HCAP_02 (Treatment)
advertisement

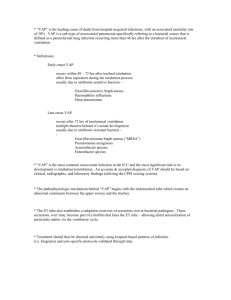
HCAP (Treatment) INTRODUCTION 1. HAP, VAP, and HCAP are important causes of morbidity and mortality despite improved antimicrobial therapy, supportive care, and prevention. 2. The treatment of HAP, VAP, and HCAP will be reviewed here. The diagnosis, epidemiology, pathogenesis, microbiology, risk factors, and prevention of HAP, VAP, and HCAP are discussed separately. MULTIDRUG RESISTANCE 1. The definition of MDR in GNB, which are important cause of HAP, VAP, and HCAP, is variably defined as resistance to at least 2, 3, 4, or 8 of antibiotics typically used to treat infections with these organisms. XDR GNB is defined by resistance to all commonly used systemic antibiotics except colistin, tigecycline, and AMG. Awareness of local resistance patterns is critical for decisions regarding empiric therapy for HAP, VAP, and HCAP. 2. Panresistance refers to those GNB with diminished susceptibility to all of antibiotics recommended for empiric treatment of VAP, including cefepime, ceftazidime, imipenem, meropenem, piperacillin-tazobactam, ciprofloxacin, and levofloxacin. 3. Risk factors for multidrug resistance are discussed separately. TREATMENT 1. Approach to therapy A. Appropriate antibiotic significantly improves survival for patients with HAP, VAP, or HCAP. However, establishing diagnosis of pneumonia in such patients can be difficult, B. C. especially those on mechanical ventilation in whom clinical, radiologic, and microbiologic findings can be due to numerous etiologies besides pneumonia. The difficulty in diagnosis may lead to overtreatment with its attendant risks of superinfection and antibiotic toxicity. When therapy is given, antimicrobial selection should be based upon risk factors for MDR pathogens, including recent antibiotic therapy (if any), resident flora in hospital or ICU, presence of underlying diseases, and available culture data (interpreted with care). For patients with risk factors for MDR pathogens, empiric broad-spectrum multidrug therapy is recommended. Once results of pre-therapy cultures are available, therapy should be narrowed based upon susceptibility pattern of pathogens identified. The importance of providing appropriate therapy at time of presentation was illustrated in retrospective study of almost 400 patients with culture-positive HCAP who survived but remained hospitalized 48 hours after hospital admission. Mortality was significantly higher among 107 patients who received inappropriate initial therapy compared with 289 patients who received appropriate coverage (30 vs. 18%); switching to appropriate regimen did not reduce the risk of death. D. E. F. G. In study that assessed microbial prediction and validated adequacy of 2005 ATS/IDSA guidelines for HAP in ICU, adherence to guidelines resulted in more adequate treatment and trend toward better clinical response in patients who presented late (≥ 5 days) or had risk factors for drug-resistant bacteria but did not affect mortality. 2005 guidelines were worse than 1996 guidelines for predicting drug-resistant bacteria; this was mostly observed for cases classified as lower risk for multidrug-resistant pathogens (early-onset infection without specified risk factors for resistant infection), suggesting that such patients may in fact be at risk for resistant pathogens. In survey of physicians at academic medical centers, respondents selected guideline-concordant antibiotic regimens only 9% of time for HCAP compared with 78% of time for CAP. A retrospective study showed that HCAP is associated with more severe disease, longer hospital stay, and higher mortality rates than CAP and that use of antimicrobial therapy not recommended by ATS/IDSA guidelines was associated with increased mortality in such patients. Another observational study found that lack of adherence to VAP protocol (which included considerations of appropriate use and duration of antibiotics) resulted in longer duration of therapy, ventilation, and length of ICU stay. In observational study that included 303 patients at risk for MDR pathogens, 28-day mortality was higher among patients who were treated according to ATS/IDSA guidelines compared with patients whose treatment did not comply with the guidelines (34 vs. 20%). The primary reason for "noncompliance" was lack of second drug for gram-negative pathogens. Criticisms of this study include the observation that lower coverage for certain MDR pathogens occurred in the compliant group (but was not commented upon by the authors), lack of assessment of impact of timing of antimicrobial therapy, lack of appropriate adjustment for risk of death, disregard of impact of treatment de-escalation on classification of compliance, and possibility that excess mortality may have been at least partly due to toxicity when triple regimen is used. In addition, although authors attempted to control for higher severity of infection observed in compliant group, results may still have been confounded by patients in compliant group who were at greater risk of poor outcomes at presentation. Potential messages from this study. i. ii. iii. Clinicians who are following patients and are aware of pathogen and susceptibility patterns within specific unit may be better able to appropriately select empiric therapy based on individual clinical judgment rather than using routine combination therapy (guidelines are meant to supplement clinical judgment, not supplant judgment). The need for two-drug therapy is not necessary in many cases of gram-negative bacterial infection. The definition of risk for MDR as stated in 2005 guidelines is not precise, particularly for HCAP, and should be readdressed. H. I. Various editorials and studies have reported that it is overgeneralization to consider all HCAP patients at increased risk for MDR pathogens. The challenge for clinicians is to correctly identify HCAP patient who is most likely to benefit from empiric treatment with broad-spectrum antibiotics with activity against MDR pathogens. The definition of HCAP is being reevaluated, and future investigations are required to better define patients with HCAP who are likely to be infected with MDR pathogens. Given concerns about lack of precision of definition of HCAP for detecting patients infected with resistant organisms, validation study of clinical scoring system for predicting resistant bacteria was performed, which compared definition of HCAP to scoring system. The risk score was calculated using the following weighted points. i. Recent hospitalization of at least 48 hours during the preceding 90 days – 4 points ii. Residence in a nursing home – 3 points iii. Chronic hemodialysis – 2 points iv. Critical illness – 1 point J. The risk score was higher in patients with pneumonia caused by resistant pathogen than in those without resistant pathogen (median score 4 vs. 1) and was more accurate than definition of HCAP for detecting patients with pneumonia caused by resistant bacteria, including MRSA, P. aeruginosa, and ESBL. A risk score > 0 had NPV of 85%; thus, risk score of 0 could lead to fewer patients unnecessarily receiving broad-spectrum antibiotics if it is used to guide choice of therapy. Another study of patients requiring hospitalization for pneumonia who came from community found that hospitalization in K. L. preceding 90 days (OR 4.87) and residency in nursing home (OR 3.55) were independent predictors of infection with resistant pathogen; these factors were also independent predictors of in-hospital mortality. In retrospective analysis of local microbiologic data on HAP pathogens from 111 consecutive patients in 2004, investigators developed institution-specific treatment guidelines in order to improve empiric antibiotic therapy. Institution guideline-directed treatment regimens were predicted to provide adequate initial therapy for > 90% of patients who develop HAP ≥ 10 days after hospitalization (those at greatest risk of MDR pathogens). In this institution, use of fluoroquinolone per national guidelines would not have provided adequate additional antimicrobial activity for β-lactam–resistant GNB (ciprofloxacin was active against < 10% of these pathogens that were also resistant to piperacillin-tazobactam and cefepime). This study illustrates importance of using local susceptibility data to develop treatment guidelines. The implementation of recommendations to assess patient's status 72 hours after initiation of therapy and to discontinue antibiotics or narrow regimen (deescalate therapy) based upon appropriate culture results may reduce selective pressure for antimicrobial resistance. M. A prospective observational study of 398 ICU patients with suspected VAP found that mortality was significantly lower among patients in whom therapy was deescalated compared with those whose therapy was either escalated or unchanged (17 vs. 43 and 24%). The study was limited because of its observational nature; confirmation of these results awaits RCT. In another study, deescalation was evaluated in surgical patients with septic shock in retrospective evaluation of 138 patients with VAP. Deescalation of antimicrobial therapy occurred in 55% of patients who had received initial therapy effective against identified pathogen (most common initial choice was vancomycin plus piperacillin-tazobactam). The mortality rate of patients who underwent deescalation therapy was 35% compared with 42% among patients who did not have deescalation, difference that did not reach statistical significance. This study demonstrated that 2. deescalation therapy did not lead to recurrent pneumonia or increased mortality in this population of critically ill surgical patients. N. Antimicrobial stewardship programs have been shown to reduce rates of nosocomial infections (including C. difficile, MRSA, and VRE infections) and antimicrobial expenditures without affecting mortality or length of hospital stay. Antimicrobial stewardship programs have also been shown to reduce rates of infections with MDR GNB. Specific antimicrobial consideration A. In critically ill patients, in those receiving antibiotics prior to onset of pneumonia and in institutions where these pathogens are frequent, coverage of MRSA, P. aeruginosa, and antibiotic-resistant GNB such as Acinetobacter spp and Legionella should be considered. B. Methicillin-resistant Staphylococcus aureus i. If MRSA is frequent nosocomial pathogen in institution, linezolid or vancomycin is necessary first choice for anti-staphylococcal coverage but should be discontinued if MRSA is not isolated. Telavancin is alternative agent when neither linezolid nor vancomycin can be used. ii. An overview of treatment of invasive MRSA infections is presented separately. iii. Linezolid and vancomycin 1. A meta-analysis of 9 RCT that compared linezolid to vancomycin for HAP found no differences in rates of death, clinical response, microbiologic eradication, or 2. 3. MRSA eradication. Linezolid was associated with higher rate of GI adverse effects, but there were no differences in rates of AKI, thrombocytopenia, or drug discontinuation due to adverse effects. Another meta-analysis, which included 8 trials that compared linezolid to vancomycin or teicoplanin for treatment of suspected MRSA pneumonia, found no differences in clinical success, microbiologic success, or mortality. It should be noted that studies included in meta-analyses described above used dosing regimen for vancomycin that is significantly lower than what is recommended by ATS and IDSA. 4. In later randomized double-blind trial that compared linezolid with vancomycin for the treatment of HAP or HCAP due to proven MRSA, the end of study success rate was 58% for linezolid and 47% for vancomycin. Among patients who had a respiratory specimen available for culture at the end of treatment, 16 of 92 patients (17%) who received linezolid had cultures that were persistently positive for MRSA compared with 50 of 109 patients (46%) who received vancomycin. In this study, vancomycin dosing was adjusted to achieve target trough levels. Linezolid was non-inferior and statistically superior to vancomycin in end of treatment clinical outcome and microbiologic outcome at end of treatment and end of study, but there were no differences in all-cause 60-day mortality or overall adverse events. Nephrotoxicity iv. occurred more commonly with vancomycin than linezolid (18 vs. 8%). Dosing and vancomycin trough 1. Linezolid – 600 mg BID 2. Vancomycin – 15 to 20 mg/kg (based on actual body weight) IV every 8 to 12 hours for patients with normal renal function, with target serum trough of 15 to 20 mg/L. In seriously ill patients, loading dose of 25 to 30 mg/kg can be used to facilitate rapid attainment of target trough concentration. 3. A retrospective study suggested that vancomycin failure might be related to suboptimal dosing. As result, trough of 15 to 20 mcg/mL is targeted. However, subsequent studies failed to confirm that higher vancomycin trough concentrations correlate with improved outcomes. On the other hand, higher vancomycin MIC themselves may be associated with worse outcomes in patients with HAP due to MRSA. This was suggested in prospective cohort study of 95 patients with MRSA HCAP who were treated with vancomycin in which targeted trough vancomycin concentration was at least 4 times the MIC. High MIC (≥ 2 mcg/mL) strains of MRSA were detected in 54% of patients. Despite achieving target trough concentration, mortality was higher among patients whose MRSA strain had high MIC than patients whose MRSA strain had low MIC (24 vs. 10%). In later prospective study that included 158 patients in ICU with HAP, VAP, or HCAP, an increase in 28-day mortality was observed 4. in patients whose MRSA isolates had increased MICs; increase in mortality occurred as vancomycin MIC increased from 0.75 to 3 mcg/mL and was present even for strains within susceptible range. 2005 ATS/IDSA treatment guidelines on HAP, VAP, and HCAP; 2011 IDSA guidelines for treatment of MRSA infections; and 2009 United States pharmacy consensus review recommend target vancomycin trough of 15 to 20 mcg/mL. However, these recommendations are based on retrospective pharmacokinetic modeling in absence of prospective clinical data. 5. 6. v. PK/PD analysis has suggested that lung vancomycin AUC:MIC > 400 may be difficult to achieve (particularly for isolates with MIC > 1). Clinical data have failed to demonstrate relationship between treatment outcome and target troughs of 15 to 20 mcg/mL. 2005 ATS/IDSA guidelines on HAP, VAP, and HCAP and 2011 IDSA guidelines for treatment of MRSA infections recommended either linezolid or vancomycin for infections suspected or proven to be due to MRSA. It was noted that linezolid might be preferred in patients at risk for or with renal insufficiency in whom vancomycin is often underdosed and is associated with risk of nephrotoxicity. Linezolid also may reduce toxin production, although possible benefit of this has not been established. Linezolid is particularly preferred in hospitals in which substantial proportion of MRSA isolates have vancomycin MIC ≥ 2 mcg/mL. Linezolid resistance and linezolid failure have been described rarely. An alternative to linezolid and vancomycin is clindamycin (600 mg TID), provided that the isolate is known to be susceptible, although there are fewer data to supports its use. Telavancin 1. Telavancin is antibiotic with activity against MRSA. In 2013, telavancin was approved by FDA for treatment of HAP and VAP caused by S. aureus but not for other bacterial causes of HAP or VAP; it is recommended only when alternative agents cannot be used. In patients with normal renal function, the 2. 3. 4. dose of telavancin is 10 mg/kg IV every 24 hours. Patients with preexisting moderate or severe renal impairment (CCR ≤ 50 mL/min) who were treated with telavancin for HAP or VAP had increased mortality compared with vancomycin. Use of telavancin in patients with preexisting moderate or severe renal impairment (CCr ≤ 50 mL/min) should therefore be considered only when potential benefit to patient outweighs potential risk. New onset or worsening renal impairment has occurred in patients receiving telavancin. Renal function should be monitored in all patients receiving telavancin. Adverse developmental outcomes were observed in three animal species at clinically relevant doses. These findings raise concerns about potential adverse developmental outcomes in humans. Women of childbearing potential should have a serum pregnancy test prior to administration of telavancin, and its use should be avoided during pregnancy unless the potential benefit to the patient outweighs the potential risk to the fetus. 5. vi. In two randomized trials, among patients with HAP due to monomicrobial infection with MRSA, the cure rate (regardless of vancomycin MIC) was 82% for telavancin and 74% for vancomycin. The cure rate among patients with MRSA with reduced susceptibility to vancomycin (MIC ≥ 1 mg/dL) was 87% in those who received telavancin vs. 74% in those who received vancomycin. It is important to note that dose of vancomycin that was used in these studies was lower than the dose that is currently recommended. Potentially clinically significant increases in creatinine (> 50% increase from baseline and maximum value > 1.5 mg/dL) were more common in the telavancin group than in the vancomycin group (16 vs. 10%). Other agent 1. 2. 3. 4. 5. There has been interest in using other agents for the treatment of MRSA pneumonia, but none of the following agents can be recommended. Daptomycin cannot be used to treat pneumonia because it does not achieve sufficiently high concentrations in the respiratory tract. Data are limited on the use of quinupristin-dalfopristin. In a randomized trial of HAP that included 38 patients with MRSA pneumonia, there was non-significant lower rate of clinical success with quinupristin-dalfopristin compared with vancomycin (31 vs. 44%) and higher rate of adverse effects that led to discontinuation of therapy. Ceftaroline is a broad-spectrum cephalosporin with activity against MRSA, which has been approved by the FDA for CAP but not for CAP caused by MRSA or for HAP, VAP, or HCAP. Tigecycline is a broad-spectrum antibiotic with activity against MRSA. It has been approved by FDA for SSTI and IAI caused by MRSA. It has also been approved for CAP but not for CAP caused by MRSA or for HAP. In September 2010, the FDA issued a safety announcement regarding an increased mortality risk associated with the use of tigecycline compared with other drugs observed in a pooled analysis of 13 trials. The increased risk was seen most clearly in patients treated for HAP, particularly VAP. In 2013, FDA added boxed warning in reaction to additional analysis showing an increased risk of death associated with tigecycline use. The boxed warning states that tigecycline should be reserved for use in situations when alternative agents are not suitable. In an analysis of 10 clinical trials conducted for FDA-approved uses (CAP, complicated skin and skin structure infections, complicated intraabdominal infections), tigecycline was associated with increased mortality compared with other antibacterial agents (2.5 vs. 1.8%, adjusted risk difference 0.6%). Most deaths resulted from worsening infections, complications of infection, or underlying comorbidities. 6. 7. 8. RCT of patients with HAP and meta-analysis of randomized trials have shown similar results. In RCT of 945 patients with HAP, tigecycline with or without ceftazidime was compared to imipenem-cilastatin with or without vancomycin. In the clinically evaluable population, the cure rate for tigecycline was significantly lower than for imipenem (68 vs. 78%). Cure rates in clinically evaluable patients with VAP were 48% for tigecycline and 70% for imipenem. Cure rates for MRSA infection in patients with HAP or VAP were 44% for tigecycline and 77% for imipenem plus vancomycin. A 2012 meta-analysis of 10 published and 3 unpublished randomized non-inferiority trials also found that tigecycline was associated with absolute mortality increase of 0.7% compared with other agents. In addition, tigecycline was associated with absolute increase in non-cure rate of 2.9%. These effects were not isolated to specific type of infection or comparator antibiotic regimen. Ceftobiprole is broad-spectrum cephalosporin with activity against broad range of gram-positive bacteria (including MRSA and penicillin- and ceftriaxone-resistant pneumococci) and GNB. It has not been approved by the FDA, but it has been approved in Europe for treatment of HAP and CAP but not VAP. In trial of patients with HAP, 781 patients with HAP (including 210 with VAP) were randomly assigned to receive either ceftobiprole or linezolid plus ceftazidime. In ITT population, overall cure rates for ceftobiprole vs. linezolid plus ceftazidime were similar (50 vs. 53%). Cure rates in HAP (excluding VAP) patients were also similar (60 vs. 59%). However, cure rates in VAP patients were substantially lower in those who received ceftobiprole (23 vs. 37%). Microbiologic eradication rates in HAP (excluding VAP) patients were 63 vs. 68% (microbiologically evaluable [ME]) and in VAP patients were 30 vs. 50%. The authors proposed that substantial heterogeneity in baseline characteristics of the VAP patients is the most likely explanation for lower cure rate for ceftobiprole in VAP. Exploratory analyses suggested that young age and head trauma in VAP patients and high baseline calculated creatinine clearance were associated with poor outcomes in ceftobiprole-treated patients. C. Methicillin-susceptible Staphylococcus aureus i. If sputum culture reveals MSSA, empiric therapy for MRSA should be replaced with nafcillin (2 g IV Q4H) or oxacillin (2 g IV Q4H). D. Gram-negative pathogen i. Although combination antimicrobial therapy for HAP, VAP, and HCAP due to ii. iii. iv. v. gram-negative pathogens (especially Pseudomonas) is commonly administered, there is no conclusive evidence to support this practice. The best rationale for the use of combination therapy is to provide greater spectrum of activity when there is risk for MDR pathogens (if pathogen is resistant to one agent it may be susceptible to the other). Other commonly cited reasons for combination therapy include potential for synergistic efficacy as well as potential to reduce emergence of resistance. However, it is not clear that two agents offer improved outcomes for treating gram-negative pneumonia. A meta-analysis and subsequent RCT suggested that monotherapy of VAP was as effective as combination therapy. However, percentage of MDR organisms was low in trials reviewed in meta-analysis and in RCT. In addition, RCT excluded patients known to be colonized with Pseudomonas or MRSA and found that combination vs. monotherapy was associated with improved adequacy of initial antibiotics and microbiologic eradication of infecting organisms in patients who had infection due to Pseudomonas, Acinetobacter, and MDR GNB. Thus, it is difficult to extrapolate efficacy of monotherapy to ICUs with high incidences of these pathogens. In another study of patients hospitalized in ICU due to trauma, 84 patients with VAP caused by Pseudomonas were treated with monotherapy (cefepime 2 g Q8H); this resulted in microbiologic eradication (based on repeat BAL showing <103 organisms/mL) in 94% of patients with no recurrences, suggesting that combination therapy is unnecessary when initial antimicrobial therapy is active against isolate. In ICU settings in which ESBL are found, cephalosporins should be avoided as monotherapy due to selection of resistant organisms when these agents are used. The most reliable agent in this setting is carbapenem (imipenem-cilastatin, ertapenem, or meropenem). In 2014, FDA approved revisions to doripenem label warning clinicians about increased mortality rates in patients who received doripenem rather than imipenem for VAP; these results come from RCT that was stopped early due to safety concerns. The trial compared doripenem administered as 1 g via four-hour infusion Q8H for 7 days to imipenem administered as 1 g over one hour Q8H for 10 days. In ITT population, 28-day all-cause mortality was higher among patients receiving doripenem (31 of 135, 23%) than in those receiving imipenem (22 of 132, 17%). Clinical response rates were also lower in doripenem arm. Possible reasons for this difference include shorter duration and lack of loading dose of doripenem in setting of prolonged infusion and potential confounding due to use of adjunctive aminoglycoside. Doripenem has not been approved by FDA for treatment of VAP. vi. Two novel cephalosporin-β-lactamase inhibitor combinations, ceftolozane-tazobactam and ceftazidime-avibactam, have been approved the FDA for treating UTI and IAI but not pneumonia; both combinations have activity against many drug-resistant GNB. These agents may have utility for difficult to treat gram-negative pneumonia in future, but further study is necessary. E. Legionella i. Patients who have DM, renal disease, structural lung disease, or have been recently treated with glucocorticoids may require coverage for Legionella spp (azithromycin or fluoroquinolone). HAP and VAP due to Legionella spp are also more common in hospitals where organism is present in hospital water supply. F. Anaerobes i. Patients who have aspirated or had recent abdominal surgery may warrant coverage for anaerobes (clindamycin, β-lactam-β-lactamase inhibitor, or carbapenem). G. Anti-inflammatory effects of macrolides i. There has been interest in non-antibiotic anti-inflammatory effects of macrolides. RCT of 200 patients with sepsis and VAP showed that those who received clarithromycin (in addition to standard treatment including antibiotics) had significantly faster resolution of VAP (10 vs. 15.5 days) and weaning from mechanical ventilation (16 vs. 22.5 days) compared with those who received placebo. Among those who died of sepsis, time to death was significantly prolonged 3. in those who received clarithromycin. Confirmation of these findings in another trial is necessary before recommendations should be made about using macrolide in patients with VAP. Empiric treatment A. We generally agree with ATS/IDSA guidelines for management of HAP, VAP, or HCAP. These guidelines can be accessed through ATS website. Knowledge of predominant pathogens, and particularly their susceptibility patterns, should greatly impact choice of empiric therapy; in some cases, appropriate regimen will differ from regimens recommended in ATS/IDSA guidelines. B. No known multidrug resistance risk factors i. We suggest one of following IV antibiotic regimens for empiric coverage of HAP and VAP in patients with no known risk factors for MDR pathogens. 1. Ceftriaxone (2 g QD) 2. Ampicillin-sulbactam (3 g Q6H) 3. Levofloxacin (750 mg QD) or moxifloxacin (400 mg QD). When patient is able to take oral medications, either agent may be administered orally at the same dose as that used for IV administration. 4. Ertapenem (1 g QD) ii. Choice of specific agent for empiric therapy should be based on knowledge of prevailing pathogens (and susceptibility patterns) within healthcare setting. If there is concern for GNB resistant to above options (Enterobacter spp, Serratia spp, Pseudomonas spp) based upon microbiologic data at specific institution, we feel that it is reasonable to initiate piperacillin-tazobactam (4.5 g IV Q6H) or another agent (cefepime or anti-pseudomonal carbapenem [imipenem, meropenem]) as monotherapy for patients without known risk factors for MDR bacteria, provided that institution's susceptibility data support in vitro activity. C. Known multidrug resistance risk factors i. Host risk factors for infection with MDR pathogens include receipt of antibiotics within preceding 90 days, current hospitalization of ≥ 5 days, high frequency of ii. antibiotic resistance in community or in specific hospital unit, immunosuppressive disease and/or therapy, and presence of risk factors for HCAP. Traditional dosing 1. The traditional dosing of each agent is described in the following discussion, but extended infusions may be considered to optimize pharmacokinetics and pharmacodynamics, especially in critically ill patients. 2. An anti-pseudomonal cephalosporin such as cefepime (2 g Q8H) or ceftazidime (2 g Q8H) 3. An anti-pseudomonal carbapenem such as imipenem (500 mg to 1 g Q6H) or meropenem (1 g Q8H). 4. 5. 6. Piperacillin-tazobactam (4.5 g Q6H) For patients who are allergic to penicillin, type and severity of reaction should be assessed. The great majority of patients who are allergic to penicillin by skin testing can still receive cephalosporins (especially 3rd-generation cephalosporins) or carbapenems. If there is history of mild reaction to penicillin (not an IgE-mediated reaction, SJS, or TEN), it is reasonable to administer cephalosporin or anti-pseudomonal carbapenem using simple graded challenge (give 1/10 of dose, observe closely for one hour, then give remaining 9/10 of dose, observe closely for one hour). Skin testing is indicated in some situations. If skin test is positive or if there is significant concern to warrant avoidance of cephalosporin or carbapenem, aztreonam (2 g Q6H) is recommended. Indications and strategies for skin testing are reviewed elsewhere. Patients with past allergic reactions to cephalosporins may also be treated with aztreonam, with possible exception of those allergic to ceftazidime. Ceftazidime and aztreonam have similar side chain groups, and cross reactivity between the two drugs is variable. The prevalence of cross-sensitivity has been estimated at < 5% of patients, based upon limited data. 7. iii. Patients with past reactions to ceftazidime that was life threatening or suggestive of anaphylaxis (involving urticaria, bronchospasm, and/or hypotension) should not be given aztreonam unless evaluated by allergy specialist. In contrast, reasonable approach in those with mild past reactions to ceftazidime (uncomplicated maculopapular rash) would involve informing patient of low risk of cross reactivity and administering aztreonam with graded challenge (1/100, 1/10, full dose, each separated by 1 hour of observation). PLUS consider adding one of following (if microbiologic data from institution or patient's previous cultures suggest that one of following agents provides necessary additional coverage for GNB in combination with selected β-lactam). In light of results of several studies suggesting comparable outcomes with monotherapy compared with combination of GNB and potential for added toxicity of AMG, it may not be beneficial to add one of the following agents. 1. Anti-pseudomonal fluoroquinolone, preferred regimen if Legionella is likely, such as ciprofloxacin (400 mg Q8H) or levofloxacin (750 mg QD). These agents may be administered orally when patient is able to take oral medications. The dose of levofloxacin is same when given intravenously and orally, while dose of ciprofloxacin is 750 mg orally twice daily. 2. Aminoglycoside such as gentamicin or tobramycin (7 mg/kg QD) or amikacin (20 mg/kg QD); once-daily dosing is only appropriate for patients with normal renal function. A single serum concentration should be obtained 6 to 14 hours iv. after first dose, and dose should be adjusted as needed based upon following nomogram. AMG can be stopped after 5 to 7 days in responding patients. 3. Addition of alternative agent, such as colistin, may be appropriate if highly resistant Pseudomonas spp, Acinetobacter spp, Enterobacteriaceae (including K. pneumoniae) is suspected or established. In some cases, inhaled colistin may be appropriate as adjunctive therapy in combination with systemic antimicrobials, as discussed below. 4. For patients with pan-resistant GNB, consultation with specialist with expertise in antimicrobial management of such infections is recommended. PLUS ONE of following (if MRSA is suspected, there are MRSA risk factors, or there is high incidence of MRSA locally) 1. Linezolid (600 mg Q12H) 2. Vancomycin (15 to 20 mg/kg every 8 to 12 hours for patients with normal renal function, with target serum trough of 15 to 20 mg/L). In seriously ill patients, loading dose of 25 to 30 mg/kg can be used to facilitate rapid attainment of the target trough concentration. 3. Telavancin (10 mg/kg IV every 24 hours) is an alternative agent when neither linezolid nor vancomycin can be used, but there are several boxed warnings that must be considered before choosing it. 4. v. If patients have recently received antibiotics, empiric therapy should generally be with drug from different class since earlier treatment may have selected pathogens resistant to initial class. Extended infusion 1. Because of increasing resistance of pathogens associated with VAP, HAP, and HCAP, one potential strategy to enhance antimicrobial potential of given agent is to optimize pharmacodynamic effect. Based upon pharmacokinetic and pharmacodynamic properties of each agent, optimization of antimicrobial effect can be achieved with increased doses (for concentration-dependent antibiotics such as aminoglycosides and fluoroquinolones) or with prolonged or continuous infusions (for time-dependent antibiotics such as β-lactams). 2. 3. 4. 5. 6. 7. 8. Such regimens can potentially provide effective therapy for pathogens with higher MIC, may impede emergence of resistance, and potentially provide pharmacoeconomic benefit. Extended infusions are generally more practical than continuous infusions, since dedicated IV catheters are required for continuous infusions. Since β-lactams are associated with optimal outcomes when level of drug is above MIC for pathogen for appropriate percent of dosing interval, this effect can potentially be improved with prolonged infusion of antimicrobial. This has been demonstrated with use of 3 to 4 hour infusion of piperacillin-tazobactam, cefepime, or meropenem, for treatment of VAP due to GNB with higher MICs than usual breakpoints for susceptibility. An extended infusion of doripenem has also been evaluated, but we do not recommend it because it has been associated with increased mortality in one study of patients with VAP. An extended infusion of imipenem is also not appropriate because it does not remain stable for prolonged periods. Dosing guidelines for extended infusions have not been published; we use the following dosing regimens for empiric use of extended infusions of piperacillin-tazobactam, cefepime, and meropenem based on pharmacokinetic/pharmacodynamic modeling. For patients with normal renal function, we use the following initial dosing. Piperacillin-tazobactam – 3.375 or 4.5 g infused IV over four hours, administered every eight hours. An alternative to the extended infusion is to administer piperacillin-tazobactam as a continuous infusion of 18 g IV over 24 hours, in which case we recommend an initial loading bolus dose of 3.375 or 4.5 g administered over 30 minutes. Meropenem – 1 or 2 g infused IV over 3 hours, administered Q8H Cefepime – 2 g infused IV over 3 hours, administered Q8H The patient can be transitioned to traditional dosing if MIC is low. Dose adjustments for CKD are summarized in following Table (table 1). 9. In 2013 meta-analysis of observational studies and RCT, patients with pneumonia receiving extended or continuous infusion of carbapenem (mostly meropenem) or piperacillin-tazobactam had lower mortality than patients receiving intermittent bolus dosing (RR 0.5), although there were no differences in clinical cure (RR 1.13). Previously published meta-analyses that included only RCT did not detect difference in mortality between extended infusions and intermittent bolus dosing. A possible reason for this difference is that disease severity in RCT was low, which is reflected by low mortality rates in these studies. In contrast, many of patients in 2013 meta-analysis were critically ill patients with nosocomial pneumonia. Such patients might be more likely to benefit from extended infusions. 10. In separate Cochrane meta-analysis, which included 29 RCTs published between 1977 and 2012 of patients receiving antibiotics for severe acute infections (16 of which involved patients with pneumonia), there were no differences in mortality, infection recurrence, clinical cure, superinfection post-therapy, or safety outcomes when comparing continuous infusions of IV antibiotics to traditional intermittent infusions of antibiotics. However, utility for MDR pathogens or those with higher MICs was not well defined. 11. In RCT of 60 patients with severe sepsis (nearly half of whom had pneumonia) that was published after the 2013 meta-analysis was performed, plasma antibiotic concentrations exceeded the MIC in 82% of patients who received a continuous infusion of piperacillin-tazobactam, meropenem, or ticarcillin-clavulanate compared with 29% of patients who received intermittent bolus dosing. The rate of clinical cure was significantly higher in those who received continuous infusion compared with those who received intermittent bolus dosing (70 vs. 43%). There was non-significant trend toward increased survival to hospital discharge in patients who received continuous infusion (90 vs. 80%), but this study was not powered to detect survival benefit. 12. In single-center study of extended infusion of cefepime, piperacillin-tazobactam, or meropenem (administered over 3 hours) for suspected GNB infections in critically ill patients, many of whom had pneumonia, there was no advantage compared with intermittent infusion with regard to treatment success, mortality, or length of hospital stay. The paucity of isolates with elevated MICs in this study may in part explain lack of benefit of extended infusion. 13. Prolonged infusions of β-lactam antibiotics are discussed in greater detail separately. vi. Aerosolized antibiotic 1. Aerosolized colistin, polymyxin, or AMG may be considered as potential additional antibiotics in patients with MDR GNB. Aerosolization may increase antibiotic concentrations at site of infection and may be particularly useful for treatment of organisms that have high MICs to systemic antimicrobial agents. In randomized trial that included 100 patients with VAP due to GNB (predominantly MDRAB and/or P. aeruginosa), patients who were treated with combination of systemic antibiotics and nebulized colistin had higher rate of favorable microbiologic outcome compared with patients who were treated with systemic antibiotics alone (microbiologic eradication or presumed eradication 61 vs. 38%), but there was no differences in clinical outcome (51 vs. 2. 3. 53%). In retrospective case-control study that included 86 patients with VAP due to MDR gram-negative bacilli (predominantly A. baumannii) treated with combination of IV and aerosolized colistin compared with IV colistin alone, there was only trend toward improved rates of clinical cure, pathogen eradication, and mortality in the patients who received aerosolized and IV colistin. However, this study may have been underpowered to show benefit, adequate doses of aerosolized colistin may not have been used, and difficulty in diagnosing VAP may have biased the results (if patients without VAP were included). In meta-analysis that included seven observational studies and one RCT comparing aerosolized colistin administered with IV colistin to IV colistin alone in treatment of VAP, there was improvement in clinical outcome and microbiologic eradication associated with aerosolized colistin, but level of evidence was low. In trial that included 37 patients with VAP due to P. aeruginosa, patients were randomly assigned to receive either ceftazidime plus amikacin administered intravenously (ceftazidime 90 mg/kg per day via continuous infusion for 8 days plus amikacin 15 mg/kg daily for 3 days) or by aerosolization (ceftazidime 15 mg 8 times daily for 8 days and amikacin 25 mg/kg daily for 3 days). Bacterial eradication occurred more often and more rapidly in patients who received aerosolized antibiotics. However, no significant clinical differences were detected between the treatment groups, which may have been due at least in part to the small number of patients. Clinical success was achieved in 70% of the aerosolized antibiotic group and 55% of the IV antibiotic group. No antibiotic resistance developed in patients who received aerosolized antibiotics, but 3 patients who received IV antibiotics developed resistance to ceftazidime. There were three adverse events related to obstruction of respiratory filter in aerosolized antibiotic group; one of these resulted in nonfatal cardiorespiratory arrest. 4. Tailoring regimen A. When etiology of HAP, VAP, or HCAP has been identified based upon reliable B. 5. microbiologic methods and there is no laboratory or epidemiologic evidence of coinfection, treatment regimens should be simplified and directed to that pathogen. The choice of specific agents will be dictated by results of susceptibility testing. It is important to avoid broad-spectrum therapy once pathogen has been identified. S. aureus and GNB are easy to grow in culture. Thus, if these organisms are not isolated from good quality sputum specimen, coverage for MRSA and MDR GNB can be discontinued. Patients who are improving clinically, are hemodynamically stable, and are able to take oral medications can be switched to oral therapy. If pathogen has been identified, the choice of antibiotic for oral therapy is based upon the susceptibility profile for that organism. If pathogen is not identified, choice of antibiotic for oral therapy is either same antibiotic as intravenous antibiotic or agent in same drug class, which achieves adequate lung penetration when administered orally. Duration A. The duration of therapy should be based upon clinical response. The standard duration of therapy in the past was 14 to 21 days in part because of concern for difficult to treat pathogens (Pseudomonas spp). However, shorter course could significantly reduce amount of antimicrobial drugs used in hospitals where emergence of resistant pathogens is concern. B. The following studies found that short-course treatment is effective. i. A prospective randomized multicenter trial of 401 patients with VAP compared outcomes following 8 vs. 15 days of treatment. All patients underwent bronchoscopy for quantitative cultures and were empirically treated with combination of anti-pseudomonal β-lactam plus either AMG or fluoroquinolone. Investigators were encouraged to change regimen to pathogen-directed treatment based upon culture results. ii. There was no significant difference between patients treated for 8 compared with 15 days in mortality or recurrent infection at 28 days; as expected, patients treated for eight days had more antibiotic-free days. Among patients who developed recurrent infections, MDR pathogens were isolated less frequently in those treated for eight days (42 vs. 62% for those treated for 15 days). Patients with VAP caused by NFGNB (Pseudomonas spp) had a higher pulmonary infection recurrence rate when treated for 8 vs. 15 days (41 vs. 25% with 15 days of treatment), although the number of patients who received an additional course of antibiotics was not different. In sub-analysis of 125 patients who had S. aureus isolated as pathogen, there was no significant difference based on treatment duration (8 or 15 days) for 28-day mortality or VAP recurrence; this was also the case when only VAP caused by MRSA was considered. iii. A 2011 meta-analysis that evaluated 508 patients with VAP showed that short (7 to 8 day) course of antibiotics compared with longer (10 to 15 day) course increased antibiotic-free days during 28 days following enrollment (OR 4.02) and reduced recurrence of VAP due to MDR pathogens (OR 0.44). However, for cases of VAP due to NFGNB, pneumonia recurrence was greater after short-course therapy (OR 2.18). The majority of patients included in meta-analysis derived from trial described above, and remainder were from two other smaller studies. ICU study evaluated clinical outcomes, including duration of treatment, following implementation of clinical guideline for the treatment of VAP compared with historical controls (patients with VAP treated prior to implementation of the guideline). The clinical guideline group had a shorter duration of antimicrobial therapy and was less likely iv. v. vi. vii. to have recurrent episode of VAP. An additional meta-analysis identified 4 RCTs comparing short-course fixed duration (7 to 8 days) with longer duration (10 to 15 days) regimens for VAP. This meta-analysis included two trials that were included in meta-analysis described above as well as two additional trials. No difference was found for 28-day mortality between short-course and long-duration regimens. There was increase in antibiotic-free days in favor of the short-course regimen; however, there was no difference in relapses between the groups, although a trend toward lower relapses was observed in the longer duration group. There were no differences in ventilator-free days, duration of mechanical ventilation, or length of ICU stay. A prospective study evaluated the ability of CPIS to determine duration of therapy for ICU patients with new pulmonary infiltrates (table 2). Patients were included in study if they had new-onset pulmonary infiltrates and CPIS ≤ 6. The patients were randomized to either control group (standard therapy) or to experimental group (intravenous ciprofloxacin 400 mg Q8H for 3 days). CPIS was reevaluated at 3 days and, in patients with CPIS ≤ 6, antibiotics were discontinued in experimental group. If the CPIS was > 6, ciprofloxacin was continued or antibiotics were changed based upon the microbiologic results. Significantly more patients in the control group received antibiotics beyond three days compared to those in the experimental group (90 compared with 28% in the experimental group). In addition to reduced antibiotic use, the experimental group was less likely to have colonization/infection with resistant organisms (15 compared with 35% of patients in the control group) and had trend toward lower mortality. Another relevant finding in the 2011 meta-analysis described above was that discontinuation strategies using procalcitonin led to reduction in duration of therapy without adversely affecting other outcomes, including mortality. C. Based upon these data, we recommend that all patients with HAP, VAP, or HCAP should be evaluated for clinical response and results of microbiologic studies after initial empiric antimicrobial therapy. If patient has improved after 48 to 72 hours and pathogen is isolated, antimicrobial therapy should be changed to pathogen-directed regimen based upon susceptibility pattern. We have found serial levels of procalcitonin useful in assisting in decision to discontinue antimicrobial therapy. If there has been good clinical response (including assessment of CPIS and procalcitonin results) by 48 to 72 hours, we generally continue therapy to complete total course of 7 to 8 days independent of microbial etiology. Longer durations are warranted for patients with other factors such as S. aureus bacteremia, concern for metastatic infection, or more severe disease. Based on study of S. aureus VAP discussed above, eight days of therapy may be adequate if 6. there is good clinical response early in course of appropriate therapy. If patient has improved and no pathogen is identified, we would narrow regimen, discontinuing therapy for Pseudomonas spp and MRSA. D. If patient has not improved and resistant pathogen is suspected, therapy should be changed to provide coverage for MDR pathogens until pathogen is identified, in which case pathogen-directed treatment should be chosen based upon the susceptibility pattern. In addition, failure to improve at 72 hours should prompt search for infectious complications, other diagnoses, or other sites of infection. Lack of benefit of statins A. HMG CoA reductase inhibitors (statins) appear to have anti-inflammatory properties, B. and some studies of patients taking statin chronically have suggested that they might reduce risk of infection, including pneumonia, and infection-related mortality. However, many of these studies had potential flaws, and other studies have not shown these benefits. Given potential benefits of statins suggested by some studies, multicenter RCT was performed to determine whether statin would reduce 28-day mortality in patients with VAP. Patients were randomly assigned to receive either simvastatin (60 mg once daily) or placebo, beginning on the same day as antibiotic therapy and continuing until ICU discharge, death, or day 28, whichever occurred first. The trial was stopped early for futility after enrollment of 300 patients because day 28 mortality was not lower in the statin group compared with the placebo group (21 vs. 15%; HR 1.45). In statin-naïve patients (majority of patients), day 28 mortality was 22% in statin group and 14% in the placebo group. There were no significant differences in day 14, ICU, or in-hospital mortality rates; duration of mechanical ventilation; or changes in Sequential Organ Failure Assessment (SOFA) score. PROGNOSIS 1. Despite high absolute mortality rates in HAP patients, mortality attributable to infection is 2. 3. 4. difficult to gauge. Many studies have found that HAP is associated with significant excess risk of death. However, many of these critically ill patients die from their underlying disease and not from pneumonia. Case-control studies estimate that the all-cause mortality rate for HAP and VAP is in range of 33 to 50%. In contrast, a systematic review of randomized trials for the prevention of VAP has estimated that attributable mortality of VAP is 9% (range 3 to 17%). In retrospective cohort study that used large inpatient database, mortality rates were 10% in patients with CAP, 19% in patients with HAP, 20% in patients with HCAP, and 29% in patients with VAP. In another study, HCAP was associated with higher in-hospital mortality rate than CAP (18 vs. 7%). Variables associated with increased mortality. A. Serious illness at the time of diagnosis (high APACHE score, shock, coma, respiratory failure, ARDS) B. Bacteremia C. Severe underlying comorbid disease D. Infection caused by an organism associated with multidrug resistance (eg, P. aeruginosa, Acinetobacter spp, and Enterobacteriaceae, including K. pneumoniae) E. Multi-lobar, cavitating, or rapidly progressive infiltrates on lung imaging F. Delay in the institution of effective antimicrobial therapy APACHE II score has been considered the best system to predict mortality in patients with VAP. A group of investigators has developed a simpler scoring system to predict mortality: the IBMP-10 score based on presence of immunodeficiency; SBP < 90 mmHg; multi-lobar infiltrates; PLT < 100,000; and > 10 days in hospital prior to onset of VAP. Based on point for each variable, the mortality rates for each score were: 0 to 2%; 1 to 9%; 2 to 24%; 3 to 50%; and 4 to 67%. In preliminary analysis, the authors indicated that this 5-point system was comparable with APACHE II in its ability to predict mortality in such patients.