricle. Rheumatic fever – an acute systemic inflammatory disease. Antibodies produced to destroy the bacteria attack and inflame the CT of joints, heart valves and other organs. Systemic And Pulmonary Circulations Two closed systems. The output of one becomes the input of another with each beat of the heart. Coronary Circulation The myocardium has its own blood vessels, the coronary circulation. The coronary arteries branch from the ascending aorta and encircle the heart. When the heart is contracting the coronary arteries are squeezed shut. When the heart is relaxed, the high pressure from the aorta pushes blood into the coronary arteries and from the arteries to the coronary veins. Coronary Arteries Two coronary arteries, right and left coronary arteries, branch from the ascending aorta and supply oxygenated blood to the myocardium. Coronary Arteries Left coronary artery branches into: Anterior interventricular or left anterior descending LAD (supplies ventricle walls). Circumflex branches (supplies left ventricle and left atrium). Coronary Arteries Right coronary artery branches into: Atrial branches (supplies right atrium). Posterior interventricular branch (supplies the two ventricles). Right marginal branch (supplies the right ventricle). Coronary Veins The great cardiac vein (anterior) and the middle cardiac vein (posterior) drain into the coronary sinus. Coronary Sinus – a large bascular sinus on the posterior surface of the heart. Reperfusion Damage Reperfusion is reestablishing the blood flow to the heart muscle after a blockage of a coronary artery. Reperfusion damages the tissue further due to the formation of oxygen free radicals from the reintroduced oxygen. Histology Of Cardiac Muscle Tissue Cardiac muscle fibers are shorter in length and less circular than skeletal muscle fibers. Cardiac muscle fibers exhibit branching. Histology Of Cardiac Muscle Tissue Usually one centrally located nucleus is present, although it may occasionally have two nuclei. Intercalated disc connect neighboring fibers. The discs contain desmosomes, which hold the fibers together. Mitochondria are larger and more numerous in cardiac muscle fiber. Gap junctions allow for propagation of action potentials. Regeneration Of Heart Cells Infarcted (dead) cardiac muscle tissue is replaced with noncontractile fibrous scar tissue. A lack of stem cells limits the ability of the heart to repair damage. Some stem cells from the blood migrate into the heart tissues and differentiate into functional muscle cells and endothelial cells. Autorhythmic Fibers: The Conduction System Autorhythmic fibers are self-excitable and maintain the heart’s continuous beating. Act as a pacemaker, setting the rhythm of electrical excitation that causes contraction of a heart. Form a conduction system, that provides a path for the cycle of cardiac excitation through the heart. Sequence Of Cardiac Conduction Sinoatrial (SA) node – undergo spontaneous depolarization (pacemaker potential) – propagates through the atria through gap junctions. Atrioventricular (AV) node (bundle of his) – site where action potentials are conducted from the atria to the ventricles. Sequence Of Cardiac Conduction Right and left bundle branches – propagate action potentials through the ventricles and the interventricular septum to the apex of the heart. Purkinje fibers – conduct the action potentials from the apex, through the remainder of the ventricles stimulating contraction. Pacemaker The SA node regulates the pace of the heart. At rest, it contracts approximately 100 time per minute. Nerve impulses from the ANS and blood born hormones (epinephrine) modify the timing and strength of each heartbeat. Pacemaker Acetylcholine from the ANS slows the heart rate to about 75 bpm. If the SA node becomes damaged, the AV node can pick up the job; However, at a slower rate (40 – 60 bpm). If both nodes are damaged, an artificial pacemaker sends out electrical currents to stimulate the heart to contract. Ectopic Pacemaker If a site other than the SA node becomes self-excitable, it becomes an ectopic pacemaker. It make operate occasionally, producing extra beats, or for a period of time. Triggers: Caffeine, nicotine, electrolyte imbalances, hypoxia, and toxic reactions to drugs. Refractory Period In cardiac muscle tissue, the refractory period lasts longer than the contraction period. This prevents tetanus (maintained contraction). Electrocardiogram (ECG or EKG) As action potentials propagate through the heart, they generate electrical currents that can be detected on the surface of the body. An electrocardiogram is a recording of these signals. An electrocardiograph is the instrument used to record the signals. Electrocardiogram (ECG or EKG) Electrodes are positioned on the arms and legs (limb leads) and at six positions on the chest (chest leads). 12 different tracings are produced from different combinations of leads. Electrocardiogram (ECG or EKG) If these tracings are compared to one another and to a normal tracing, it is possible to determine the following: If the conducting pathway is abnormal. If the heart is enlarged. If certain regions of the heart are damaged. Typical Lead II Record Three clearly recognizable waves appear with each heartbeat. P wave – atrial depolarization. QRS complex – rapid ventricular depolarization. T wave – ventricular repolarization. Changes In Wave Size Large P waves – enlargement of the atrium. Large Q waves – myocardial infarction. Large R waves – enlarged ventricles. Flat T wave – insufficient oxygen. Large T wave – hyperkalemia (high blood K+ levels). Stress Electrocardiogram (Stress Test) Elevate the heart’s response to stress. Narrowed coronary arteries may carry adequate blood supply at rest, but not during exercise. Changes In Time Span Between Waves Time spans between waves are called intervals or segments. P-Q interval – time between the beginning of the P wave and the beginning of the QRS complex. The P-Q interval represents the time required for an action potential to travel through the atria, AV node and remaining fibers of the conduction system. Changes In Time Span Between Waves The P-Q interval lengthens when the action potentials must travel around scar tissue from rheumatic fever. The S-T segement is elevated in acute myocardial infarction and depressed when the heart receives insufficient oxygen. The Q-T interval may be lengthened by myocardial damage, myocardial ischemia, or conduction abnormalities. Terminology Systole – the phase of contraction. Diastole – the phase of relaxation. Cardiac cycle – all of the events associated with one heartbeat (systole and diastole of the atria and systole and diastole of the ventricles). Heart Sounds Auscultation – listening to sounds within the body (performed with a stethoscope). During each cardiac cycle there are 4 heart sounds, but in a normal heart, only the first and second heart sounds (S1 and S2) are loud enough to be heard with a stethoscope. Heart Sounds The first sound (S1), described as a lubb sound, is louder and longer than the second. Caused by closure of the AV valves after ventricular systole begins. The second sound (S2), described as dupp sound, is shorter and not as loud as S1. Caused by closure of the semilunar valves as ventricular diastole begins. Heart Sounds S3 is due to blood turbulence from rapid ventricular filling. S4 is due to blood turbulence during atrial systole. S3 and S4 are not normally heard. Heart Murmurs A heart murmur is an abnormal sound consisting of a clicking, rushing, or gurgling noise that is heard before, between, or after the normal heart sounds. It can also mask the normal heart sounds. Some heart murmurs are “innocent”; However, they usually represent a valve disorder. Congestive Heart Failure In CHF, the heart is a failing pump. Causes include coronary artery disease, congenital defects, longterm high blood pressure (increases afterload), myocardial infarctions, valve disorders. Pulmonary edema – left ventricle fails first. Peripheral edema – right ventricle fails first. Regulation Of Heart Rate Autonomic regulation of heart rate. Proprioceptors, chemoreceptors, baroreceptors. Cardiac accelerator nerves. Chemical regulation of heart rate. Hormones (epinephrine, norepinephrine, and thyroid hormones) accelerate the heart rate. Cations. Terminology Tachycardia – elevated resting heart rate. Bradycardia – a resting heart rate under 60 bpm. Hypothermia – lowering of the body temperature, which slows the heart rate. Disorders Of The Heart Coronary artery disease (CAD). Arteriosclerosis and atherosclerosis. Disorders Of The Heart Myocardial ischemia and infarction. Hypoxia. Angina pectoris. Disorders Of The Heart Congenital defects. Coarctation of the aorta. Patent ductus arteriosus. Septal defect. Atrial and ventricular. Tetralogy of Fallot. Disorders Of The Heart Arrhythmias – irregularity of the heart rhythm. Heart block. Flutter and fibrillation. Ventricular premature contraction. Medical Terminology Angiocardiography – x-ray examination of the heart and great vessels with radiopaque dye. Cardiac arrest. Cardiomegaly. Cor pulmonale (CP) – ventricular hypertrophy from disorders that bring about hypertension in the pulmonary circulation. Palpitation.