Gastric secretions
advertisement

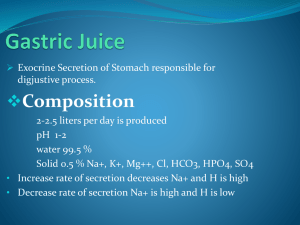
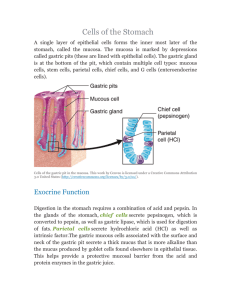
Gastric secretions • Gastric secretion is a colorless, watery, acidic, digestive fluid produced in the stomach . • Physical properties; • It is a watery fluid, that has a pale yellow colour , pH is 1-3 , the volume secreted per day is 2-3 L . • The stomach is famous for its secretion of acid, but acid is only one of four major secretory products of the gastric epithelium, all of which are important either to the digestive process or to control of gastric function. • Chemical composition; It is 97-99% water , it contains inorganic salts ,and organic components that include ,mucin, digestive enzymes , hormones …. Digestive system Gastric Glands and secretions • The gastric secretion is produced by the epithelium cells of the gasric glands . Goblet cells or mucus cells:are mucous cells, which cover the entire lumenal surface and extend down into the glands as "mucous neck cells". These cells secrete a bicarbonate-rich mucus that coats and lubricates the gastric surface, and serves an important role in protecting the epithelium from hydrochloric acid and pepsin and other chemical insults. . Gastric Mucus-Bicarbonate Barrier 4 Gastric Glands and secretions • Parietal cells: They secret HCl into the stomach lumen where it establishes an extremely acidic environment. This acid is important for activation of pepsinogen and inactivation of ingested microorganisms such as bacteria. . • It also secrets the intrinsic factor, a glycoprotein secreted by parietal cells that is necessary for intestinal absorption of vitamin B12. • Chief cells: It secrets pepsinogen(zymogen). Once secreted, pepsinogen is activated by stomach acid into the active protease pepsin, which is largely responsible for the stomach's ability to initiate digestion of proteins. In young animals, chief cells also secrete rennin a protease that helps coagulate milk allowing it to be retained more than briefly in the stomach – The epithelium cells also produce important hormones gastrin a peptide that is important in control of acid secretion and gastric motility. and somatostatin. Gastric Glands and secretions Exocrine gland cells of gastric pits Produce alkaline mucus that covers mucosa layer Synthesize and secrete the protease precursor known as pepsinogen. Synthesize and secrete the HCl acid responsible for the acidic pH in the gastric lumen. 8 HCl Functions • Makes gastric juice very acidic. – Denatures ingested proteins (alter tertiary structure) so become more digestible. • Activates pepsinogen to pepsin. – Pepsin is more active at pH of 2.0. Insert fig. 18.9 HCl Production • Parietal cells secrete H+ into gastric lumen by primary active transport, through H+/ K+ ATPase pump. • Parietal cell’s basolateral membrane takes in Cl- against its electrochemical gradient, by coupling its transport with HC03-. Insert fig. 18.8 Gastric secretion phases Gastric acid secretion can be divided • into three phases: • Cephalic phase mediated by the CNS and • triggered by smelling, chewing or even the thought • of food. Mediated by the vagus and acounts for 10• 30% of the cid secreted). • Gastric phase triggered by the presence of food in • the stomach (both chemical and mechanical • sensing are involved). Accounts for 70-90% of the • acid secretion • Intestinal phase. Presence of chyme, most • probably amino acids, in the intestine triggers • approximately 5% of the gastric acid secretion. Gastric and Peptic Ulcers • Peptic ulcers: – Erosions of the mucous membranes of the stomach or duodenum produced by action of HCl. • Zollinger-Ellison syndrome: – Ulcers of the duodenum are produced by excessive gastric acid secretions. • Helicobacter pylori: – Bacterium that resides in GI tract that may produce ulcers. • Acute gastritis: – Histamine released by tissue damage and inflammation stimulate further acid secretion. HCl Production • Parietal cells secrete H+ into gastric lumen by primary active transport, through H+/ K+ ATPase pump. • Parietal cell’s basolateral membrane takes in Cl- against its electrochemical gradient, by coupling its transport with HC03-. Insert fig. 18.8 Hydrochloric Acid Production 1. CO2 and Cl- diffuse from the blood into the stomach cell. 2. CO2 combines with H2O to form H2CO3. 3. H2CO3 dissociates into bicarbonate (HCO3-) and H+. 4. H+ combines with Cl- in duct of gastric gland to form HCl-. 5. An ATP pump is necessary to pump the HCl- into the duct since the concentration of HCl- is about a million times more concentrated in the duct than in the cytosol of the cell. II.2 Composition and function of gastric secretions 1. HCl converts pepsinogen to pepsin for chemical digestion provides optimal pH environment for pepsin destroys some bacteria stimulates the small intestinal mucosa to release secretinand CCK promotes the absorption of Ca2+ and Fe2+ in small intestine 15 Composition and function of gastric secretions 2. Pepsinogen (precursor of pepsin) digestion of proteins 3. Mucus forms a protective barrier: Mucus-bicarbonate barrier 4. Intrinsic factor combines with vitamin B12 to make it absorbable 16 Control of Gastric Acid Secretion Gastric acid secretion is controlled by three mechanisms: • • • Neurocrine (denoting an endocrine influence on or by the nerves). Endocrine (gastrin) Paracrine (histamine) in contrast to true endocrines these hormones are not released into the bloodstream but into the surrounding tissues and act in the immediate vicinity, e.g. intestinal mucosal hormones. 17 Regulation of Gastric Secretion • Neural and hormonal mechanisms regulate the release of gastric juice • gastric secretion occurs in three phases – Cephalic (reflex) phase: prior to food entry – Gastric phase: once food enters the stomach – Intestinal phase: as partially digested food enters the duodenum Cephalic Phase • Stimulated by sight, smell, and taste of food. • Activation of vagus: – Stimulates chief cells to secrete pepsinogen. – Directly stimulates G cells to secrete gastrin. – Directly stimulates ECL cells to secrete histamine. – Indirectly stimulates parietal cells to secrete HCl. • Continues into the 1st 30 min. of a meal. Gastric Phase • Arrival of food in stomach stimulates the gastric phase. • Gastric secretion stimulated by: – Distension. – Chemical nature of chyme (amino acids and short polypeptides). • Stimulates G cells to secrete gastrin. • Stimulates chief cells to secrete pepsinogen. • Stimulates ECL cells to secrete histamine. – Histamine stimulates secretin of HCl. – Positive feedback effect. • As more HCl and pepsinogen are secreted, more polypeptides and amino acids are released. – Intestinal phase: as partially digested food enters the duodenum B. Functional Phases of Gastric Secretion 2. Gastric Phase of 1. Cephalic Phase of Gastric Secretion (approx. 30% of total) Gastric Secretion (approx 60% of total) (initiated by brain) (initiated by gastric events) vagus nerve vagus nerve FOOD HCl HCl Distension Peptides circulation G circulation G gastrin gastrin Regulation of Gastric Secretion • Secretion of HCl is also regulated by a negative feedback effect: – HCl secretion decreases if pH < 2.5. – At pH of 1.0, gastrin secretion ceases. • D cells stimulate secretion of somatostatin. Endogenous substances regulating gastric secretion 协同作用 23 Regulation of Gastric Secretion • Neural and hormonal mechanisms regulate the release of gastric juice • Stimulatory and inhibitory events occur in three phases – Cephalic (reflex) phase: prior to food entry – Gastric phase: once food enters the stomach – Intestinal phase: as partially digested food enters the duodenum B. Functional Phases of Gastric Secretion 2. Gastric Phase of 1. Cephalic Phase of Gastric Secretion (approx. 30% of total) Gastric Secretion (approx 60% of total) (initiated by brain) (initiated by gastric events) vagus nerve vagus nerve FOOD HCl HCl Distension Peptides circulation G circulation G gastrin gastrin Peptic ulcers: Erosions of the mucous membranes of the stomach or duodenum produced by action of HCl. Control of Gastric Acid Secretion Gastric acid secretion is controlled by three mechanisms: • • • Neurocrine (denoting an endocrine influence on or by the nerves). Endocrine (gastrin) Paracrine (histamine) in contrast to true endocrines these hormones are not released into the bloodstream but into the surrounding tissues and act in the immediate vicinity, e.g. intestinal mucosal hormones. 27