MRSA: the ER, and the ER/ICU interface
advertisement

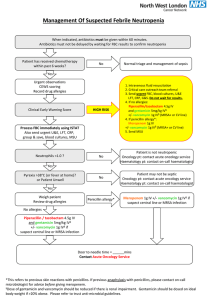
Skin and Soft Tissue Emergencies Dennis Djogovic MD, FRCPC Financial Disclosures None to declare Objectives When should skin infections be of special concern? Differential? Treatment priorities? Case 1 23 previously healthy male presents to the ED with “spider bites” to his left lower leg Clinically stable vitals and appearance Medical Hx: benign Social Hx: lives at home. Competitive wrestler Non systemic cellulitis PO Abx Evidence based choices are poor Retrospective analyses O/E: Chest/abd exam normal Lower left leg Normal pulses, sensation, strength 10-20 small pustules (<1mm in size), mild surrounding redness, non painful Make sure you cover for Strep and Staph Staph Do you need to worry about MSSA or MRSA? PO Abx Choices Keflex Strep and MSSA Clinda Strep, MSSA, MRSA Amoxicillin Strep But not staph Septra, Doxycycline Staph (MSSA and MRSA) But not strep Linezolid MRSA background Methicillin (B lactamase) in use since 1959 Outbreaks of MRSA since the 1960s Hospital acquired Far more virulent Community acquired Less virulent (usually) Community prevalence increasing Incidence of MRSA in Different Settings MRSA per Ward, MSSA (N=818); MRSA (N=295) CAN-WARD WARD TYPE % OF ALL S. aureus ICU 15.7% Surgical Ward 9.2% Medical Ward 27.8% ER 24.2% Outpatient Clinic 23.1% Overall 26.5% MRSA tips Age <2 First nations Close proximity to many people Athletes Prisons Military Hospital Skin breaks IVDU Skin disorders Known colonizers Case 2 23 previously healthy male presents to the ED with “spider bites” to his left lower leg Treated with clindamycin, swab grew MRSA 5 days later, lesions not healing, and appears to have more cellulitis Appears clinically unwell HR 115, 125/70, 38.9C Erythema of lower leg Although not rapidly progressive What is the ideal parenteral therapy? Vancomycin Inhibits cell wall synthesis Fairly safe Very effective For now Greatest level of experience and knowledge Achieving ideal dose levels not easy MSSA cleared faster with B lactams than Vanc Tissue penetration variable Bone, CSF Linezolid Bacteriostatic Inhibits at ribosomal level Excellent tissue bioavailability IV or PO Linezolid Adverse effects Thrombocytopenia Anemia Lactic acidosis Above mostly in the prolonged use setting Serotonin syndrome Reversibly binds MOA, if added to serotonin agent Vanco vs Linezolid Linezolid versus vancomycin for the treatment of methicillin-resistant Staphylococcus aureus infections. Stevens DL, Herr D, Lampiris H, Hunt JL, Batts DH, Hafkin. Clin Infect Dis. 2002;34(11):1481 hospitalized adults with known or suspected methicillin-resistant Staphylococcus aureus (MRSA) infections linezolid (600 mg twice daily; n=240) or vancomycin (1 g twice daily; n=220) for 7-28 days. S. aureus was isolated from 53% of patients; 93% of these isolates were MRSA. Skin and soft-tissue infection was the most common diagnosis, 15-21 days after the end of therapy, no statistical difference between the 2 treatment groups clinical cure rates (73.2% of linezolid group and 73.1% in vancomycin group) microbiological success rates (58.9% linezolid group, 63.2% vancomycin group) similar rates of adverse event Case 3 62 yr old female presents with triage complaint of “blisters” Groan… Case 3 62 yr old female 2 day duration Now also in her mouth Rapidly worsening HR 120, BP 105/50, 38.4C, RR 26/min Blisters- Bad or just gross? Acuity? Sick? Localized or widespread? Mucus membranes? Patient Sick? Immunocompromised? Age? New meds? Blisters: tough or fragile? Mucous Membranes? HSV SJS/TENS Pemphigus vulgaris Pemphigus paraneoplastic Mucus membrane pemhigoid type of Bullous Pemphigoid Stevens-Johnson Syndrome/ Toxic Epidermal Necrolysis Syndrome (SJS/TENS) An acute, immunologically mediated desquamation disorder secondary to infectious or environmental exposure. Very uncommon. (1/500000) BUT it can lead to disastrous sequelae akin to a major burn. Mortality SJS – 10% Mortality TENS – 30% Risk Factors Any viral infection prior to triggering exposure, notably HIV+ Medication exposures Active malignancy Southeast Asian Ethnicity Early Prognostic Markers Age >40 Active Malignancy Tachycardia (>120) at presentation % TBSA desquamated Serum Bicarbonate <20mmol/L at presentation Uremia at presentation (>10mmol/L) Hyperglycemia at presentation (>14mmol/L) SCORTEN Prognostic Score SCORTEN Score Mortality 0-1 3.20% 2 12.10% 3 35.30% 4 58.30% 5 or more 90% Management Prompt identification and withdrawal of trigger. General principles of burn care. Appropriate fluid resuscitation Wound care/Debridement Steroids** IVIG** Mucosal / Ophthalmological involvement require appropriate specialist involvement. UAH Burn Unit-Suspected Trigger - Cefazolin Diltazem TMP-SMX Phenytoin Vancomycin Atorvastatin Lamogtridine Allopurinol Mycoplasma pneumonia 2 1 3 1 1 2 1 1 1 **Viral serology was sought on all patients with a diagnosis of SJS/TENS and was all non-contributory. Observations on Triggers The average time from onset of rash to stopping of medication was 10 days (range 2-30) Case 4 86 yr old male Dementia 2 week onset of blisters on arms, legs (creases) A few have popped/leaked over past day Bullous Pemphigoid versus Pemphigous Vulgaris PemphigoiD = Deep VulgariS = Superficial OR Vulgaris = vulgar = ugly = sick and bad! Refer early Not many acute therapies in the ED Maybe IV steroids? Make sure you are not missing infection!! If on a recent abx, use a different class (TENS?!) Case 5 Healthy 32 yr female Gardening yesterday, scratched left arm on fence Nightime fever Awoke with painful red rash on left arm Spreading HR 130, BP 90/50, O2 sat 91% VBG: 40/26/7.18/lactate 9 Necrotizing skin infections Necrotizing Fasciitis Myositis Cellulitis In common all of these patients are SICK Only the OR can really tell the difference Imaging? Ultrasound Not too helpful Can find abscess MRI Obtained from the ER?? May overexaggerate soft tissue involvment Imaging? Non contrast CT Looking for air If you see air, you have necrotizing infection If you don’t see air, this could still be necrotizing infection Get your surgeon to look Ideally in the OR! Treatment OR Antibiotics Pen G and Clindamycin +/-IVIG Take home points A few ideas on antibiotic choices Blisters, rashes, lesions Quick? Sick? Tick, tick, tick!! Thanks for your time! djogovic@ualberta.ca