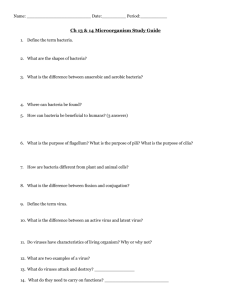
Path Chapter 8 p332-357 [4-20
advertisement
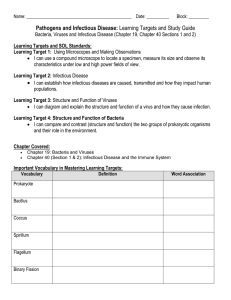
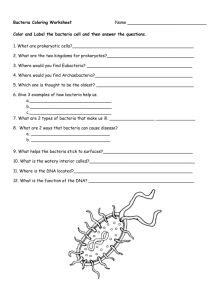
Path Chapter 8: Infectious Diseases (pages 332-357) Table 8-1 page 333 Prion – prions are made of abnormal forms of a host protein normally in neurons, called prion protein (PrP) - PrPs cause spongiform encephalopathis, like kuru (cannibals, scrubs!), Creutzfeldt-Jakob disease (CJD), bovine spongiform encephalopathy (made cow) Disease happens when the PrP does a shape change that makes it resistant to proteases The protease resistant PrP then promotes conversion of normal PrPs to this new form, which is why prions are infectious Accumulation of abnormal PrP leads to neuron damage and spongiform pathologies in the brain Virus – intracellular parasites that depend on host cell metabolic machinery for their replication - - Viruses consist of a nucleic acid genome surrounded by a protein coat called a capsid Viruses are classified by their nucleic acid genome(either DNA or RNA, but not both), shape of the capsid (helical or icosahedral), the presence or absence of a lipid envelope, how they replicate, the cell they like to replicate in (called tropism) Viruses can hang out in host cells for years, either continuing to multiply, or not replicate but have the ability to later (called a latent infection) Bacteria – prokaryotes (means they have a cell membrane but no nuclei and other membrane bound organelles) - - Most bacteria are bound by a cell wall made of peptidoglycan (sugar chain polymer linked by peptide bridges) o 2 types of cell walls in bacteria – pic page 334 Gram positive – thick cell wall surrounding the cell membrane, that retains crystal-violet stain Gram-negative – thin cell wall sandwhiched between 2 phospholipid bilayer membranes, that won’t stain crystal-violet Spherical bacteria are called cocci Rod shaped bacteria are called bacilli Bacteria that need oxygen are called aerobic, and those that don’t are called anaerobic Some bacteria have flagella – allow the bacteria to move Other bacteria have pili- surface projection that can attach bacteria to host cells or ECM Most bacteria make their own DNA, RNA, and proteins, but they depend on the host for favorable growth conditions Staph epidermidis and propionibacterium acnes (causes acne) are common bacteria on skin Bacteria in the mouth can cause tooth decay, especially strep mutans Intracellular bacteria, like chlamydia and rickettsia, replicate inside membrane-bound vacuoles, and get their ATP energy from the host cell - - Chlamydia trachomatis is the common infectious cause of female sterility (it scars and narrows fallopian tubes) and blindness (chronic inflammation of the conjunctiva leads to scarring and opacity of the cornea) Rickettsia injure the endothelial cells they grow in, causing hemorrhagic vasculitis often visible as a rash, and can also injure the CNS and cause death (rocky mountain fever) Mycoplasma bacteria are unique in that they don’t have a cell wall Fungi – eukaryotes that have thick chitin-containing cell walls, and ergosterol-containing cell membranes - - Fungi can grow either as round yeast cells, or as slender filamentous hyphae Hyphae may be septate (with cell walls separating individual cells) or aseptate Many important pathogenic fungi show thermal dimorphism, where they grow as hyphal forms at room temperature, but as yeast forms at body temp Fungi can produce sexual spores, or more often asexual spores called conidia Dermatophytes – fungi that cause superficial skin infection o These infections are termed “tinea” and then you name where in the body they are (ex: tinea pedis – athletes foot) In immunodeficient people, opportunistic fungi (candida, aspergillus, mucor, and Cryptococcus) can cause life threatening infections characterized by tissue necrosis, hemorrhage, and vascular occlusion, with little or no inflammatory response Protozoa – parasite protozoa are single-celled eukaryotes that are major causes of disease and death in developing countries - - Protozoa can replicate intracellularly or extracellularly Trichomonas vaginalis are protozoa parasites with flagella that are STI’s and can colonize the vagina and male urethra Intestine protozoa are gotten from ingestion of cysts from contaminated food or water The most common intestine protozoas, entamoeba histolytica and giarda lamblia, have 2 forms: o Motile trophozoites that attach to the intestinal wall epithelium and may invade o Immobile cysts that are resistant to stomach acids and are infectious when ingested Blood borne protozoa are transmitted by insects, which they replicate in before they’re passed to humans Helminthes – parasitic worms that are very differentiated and multicellular - - Most worms alternate between sexual reproduction in the definitive host, and asexual multiplication in an intermediary host or vector o So depending on the worm, humans can harbor adult worms, immature stages, or asexual larva forms Once adult worms live in humans, they don’t multiply, but make eggs or larva that are usually passed out in stool Often, the severity of worm disease depends how may worms are there - In some worms, disease is caused by inflammatory responses to the eggs or larva, instead of the adults (ex: schistosomiasis) Ectoparasites (arthropods) – insects (lice, bedbugs, fleas) or arachnids (mites, ticks, spiders) that attach to and live on or in the skin - They can cause disease by directly damaging the human host, or indirectly being vectors to pass infection to the human host (ex: deer ticks pass on lyme disease spirochete borrelia burgdorferi) Some arthropods cause itching and excoriations (skin abrasions) (ex: scabies – burrows) Special techniques to diagnose infectious agents – table 8-2 page 336 - - Acute infections can be diagnosed by looking for pathogen specific antibodies in the serum o The presence of a specific IgM antibody shortly after the onset of symptoms is often diagnostic Nucleic acid-based tests are called molecular diagnostics and commonly used o Ex: diagnosing HIV requires figuring out how much HIV RNA is there Nucleic acid amplification tests, like polymerase chain rxn (PCR) are common Giemsa stains – used to look for malaria, leishmania, and campylobacter Infectious agents in bioterrorism are ranked by the CDC – table 8-4 page 337 - - Category A – pose the highest risk and can spread from person to person easily, causing a high mortality rate o Ex: smallpox – easily spread in any environment, has a high mortality rate, and there is no antiviral therapy Smallpox spreads by direct contact with skin, or by contaminated clothes or bedding Symptoms show up after 7-17 days Starts with high fever, headache, and backache, followed by rash Category B – moderate in ease to spread, morbidity, and have low mortality Category C – new pathogens that could be engineered to spread easily and cause high morbidity and mortality Routes of entry for microbes – inhalation, ingestion, sexual transmission, skin breach - - The first defense against infection is intact skin and mucosal surfaces, which provide physical barriers and produce antimicrobial substances o In general, respiratory, GI, or GU infections in healthy people are caused by more virulent pathogens that can damage or penetrate epithelial barriers o Most skin infections in healthy people are caused by less virulent organisms entering the skin through a damaged site Skin – acts as a barrier, and has a low pH and fatty acids to inhibit growth of microorganisms other than normal flora o - - Skin is normally inhabited by some bacteria and fungi, including opportunists like Strep epidermidis and candida albicans o Dermatophyte fungi can infect the stratum, corneum, hair , and nails o Schistosoma larva can penetrate skin in water, by using collagenase, elastase, and other enzymes, to dissolve the ECM (fresh water snails!) o Most pathogens though penetrate through breaks in skin, like wounds, burns, and pressure related sites GI – most of these pathogens are transmitted by food or drink contaminated with fecal material o Areas with poor hygiene have high cases of diarrhea o Acidic gastric secretions are important defenses in the GI and lethal to many pathogens o Other defenses of the GI are the viscous mucus layer covering intestinal epithelium, pancreatic enzymes and bile detergents, mucosa antimicrobial peptides called defensins, normal flora, and secreted IgA antibodies IgA antibodies are made by plasma cells in mucosa associated lymphoid tissues (MALT) These lymph aggregates are covered by a single layer of specialized epithelial cells called M cells M cells are important for transport of antigens to MALT and for binding and uptake of gut pathogens o Host defenses are weakened by poor gastric acidity, antibiotics that affect the normal flora (like in pseudomembranous colitis), or in obstruction or stalled peristalsis o GI bacteria hurt us by: Certain staph grow on contaminated food, and release enterotoxins (HT) that cause food poisoning, without any bacterial multiplication V. cholera and E. coli (ETEC) multiply inside the mucous layer of gut epithelium, and release exotoxins that cause gut epithelium to secrete lots of fluid, causing watery diarrhea (cholera toxins) Shigella, salmonella, and campylobacter invade and damage intestinal mucosa and lamina propria, causing ulceration, inflammation, and hemorrhage, all seen as dysentery Salmonella typhi passes from damaged mucosa into the blood to cause systemic infection o Fungal infection of the GI happens mainly in immunocompromised people o GI protozoa must be in cyst forms, since the cysts resist stomach acid In the gut, the cysts convert to motile trophozoites, and attach to sugars on intestine epithelia o GI worms only cause disease when there is a lot of them or they block something Hookworms can cause iron deficiency anemia by chronic loss of blood sucked from intestine villi Respiratory tract – lots of organisms are inhaled daily, often in dust or aerosol particles o They only travel as far as their size lets them - Large particles are trapped in the mucociliary blanket that lines the nose and upper respiratory tract Inhaled microorganism are trapped in mucus secreted by goblet cells, and are tehn transported by ciliary action to the back of the throat, where they are swallowed and cleared Very small particle go right to the alveoli, where they get phagocytosed by alveolar macrophage or by recruited neutrophils o Some respiratory pathogens evade defense by attaching to epithelial cells int eh lower respiratory tract and pharynx Ex: flu virus has hemagglutinin proteins on the virus surface that bind to sialic acid on the surface of epithelial cells This induces the epithelial cell to engulf the virus, and the virus replicates in the epithelial cell Sialic acid also interferes with shedding of newly made viruses from the host cell, so flu virus also has neuraminidase, which cleaves sialic acid to allow virus release and also lowers the viscosity of mucus to allow better virus travel in the respiratory tract o Some respiratory pathogens impair ciliary activity Any damage to the cilia (like in smoking) will also make you susceptible to infection GU tract – the urinary tract is almost always invaded from the exterior via the urethra o The regular flushing of the urinary tract with urine is a defense against invaders o Urine in the bladder is normally sterile o Women have more urinary infections than men, because there’s a shorter distance for the infection to travel o From puberty to menopause, the vagina is protected from pathogens by a low pH resulting from catabolism of glycogen in the normal epithelium by lactobacilli Antibiotics can kill the lactobacilli and make the vagina susceptible to infection Spread of microbes: - Pathogens that cause superficial infections stay confined to the lumen of hollow viscera, or stick to or invade epithelial cells Most viruses spread from cell to cell by replication and release of infectious virions Sporadic blood invasion by low virulence or nonvirulent microbes is common (like in brushing your teeth) but quickly controlled by normal host defense Signs of system sepsis are fever and low blood pressure Release of microbes from the body: - Skin shedding, coughing, sneezing, urine or feces release, sex, or insect vectors, are all ways a microorganism can leave a host - Transmission from person to person can be done through the respiratory, fecal-oral, or sex routes Pathogens transmitted by the respiratory route are infectious only when lesions are open to airways Fecal-oral route – ingesting stool-contaminated water or food Viruses infecting the oropharynx are transmitted mainly through saliva Sexually transmitted infections (STI’s) – table 8-5 page 341 - - Organisms that cause STIs tend to be short-lived outside of the host, so the usually depend on direct person-to-person spread Most STIs can be infectious even if there’s no symptoms Infection with one STI increases the risk for another STI – since they have the same risk factors o Ex: chlamydia (chlamydia trachomatis) and gonorrhea (neisseria gonorrhoeae) happen so often together, if you see one, you should immediately treat for the other as well STIs can spread from a pregnant woman to the fetus and cause severe damage o HSV causes CNS disease, syphilils causes miscarriage, HIV can be fatal, chlamydia causes conjunctivitis Noscomical infections – infections caught in a hospital - The most common way they spread is by the hands of healthcare workers, or from contaminated hospital stuff o Need to wash your hands! Innate immunity – ready to go before infection takes place - Includes physical barriers, phagocytes, NK cells, complement 3 ways pathogens cause disease: - They contact or enter host cells and directly cause cell death They release toxins that kills cells They can induce a host immune response that also hurts host tissue Ways viruses cause injury: - - Viruses can directly damage host cells by entering them and replicating Tropism – viruses like to infect certain cells and not others o Tropism is determined by expression of host cell receptors for the virus, presence of cell transcription factors the virus can use, anatomic barriers, and local environment (pH, temp, etc.) Many viruses use normal host cell receptors to enter the cell o Ex: HIV uses CD4 on T cells o Sometimes a host protease is needed to change the virus a little to bind - A host cell needs to have the promoter and enhancer DNA sequences for the viral genes in order for the virus to replicate in that cell Ways a virus hurts host cells it infects: o Direct effects – viruses can prevent making of host DNA, proteins, etc.; make enzymes and toxic proteins to hurt the host, or cause apoptosis (by making pro-apoptotic stuff, or causing injury to the ER to release caspases) o The immune response against the virus – often by TC cells o Transformation of infected cells into benign or malignant tumor cells Ways bacteria cause injury: - - - - - Bacteria damage to host tissues depends on the ability of the bacteria to adhere to host cells, invade cells and tissues, or deliver toxins o Pathogenic bacteria have virulence genes that encode proteins to do this stuff o Virulence genes are grouped together in clusters called pathogenicity islands Plasmids and bacteriophage (bacteria viruses) are mobile genetic stuff that spreads between bacteria and can encode virulence factors, converting otherwise nonharmful bacteria into pathogenic bacteria Plasmids and transposons can adapt the bacteria genome so that it’s resistant to the host defense Bacteria can do quorum sensing, where they realize there’s lots of other bacteria with them, so they release stuff the others don’t, but will cause the others to release things to progress the infection, like toxins o This way, unicellular bacteria get to use ways to infect that they don’t normally have themselves Communities of bacteria can form biofilms, where they live in a viscous layer of extracellular polysaccharides, that adhere to host tissues or medical devices o Biofilms increase the virulence of a bacteria, by making them inaccessible to immune responses Bacteria use adhesin surface molecules to bind to host cells or ECM Pili – the amino acids at the tip determine what it will bind to, while the stalk is the same in every bacteria Intracellular bacteria infect either epithelial cells (shigella and E. coli), macrophage ( (M. tuberculosis, M. leprae), or both (S. typhi) o The growth of bacteria in the cell can let it escape from some immune defenses, like antibodies o It also helps them spread, like how macrophage can carry infection to other sites o Some bacteria use the host immune response to enter a macrophage Coating these bacteria with antibodies or complement C3b (called opsonization) will cause phagocytosis o Gram-negative bacteria rearrange host cell membranes to let them in They use needle-like structures on their surface - Any bacterial substance that adds to illness is considered a toxin o Two types of bacterial toxins: Endotoxin – parts of the bacterial cell Exotoxins – proteins secreted by the bacteria o Bacterial endotoxin – a lipopolysaccharide (LPS) that is a large part of the outer membrane of gram negative bacteria LPS is made of a long-chain fatty acid anchor (lipid A) connected to a core sugar chain Attached to the core is a variable carb chain (O antigen) that is used to diagnose and tell the difference between different bacteria Our response to LPS can help by inducing cytokines and chemokines, and increased expression of costimulatory molecules that enhance T cell activation If too many cytokines are activated through a lot of LPS, it can cause septic shock, DIC, and respiratory distress syndrome, by excessive TNF, Il-1 and Il-12 LPS binds to cell surface receptor CD14, and this complex then binds to tolllike receptor 4 (TLR4) o Types of exotoxins: Enzymes Toxins that change intracellular signaling – most of these have an active A subunit with enzyme activity, and a binding B subunit that binds receptors on the cell surface and delivers the A subunit into the cell cytoplasm Neurotoxins – inhibit release of neurotransmitters, causing paralysis They don’t kill neurons Superantigens – stimulate very large #’s of T cells by binding to the T cell receptor, causing massive T cell proliferation and cytokine release The high levels of cytokines can cause capillary leak and shock Superantigens made by staph aureus and strep pyogenes cause toxic shock syndrome (TSS) Ways microbes evade the immune system: - - They can grow in places that the immune system can’t get to o Ex: replication in the lumen of the intestine or gallbladder o Others invade a host cell so quick there’s no time for the humoral response to react o Large parasites form cysts in host tissues covered by a dense capsule that immune cells and antibodies can’t get through They do antigenic variation – changing the antigens that are expressed, using mutations or genetic recombination They’re resistant to innate immunity o Cationic antimicrobial peptides (like defensins, cathelicidins, and thrombocidins) provide important initial defense against invading microbes Resistance these is key for a bacteria to be virulent o - - The carb capsule on the surface of all major bacteria that cause pneumonia or meningitis, makes them more virulent by shielding bacterial antigens and preventing phagocytosis o Many bacteria make toxic proteins that kill phagocytes, prevent their migration, or prevent release of reactive oxygen species o Bacteria can also cover themselves in host proteins They immunosuppress the innate immune system – by making things to inhibit it o Some viruses make things to block complement activation and interferons They can make soluble homologues of IFN-α, β, and γ receptors, that bind to and inhibit secreted IFNs (decoy receptors) Can also make proteins that inhibit JAK/STAT signaling Some microbes make things that decrease recognition of infected cells by CD4+ TH cells and CD8+ TC cells o Ex: some viruses bind to or mess with MHC1s, impairing presentation to CD8 T cells o Things like that are recognized by NK cells, so they also make homologues for NK cells to see and leave them alone People with antibody deficiency are susceptible to severe bacterial infections People with T cell defects are susceptible to infections with intracellular pathogens, mainly viruses and parasites People with problems with complement are susceptible to infections by strep pneumonia, H. influenza, and N. meningitides HIV infects and eventually kills CD4+ TH cells, causing huge immunosuppression and prone to infections Diseases that impair making of leukocytes, like leukemia which fills the bone marrow with cancerous cells, makes patients vulnerable to opportunistic infections Therapy to prevent rejection of an organ after transplant will lower the immune system, increasing the risk for infection Patients receiving bone marrow transplants have big defects in innate and adaptive immunity during the long time it takes for the donated bone marrow to engraft People with cystic fibrosis often get respiratory infections with P. aeruginosa and staph aureus Sickle cell impairs spleen function, making them susceptible to infection with encapsulated bacteria like strep pneumonia, which usually get opsonized and phagocytosed by spleen macrophage There are only a limited # of tissue responses to microbes: - Suppurative (purulent) inflammation – the rxn to acute tissue damage o - - - Suppurative inflammation is characterized by increased vascular permeability and WBC infiltration, mainly by neutrophils o Neutrophils are attracted to the site of infection by release of chemoattractants from the pyogenic (pus-forming) bacteria that evoke this response (mostly extracellular gram positive cocci, and gram negative rods) o Liquefactive necrosis and all the neutorphils form pus Mononuclear and granulomatous inflammation – acute response to intracellular pathogens o Which mononuclear cell predominates the inflammatory lesion depends on the immune response to the organism (ex: plasma cells dominate inflammation against extracellular stuff) o Granulomatous inflammation – resistant stuff triggers a mononuclear infiltrate of macrophage that wall it off Characterized by accumulation of activated macrophage called epitheliod cells, which can fuse to form giant cells Cytopathic-cytoproliferative rxn – usually in response to a virus o The lesions are characterized by cell necrosis or cell proliferation, with few inflammatory cells o So the tissue is told to either die or proliferate o This includes viruscancer rxns, inclusion bodies, blisters and warts Tissue necrosis – necrosis is so rapid and severe that tissue necrosis is the dominant feature o Few inflammatory cells are present, so necrotic lesions look like infarcts Chronic inflammation and scarring - can lead to either complete healing, or scarring Acute (transient) viral infections: - The virus triggers an effective immune response that gets rid of the organism Measles (rubeola) virus o Measles is the leading cause of vaccine-preventable death and illness in the world o Kids in developing countries have poor nutrition, and so are much more likely to die of measles-caused pneumonia than kids in developed countries o Measles virus is a single-stranded RNA virus that’s part of the same family as mumps, croup, and lower respiratory infections, called paramyxovirus o Measles has only two cell surface receptors: CD46 – inactivates C3 convertases of complement Signaling lymphocytic activation molecule (SLAM) – works in T cell activation CD46 is expressed on all nucleated cells, while SLAM is expressed on cells of the immune system Both receptors bind the virus hemagglutinin protein o Measles is transmitted by respiratory droplets o Measles first multiplies int eh upper respiratory epithelial cells, and then spreads to local lymph tissue - - Measles can replicate in epithelial cells, endothelial cells, phagocytes, and lymphocytes o Replication of measles in the lymph then leads to its spread to many body tissues o Measles can cause croup, pneumonia, diarrhea, keratitis with scarring and blindness, encephalitis, and hemorrhagic rashes (black measles) o Most kids develop T cell immunity to measles virus, that controls the infection and causes measles rash (hypersensitivity rxn to measles infected cells in the skin) Measles rash looks blotchy, reddish brown, and is on the face, trunk, or extremities It’s caused by dilated skin vessels, edema, and mononuclear inflitrate o Antibodies against measles will protect against reinfection o Measles can also cause transient immunosuppression, allowing for secondary infections that cause much of the morbidity and mortality of measles o Measles shows mucosa ulcers in the oral cavity near the stensen ducts The ulcers are marked by necrosis and a neutrophil filled exudate o Giant cells in measles are called Warthin-Finkeldey cells, and have eosinophilic nuclear and cytoplasm inclusion bodies Mumps – another paramyxovirus o Mumps has 2 types of surface glycoproteins: one with hemoagglutinin and neuraminidase, and one with that does cell fusion and cytolytic activities o Mumps virus enters the upper respiratory tract through inhalation and respiratory droplets, spreads to draining lymph nodes where they replicate in lymphocytes (usually activated T cells) and then spread through the blood to body glands (especially salivary) o Mumps virus infects salivary gland duct epithelial cells, causing desquamation of infected cells, edema, and inflammation, that cause the classic salivary gland pain and swelling of mumps o Aseptic meningitis is the most common complication of mumps outside the salivary glands (happens 1/10 the time) o Mumps parotitis causes salivary glands to be enlarged, feel doughy, and be moist, glistening, and reddish brown The salivary glands will be edematous and infiltrated by macrophage, lymphocytes, and plasma cells, which all compress the ducts o Mumps orchitis – causes testicle swelling from edema and hemorrhage Since the testes are enclosed, swelling can cut off blood supply and cause infarction This can lead to scarring that causes them to be sterile Poliovirus – spherical unencapsulated RNA enterovirus o There’s 3 forms of polio, and all of them are vaccinated against o Now polio is basically eliminated in the western hemisphere, because polio only infects people and not animals, is only briefly shed, and doesn’t do antigenic variation o Poliovirus is transmitted fecal-oral, and infects the oropharynx, gets secreted into saliva and swallowed, and then multiplies in the intestines and lymph nodes, causing fever - - o Poliovirus only infects humans because it uses human proteins to enter human cells o Most polio infections are asymptomatic, but rare cases can invade the CNS West nile virus – an arbovirus (arthropod borne virus) transferred by mosquitoes to birds and mammals o Birds are the reservoir for the virus o Once transferred from mosquito to the skin dendritic cells, it replicates in them, and then migrates to lymph nodes, where it replicates more, then enters the blood, and can cross the blood brain barrier into the CNS to infect neurons o In healthy people, chemokines direct WBCs to the CNS to clear a virus The host chemokine receptor CCR5 is essential to resist CNS invasion Homozygous mutations to the CCR5 gene allow for lethal west nile virus infection, but protects against HIV because HIV uses CCR5 to infect host cells o West nile virus infection is usually asymptomatic, but in 1/5 of infections it causes a mild, short-lived febrile illness with headache and myalgia o A macule-papule like rash is seen in half of cases of west nile o Neuro symptoms are rare, but 10% of these patients die, and many of them have longterm neuro issues Viral hemorrhagic fevers (VHFs) – systemic infections caused by RNA viruses o Ex: ebola o They all depend on an animal or insect host for survival o Human’s aren’t the normal reservoir, and get infected when they encounter one of these hosts, but once a human gets it, it can be spread from person to person o They cause hemorrhages, thanks to thrombocytopenia and severe platelet or endothelial problems Chronic latent infections – these are the herpes virus infections - - Herpesviruses are large encapsulated viruses that have a double stranded DNA genome Herpesviruses cause acute infection followed by latent infection, where the virus persists in a noninfectious form, and can reactivate and be infectious again for a period 3 types of herpesvirus based on the cell they infect: o α-group herpesviruses – infect epithelial cells, and cause latent infection in neurons ex: HSV-1, HSV-2, and VZV (varicella zoster) o lymphotropic β-group herpesviruses – infect several cell types ex: CMV o γ-group viruses – cause latent infection mainly in lymph cells ex: EBV and KSHV/HHV-8 (causes Kaposi sarcoma) Herpes virus form a large nuclear inclusion surrounded by a clear halo Herpes simplex virus (HSV) o HSV-1 and HSV-2 differ serologically, but are genetically similar and cause a similar set of primary and recurrent infections o HSV causes acute and latent infections o o o o o o o o o o o o o Both HSVs replicate in the skin and mucous membranes at the site of entrance, usually the oropharynx or genitals There they make infectious virions and cause blistery lesions of the epidermis HSV spreads to sensory neurons that innervate these primary sites of replication The viral nucleocapsids are transported along axons to the neuron cell bodies, where the viruses cause latent infection During latency the viral DNA remains in the nucleus of the neuron, and only latencyassociated RNA transcripts (LATs) are made In this state, no viral proteins are made Reactivation of HSV may happen repeatedly with or without symptoms, and results in spread of virus from the neurons to the skin or to mucous membranes Herpesviruses can avoid immune recognition HSVs can evade antiviral TC cells by inhibiting MHC1 recognition HSVs can evade humoral immunity by making receptors for the Fc domain of immunoglobulin, and inhibitors of complement HSV-1 causes skin lesions, and is the major infectious cause of corneal blindness itn eh US, as well as the major cause of fatal sporadic encephalitis in the US when it spreads to the brain (especially temporal frontal lobes (think what happened to mike mccurdy) HSV infected cells have large, pink-purple inclusions in the nucleus that are made of virions that push host cell chromatin to the edge of the nucleus HSV also causes cells to fuse, producing inclusion-having multinuclei cells HSV-1 and HSV-2 cause lesions ranging from self-limited cold sores to life-threatening organ infections and encephalitis Cold sores (aka “fever blisters”) favor the skin around the mucosa of the lips and nose The intraepithelial vesicles (blisters) are formed by intracellular edema and ballooning degeneration of epidermal cells, and they often burst and crust over Stress can trigger fever blisters (herpes labialis) Gingivostomatitis – vesicular (blister) eruption extending from the tongue to the pharynx, and causes cervical lymphadenopathy Caused by HSV-1 and usually in kids Swollen erythematous HSV lesions of the fingers or palm are seen Genital herpes – vesicles (blisters) on genital mucous membranes and external genitalia, that rapidly convert into superficial ulcers rimmed by inflammatory infiltrate Genital herpes is more often HSV-2 than HSV-1 HSV can be transmitted to neonates during passage through the birth canal of infected moms In the child, HSV-2 infection has lymphadenopathy, enlarged spleen, and necrosis in many organs Two forms of corneal lesions are caused by HSV: Herpes epithelial keratitis – shows lysis of the superficial epithelium - Herpes stromal keratitis – shows infiltrates of mononuclear cells around keratinocytes and endothelial cells, leading to neovascularization, scarring, opacity of the cornea, and eventual blindness It’s an immune rxn to the HSV infection o Kaposi varicelliform eruption – generalized blisters on the skin o Eczema herpeticum – pustular hemorrhagic blisters often with bacterial infection and spread of HSV to organs o Herpes hepatitis can cause liver failure Varicella-Zoster Virus (VZV) – causes chickenpox and shingles o Acute VZV infections cause chickenpox o Reactivation of latent VZV causes shingles (aka herpes zoster) o Chickenpox is mild in children but more severe in adults and immunocompromised o Shingles usually gets the elderly and immunosuppressed o VZV infects mucous membranes, skin, and neurons, and causes a self-limited primary infection, just like HSV o Also like HSV, VZV evades immune responses and establishes a latent infection in sensory ganglia o VZV is transmitted by aerosols, and causes widespread blistery skin lesions o VZV infects neurons and/or satellite cells in the dorsal root ganglia, and can recur years after the primary infection, to cause shingles o Localized recurrence of VZV is most common and painful in dermatomes innervated by the trigeminal ganglia (CN5), where it’s most likely to exist in a state of latency o Unlike HSV, there is usually not a recurrence of VZV It will only recur once in healthy people In the immunosuppressed or elderly, it can recur several times o The chickenpox rash starts about 2 weeks after respiratory infection Lesions appear in waves from the torso to the head and extremities Each lesion progresses rapidly from a macule to a vesicle (blister), which resembles a “dewdrop on a rose petal” Chickenpox vesicles have intranuclear inclusions in epithelial cells like HSV-1 After a few days, most chickenpox blisters rupture, crust over, and heal by regeneration, leaving no scars However, bacterial superinfection of blisters that are ruptured by trauma can lead to destruction of the basal epidermal layer, & scarring o Shingles happens when VZV that has remained latent int eh dorsal root ganglia after previous chickenpox infection, is reactivated and infects sensory nerves that carry it to one or more dermatomes There, VZV infects keratinocytes and causes vesicular lesions (blisters) which, unlike chickenpox, often have intense burning, or sharp pain, because of simultaneous radiculoneuritis This pain is really bad when the trigeminal nerves (CN 5) are involved - Rarely, the geniculate nucleus is involved, causing facial paralysis – called Ramsay Hunt syndrome The sensory ganglia have a dense, mononuclear infiltrate, with herpes inclusions in neuron nuclei Cytomegalovirus (CMV) – a β-group herpesvirus that latently infects monocytes and their bone marrow progenitors, and can be reactivated when cellular immunity is depressed o CMV causes an asymptomatic or mono like infection in healthy people o CMV infected cells show gigantism of both the entire cell and its nucleus Within the nucleus is a large inclusion surrounded by a clear halo (owl’s eye) o Transmission of CMV: Congenital CMV - transplacental transmission from a new or primary infection in a mom who doesn’t have protective antibodies Perinatal CMV - neonatal transmission can happen through cervical or vaginal secretions at birth, or later through breast milk from a mom who has an active infection Transmission through saliva during preschool years After 15 years old, spread is most often through STD or fecal-oral and respiratory secretions Iatrogenic transmission through blood transfusions or transplants o Acute CMV infection induces transient but severe immunosuppression o CMV can infect dendritic cells and impair their maturation and ability to stimulate T cells o CMV can evade immune responses by downregulating MHC1 and 2s, and making homologs of the TNF receptor, Il-10, and MHC1s o CMV can both activate and evade NK cells, letting it hide from and suppress immune responses o Infected CMV cells are enlarged with basophilic intranuclear inclusions that take up half the nucleus, and separated from the nuclear membrane by a clear halo Other inclusions are seen in the cytoplasm as well o Congenital CMV infections - infection acquired in utero If mom has primary infection, which means no antibodies, it can cause cytomegalic inclusion disease, where they’re growth is retarded, they become ill, get jaundice, hepatospenomegaly, anemia, bleeding from thrombocytopenia, and encephalitis Fatal cases happen from microcephaly (small brain) and calcification Infants who survive often have permanent deficits, like mental retardation, hearing loss, and other neuro issues There’s also a milder form with just pneumonitis, hepatitis, or a hematologic problems, and the infant recovers o Perinatal CMV infections – infection gotten from passage through the birth canal or from breast milk Usually asymptomatic, but sometimes it can cause pneumonitis, failure to thrive, skin rash, or hepatitis o o o These kids will have acquired mom antibodies against CMV, which decreases how severe it is They’ll excrete the CMV for months to years, and may have hearing or intelligence issues later in life CMV mononucleosis – almost always asymptomatic in healthy people Around the world at least half of people have antibodies to CMV in their serum, meaning they were exposed at some point The most common clinical manifestation of CMV infection in healthy people after the neonatal period is an infectious mono-like illness, with fever, lymphocytosis, lymphadenopathy, and hepatomegaly, along with abnormal liver tests that suggest mild hepatitis Most people recover without issue, but may excrete the virus for months to years The virus then becomes latent in WBCs CMV in immunosuppressed people – can cause severe CMV infection Can be either primary or reactivation of latent infection CMV is the most common opportunistic viral pathogen in AIDs Serious life-threatening CMV infections mainly affect the lungs (called pneumonitis) and GI tract (colitis) The pneumonitis can progress to full-blown acute respiratory distress syndrome Intestinal necrosis and ulceration can develop and lead to formation of pseudomembranes and debilitating diarrhea Hepatitis B virus (HBV) – HBV is a chronic productive infection that causes viral hepatitis - HBV is spread percutaneously (IV), perninatally, and sexually HBV infects hepatocytes and cell injury happens from the immune response against it TC cells get rid of infected hepatocytes, but if more cells are infected than destroyed, you get a chronic infection Long term liver injury can lead to cirrhosis Sometimes the hepatocytes are infected but there’s no TC response against them, so they stay there in a “carrier” state Transforming infections are viruses that can cause cancer – includes EBV, HPV, HBV Epstein-Barr virus (EBV) – causes infectious mononucleosis - EBV can cause lymphomas and nasopharyngeal carcinoma Infectious mono is characterized by fever, lymphadenopathy, splenomegaly, sore throat, and atypically activated T cells called mononucleosis cells Some people develop hepatitis, meningoencephalitis, and pneumonitis Infectious mono happens mainly in young adults in developed nations - - - - o In the rest of the world it happens in asymptomatic kids EBV is transmitted by close human contact, often with saliva during kissing An EBV envelope glycoprotein binds to CD21 (CR2), the receptor for the C3d complement that’s on B cells Mono starts in the nasopharynx and oropharyngeal lymph tissues, especially in the tonsils EBV then enters the submucosal lymph tissues Here, in some B cells there is a productive infection with lysis of infected cells and release of virons, which can then infect other B cells o B cells are the main reservoir of latent infection During latent infection, a small # of EBV genes are expressed and help establish latency o Gene products are EBNA1, which binds the EBV genome to chromosomes, EBBNA2, and latent membrane protein 1 (LMP1), which drive B cell activation and proliferation o EBNA2 (EB nuclear antigen 2), stimulates transcription of many host genes including genes that drive cell cycle entry Activated B cells then spread and secrete antibodies, including anti-sheep RBC antibodies used to diagnose mono The symptoms of mono show up on initiation of the host immune response o TC cells and NK cells are the main response o The atypical lymphocytes in the blood characteristic of mono are EBV specific CD8+ TC cells, and some CD16+ NK cells o The reactive proliferation of T cells is mainly in the lymph tissues, which explains the lymphadenopathy and splenomegaly o Early in the infection, IgM antibodies are formed against viral capsid antigens o Later, IgG anitbodies are formed that last for life o In healthy people, the immune system prevents viral shedding and gets rid of B cells that express all the EBV latency associated genes But EBV lasts throughout life in a small # of resting B cells, that only express EBNA1 and LMP2 These cells can occasionally reactivate expression the other latency genes, causing them to proliferate In people with acquired problems in cell immunity, this proliferation can progress to EBV associated B cell lymphomas EBV can also contribute to development of Burkitt lymphoma Morphology of EBV: o The main changes involve the blood, lymph nodes, spleen, liver, and CNS o Peripheral blood shows lymphocytosis with a high lymphocyte% of WBCs Many of these lymphocytes are atypical lymphocytes, characterized by lots of cytoplasm that has many clear vacuolations, and oval,indented, or folded nucleus, and scattered granules Most of the atypical lymphocytes express CD8 o The lymph nodes are enlarged throughout the body B cell areas (follicles) may be hyperplastic o - - The spleen is enlarged, with expanded white and red pulp from all the many T cells These spleens are vulnerable to rupture Infectious mono classically presents with fever, sore throat, lymphadenitis, and sometimes malaise, fatigue, and lymphadenopathy, hepatitis, or a febrile rash You diagnose mono by these things: o Lymphocytosis with characteristic atypical lymphocytes in the peripheral blood o A positive heterophile antibody rxn – aka a positive monospot test o Specific antibodies for EBV antigens – viral capsid antigens, early antigens, or EB nuclear antigen In most patients, infectious mono resolves within 4-6 weeks o A common complication of mono is liver problems with jaundice, increased liver enzymes, poor appetite, and sometimes liver failure o The spleen is vulnerable to rupture (NO SPORTS!), and minor trauma to it can cause fatal hemorrhage o B cell lymphomas can show up in immunocompromised people