Charnley-Kerboull Total Hip Replacement Long Term Results
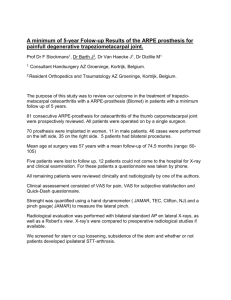
advertisement

Charnley-Kerboull Total Hip Replacement Long Term Results In Patients Younger Than 50 Results of a 30 years experience L Kerboull, M Hamadouche, M Kerboull. Long term results in patients under 50 • Reliability of THR outcome in young people is still being debated • The cemented metal/PE Kerboull system is now old and someone could think that it is no more indicated for young patients in the third millenium ? • Results published in CORR Jan 2004 The series • • • • • • 287 THR performed from 1975 to 1990 Randomly sorted from a cohort of 2804 patients Senior and junior surgeons 222 patients, 144 females and 78 males Mean age : 40,1 y ( ± 8 y ; 15,5 - 50 y). Mean weight : 63 kg (± 18,2 kg ; 37 – 116 kg) 180 300 160 140 250 120 200 100 80 60 40 115 172 20 150 100 50 0 Actif Inactif 0 ASA 1 ASA 2 ASA 3 ASA 4 The series : preoperative diagnosis 120 100 80 60 40 20 H ip S A A O rth N A e D rit cr is os is lo is ca tio n P 0 Se O O th pt A er ic s A rth rit is Previous surgery : 123 hips Operative Technique • Transtrochanteric approach • Charnley-Kerboull standard implants • Cup all poly • CMW type 1, mixed in air • Distal plug • Acetabular reconstruction in 92 hips Operative Technique : femoral implant Implants Surface design Section Neck Hips diamete r (mm) MK I Polished Quadrangular 13 139 CMK 2 Matt Oval 13 51 MK III Polished Quadrangular 10 27 CMK 3 Matt 10 70 Oval Polished 166 Matt 121 Methods • Merle d’Aubigné and Postel clinical scoring system • Cup : Charnley and Delee classification • Stem : Gruen and Amstutz classification • • • • Linear Wear : Chevrot and Kerboull M Cystic osteolysis Heterotopic ossifications Statistical analysis Methods : Modified Harris classification for radiological loosening Socket Femoral Stem Definite loosening Migration ≥ 3 mm and/or 3° Complete radiolucent line ≥ 2 mm Probable loosening Complete radiolucent line < 2 mm Subsidence ≥ 3 mm Cement mantle fracture Complete radiolucent line ≥ 2 mm Radiolucent line in Zone I ≥ 2 mm Complete radiolucent line < 2 mm Potential loosening Radiolucent line in 2 zones Radiolucent line in 2 zones Type of Loosening Mean follow-up : 14,5 years (± 5.1, 6m to 25 y) Status Mean follow-up (years) Number of hips Reviewed 16,1 ± 4,6 210 ( 73,2%) Died of 5,4 ± 3,1 unrelated causes 10 (3,5%) Lost to follow-up 10,8 ± 5,1 42 (14,6%) Revised 12,6 ± 6,1 25 (8,7%) 52 hips had a follow-up greater than 20 years Complications 3 non unions of the trochanter 1%, 1 reoperated 2 Deep infections, 1 acute treated by articular debridment and 1 chronic revised. 3 dislocations, 1 revised 1% 1 hematoma reoperated 3 heterotopic ossification grade 4, 1 reoperated 3 palsies of the peroneal nerve Clinical results : PMA score postop preop 60 250 50 200 40 150 30 100 20 10 50 0 0 0 2 4 6 8 10 12 14 16 18 20 Mean : 9,6 0 2 4 6 8 10 12 14 16 18 20 Mean : 17,4 83% of the hips rated excellent to very good Radiological results : Cup loosening No loosening Definite or Potential probable loosening loosening Wear > 0,1 mm/y Number of 238 hips 82,9% 15 5,2% 24 8,4% Radiological results : cup wear Mean femoral head penetration : 1,3 mm ± 1,5 mm (0 – 8 mm) 0,1mm/y 196 hips 91 hips 0.02 mm/y versus 0.28 mm/y P < 0.0001 8 ans Wear related factors Normal versus abnormal wear Factor P value Factor P value Age 0,7 Follow-up 0,5 Sexe ratio 0,2 Diagnosis 0,1 Activity 0,34 Cup position 0,8 Weight 0,9 Osteolysis 0,0001 Year of surgery 0,0001 Surgeon 0,5 1979 : 0,095 mm/an 1980 : 0,158 mm/an Intrinsic properties of PE was the main related factor These changes were due to manufacturing process variations PE Quality is the main factor Bilateral cases 17 y 18 y Radiological results : Stem loosening Number of hips No loosening Definite or Potential probable loosening loosening 271 95,1% 12 4,2% 4 0,7% osteolysis 10 aseptic, 1 septic, 1 after a periprosthetic fracture Radiological loosening : stem Implants design Surface Section Aseptic loosening Hips MK I Polished Quadrangular 1 139 CMK 2 Matte Oval 2 51 MK III Polished Quadrangular 0 27 CMK 3 Matte Oval 7 70 Matt vs Polished : p = 0,0001 Matt or polished surface ? Square or rounded cross section ? Mechanical basis Fact: - Bone, cement and stem form a composite - All mentioned materials have different E-Moduli Cortex: PMMA: WHN Stainless Steel - All material deform differently under load this leads to micro motions 12 - 18 Gpa 1.8 Gpa 250 Gpa Why the polished stem became matt ? •Initiation of stem loosening: debonding of the cement to prosthesis interface Improvement of the bond through a matt surface But ……… With a Matt surface Bone – No relative movement between stem and cement possible – Micromotions result in localy debonded areas at the bone cement interface which create an abrasive medium that induce osteolisys While a polished surface Bone Allowes micro movements in the stem to cement viscoelastic interface that protect the bone cement interface Does a polished cimented stem always subside ? Subsidence: Unlike other stems the CMK is not designed to subside and does not subside. « The French paradox »: Langlais, Ling, Kerboull, Sedel. JBJS Br, 2003. Why ?? - We choose the stem which best fills the medullary canal there is no space for the stem to subside. - The collar decreases the distal force applied to ciment plug - The stem does not get loose due to the cohesion forces acting on the two polished (cement/stem) surfaces. Round or Rectangular cross section ? Stems are prone to relative rotation when torque forces are applied Rounder cross section – Prevents hook stresses at the angle – But Increased shear stresses at the interface Rectangular cross section – Might induce hook stresses – Applies compressive stresses on the cement Round vs Rectangular a M2 F1a M1 M1 F1b b shear stress compressive stress cross section design ? The cross section is very delicate: Too round results in problems Too edgy might result in problems (increased hoop stresses) Look for a compromise Almost rectangular with smooth angles What was the most deleterious change Matt surface or rounded cross section Ra 0.9 m (35 inch) MK 2 : 4 % at 15 Y. Ra 1.7 m (67 inch) CMK 3 : 21 % at 10 Y. Matt surface Revisions : 25 Loosening or wear : 22 7 loosened stems 10 loosened cups 5 worn cups Other : 3 1 septic 1 recurrent dislocation 1 femoral fracture Suvival rate % Survival rate : revision 1 ,8 ,6 ,4 ,2 0 20 years 85,4% 95% sup : 92,4 % 95% inf : 78,4 % 0 5 10 15 20 25 30 Follow-up years Survival rate : cup loosening age NS Survival rate : stem loosening age NS Survival rate : stem loosening, surface finish Suvival rate % 1 96,4% 88,5% ,8 ,6 P= 0,0001 ,4 matt polished ,2 0 0 5 10 15 20 25 30 Follow-up years Suvival rate % Survival rate : wear dependant 1 Wear <= 0,1 94,8 % ,8 ,6 Wear > 0,1 70,6 % P = 0,002 ,4 ,2 0 0 5 10 15 20 25 30 Follow-up years What we learnt at the end of this study • The Kerboull cemented prosthesis could provide satisfactory and durable results for 20 years in 85 % of patients younger than 50 years. • So in our mind it remains a good solution, specially for young patient when anatomic and bony conditions are disturbed. • PE wear, when higher than 0.1 mm/y, is the only unsolved problem. • PE wear is mainly influenced by PE intrinsic qualities • Surface of a cemented stem must be definitely polished to protect cement and bone from excessive stresses. Do we need different implants for young people? • When we change implant, we also experiment new problems and our rate of failure increases compared with our routine technique • So we must change for a good reason – Bearing surfaces : may be – Type of fixation : definitely no , except if imposed by the mechanical properties of the bearing surfaces • when using a new implant, If our operative technique is reliable don’t change it, if possible Conclusions • Proven designs are not numerous because a long time is necessary to evaluate a hip prosthesis • Before changing try to correct the identified problems • Fashion, experimental studies and marketing features are not always our best friends ! Thank you