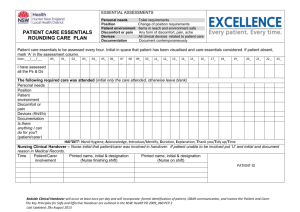
Australian Commission on Safety and Quality in Health Care
advertisement

Standard 6: Clinical Handover Suellen Allen, Accrediting Agencies Surveyor Workshop, 11 July 2012 What is Clinical handover Clinical Handover is the transfer of professional responsibility and accountability for some or all aspects of care for a patient or group of patients, to another person or professional group on a temporary or permanent basis Why have a Standard about clinical handover? Communication problems are a major contributing factor in adverse events particular during patient transitions of care Poor or absent clinical handover can have serious consequences: • delay in diagnosis or treatment • tests being missed or duplicated and • lead to the wrong treatment or • medication errors Clinical handover is often variable and ad hoc Information transferred between providers should include relevant data, be accurate, unambiguous and occur in a timely manor Structuring handover processes should be standardised to fit the local context Evidence base for Standard 6 Research from the National Clinical Handover Initiative Pilot Project Resources were developed from research to support clinical handover improvement and the Standard. The OSSIE Guide was endorsed by Australian Health Ministers as a national approach for the improving clinical handover There are principles of effective handover Evidence supports a structured format (minimum data set and structure for handover communication) and standardised processes for conducting clinical handover There is no one size fits all standard operating procedure – should be flexible standardisation to fit the local context, setting situation of handover Principles of effective handover Preparing for handover – setting, location and time Organising relevant workforce Being aware of clinical context and patient needs Participating in effective handover resulting in transfer of responsibility and accountability of care The Standard Intention of the Standard: Ensure there is timely, relevant and structured clinical handover that supports safe patient care. Clinical leaders and senior managers of a health service organisation implement documented systems for effective and structured clinical handover. Clinicians and other members of the workforce use the clinical handover systems. Three criteria 1. Governance and Leadership for effective clinical handover • Health service organisations implement effective clinical handover systems 2. Clinical Handover Process • Health service organisations have documented and structured handover processes in place 3. Patient and carer involvement in clinical handover • Health service organistions establish mechanisms to include patients and carers in clinical handover processes 1. Governance and leadership for effective clinical handover 6.1 Developing and implementing an organisational system for structured clinical handover that is relevant to the healthcare setting and specialities, including: • Documented policy, procedures and/or protocols • Agreed tools and guides Why? Policies, procedure and or protocols should include the documented structured processes that incorporates the principles of handover relevant to the setting and context to ensure: Workforce know the purpose of the handover Minimum data set and tools required to know and communicate Workforce know what documentation is required Workforce is trained and able to participate in agreed handover Handover is effective resulting the transfer responsibility and accountability Governance and leadership for effective clinical handover Issues What is ‘structured clinical handover’? that the minimum data set (information content) and conduct of handover be delivered in a structured format to improve patient safety What is a ‘minimum data set’ • the minimum content that must be contained and transferred in an individual patient handover • There are many possible minimum data sets and will vary depending on the context and reason of the handover Governance and leadership for effective clinical handover Issues: What structured clinical handover is relevant to the healthcare setting? Needs to be flexible – depend on: • Points of risk during patient transition of care • Setting • Situation • Method Clinical Handover will vary depending on: Size of the service, setting and circumstances, including: The situation of the handover: • during a shift change • when patients are transferred inter and intra hospital/service/unit • during patient admission, referral or discharge The method of the handover, such as: • face-to-face • via telephone • via written orders When aided by electronic handover tools The venue where handover takes place 1. Governance and leadership for effective clinical handover What? Establish and/or review policy, procedures and/or clinical handover protocols that are relevant to the healthcare setting e.g. different situations, methods and contexts Develop/ agree on structured clinical handover tools based on principles of clinical handover Train and monitor the workforce in the use of clinical handover policy/procedures Implement/maintain the structure clinical handover policy Develop a system to evaluation/ review clinical handover policies 2. Clinical Handover Process 6.2 Establishing and maintaining structured and documented processes for clinical handover Why? Standardisation and structuring of routine procedures allows clinical information to be conveyed more efficiently and with high reliability Clinical handover solutions must be standardised and fit for local purpose and appropriate to the clinical context in which handover occurs. 2. Clinical Handover Process 2. Clinical Handover Process - Issues Hospital example If a hospital transfers a patient: • • • • to another facility within the hospital to oncoming clinicians to the next shift or is discharged Handover processes need to be in place for these situations Shift to shift Inter and Intra hospital transfer Discharge Summary 2. Clinical Handover Process - Issues Day Procedure Centre example Patient handover situations may include: Handover between theatre staff with recovery staff Procedures for handover at discharge to the primary carer and the patient such as a discharge summary 2. Clinical Handover Process - Issues Issue participating in effective clinical handover Tools: Various tools (ISOBAR, ISBAR, SBAR, SHARED) have been developed to help structured handover and are designed to be flexible and adapted to suit local workforce environments. Health services can use new tools, or alter available tools, to develop structured process documentation. Education resources are available on the Commission Website Clinical Handover process What? Documented policy for clinical handover based on local needs including, time management strategies ensuring all relevant staff are present, organised, educated and prepared for handover Documented procedures for communication of transfer of responsibility and accountability Record of attendance for staff to appropriate training/orientation regarding standard of content and delivery of clinical handover for the local setting Clinical handover tools and policies for all levels of staff 2. Clinical Handover Process 6.3 Monitoring and evaluating the agreed structured clinical handover processes including: • Regularly reviewing local processes based on current best practice in collaboration with clinicians, patients and carers • Undertaking quality improvement activities and acting on issues identified from clinical handover reviews • Reporting on results of clinical handover reviews at executive level of governance Why? Evaluation establish if the policy, procedure and processes is efficient and determine if changes are needed to optimise performance and to identify areas for improvement. Reporting results should be fed back to the relevant committee or meeting about governance as health service organisation is responsible for ensuring that their systems for clinical handover are operational and effective. 2. Clinical Handover Process: 6.3 What? Identify a suitable individual, group or committee to take on responsibility for monitoring clinical handover process Audit of clinical handover/records to ensure staff practices are monitored and are consistent with policy, process and procedure Defined role and responsibility to facilitate clinical handover improvement (if required) and actions relating to evaluation and monitoring of current practice Defined process for feed back into executive level governance in relation to findings on evaluation and monitoring within the local setting Agree on strategies for evaluating the clinical handover processes that includes assessing processes and outcomes 2. Clinical Handover Process: 6.3 Issues Organisation-wide clinical handover evaluation systems may already be in place. However, localised workforce may find it beneficial to establish local project team or member of staff to oversee, plan and coordinate the implementation and evaluation of policy, procedure and process in their local setting. A localised mechanism to monitor the effectiveness of clinical handover policy is required to develop quality improvement processes tailored to individual workforce and environment which is consistent with best practice 2. Clinical Handover Process 6.4 Implementing a robust organisation-wide system of reporting, investigation and change management to respond to any clinical handover incidents Why? Monitoring adverse events from clinical handover allow practices to be modified to further suit local processes and patient outcomes Investigation and feedback to the workforce is important for them to understand the reason for practice change Evaluation allows measurement of the progress and impact of the handover process and possible improvement strategies 2. Clinical Handover Process: 6.4 What? Establish / confirm incident reporting system that captures data on clinical handover incidents Use information from the incident reports to improve performance Establishing a mechanism for review and feedback on clinical handover incidents and actions taken 3. Patient and carer involvement in clinical handover 6.5 Developing and implementing mechanisms to include patients and carers in the clinical handover process that are relevant to the healthcare setting Why? The effectiveness of handover communication may be enhanced by the participation of patients, carers and family members Patients involved in their own care, asking questions and being an active participant in decision making processes in relation to their condition, results in a reduction in the risk of the patient experiencing an adverse event 3. Patient and carer involvement in clinical handover : 6.5 What? Clinical handover procedure corresponds with the achievement of other expected outcomes in Standard 2 (Partnering with Consumers) Evidence of a patient experience survey examining exposure and feedback of clinical handover scenarios Evidence of an active mechanism for monitoring and responding to patient complaints and feedback relating to clinical Audit of clinical handover processes/documentation to establish the extent of patient and family involvement in handover discussions Evidence - 1 Policy and procedure Documentation of clinical handover Clinical handover records Patient care plans Discharge summaries Operation reports Transfer checklist (if appropriate) Evidence – 2 Workforce Education Orientation Policy / protocols Staff education sessions Feedback Evidence - 3 Clinical handover improvement/ Quality activities Improvement requires time Change management Clinician engagement Requires someone to be responsible for the improvement activity Other Issues ? Resources Safety and Quality Improvement Guide for Standard 6 Additional material about Standard 6 to follow from the Commission Implementation Toolkit for Clinical Handover Improvement and Resource Portal OSSIE Guide for Clinical Handover Improvement Jurisdictional programs Other Australian organisations and resources Summary www.safetyandquality.gov.au suellen.allen@safetyandquality.gov.au