presentation slides
advertisement
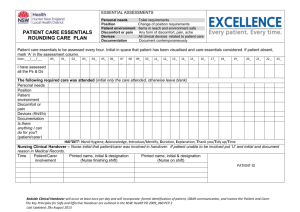
Patient Safety What should we be trying to communicate? Making Tomorrows Doctors Safer January 2011 Charles Vincent Professor of Clinical Safety Research Department of Surgical Oncology & Technology Imperial College London www.cpssq.org Overview Understanding patient safety What have we learned so far? Teams create safety So what should we try to communicate in education and training? Imperial Academic Health Sciences Centre Defining patient safety `The avoidance, prevention and amelioration of adverse outcomes or injuries stemming from the process of healthcare’ – Negative or positive – Reactive or proactive An Aspiration & Ambition – One of a number of objectives – The heart of quality Consequences of serious adverse events for patients & families Death of neonates, children, adults Loss of womb in young women Untreated cancer, mastectomy Blindness Disability and handicap, children and adults Chronic pain, scarring, incontinence Profound effects on all aspects of their lives Vincent, Young & Phillips, 1994 Impact of mistakes `I was really shaken. My whole feeling of self worth and ability was basically profoundly shaken’ `I was appalled and devastated that I had done this to somebody’ `My great fear was that I had missed something, then there was a sense of panic’ `It was hard to concentrate on anything else because I was so worried’ (Christensen, 1992) Patient Safety in the UK UK Department of Health, 2000 Epidemiology of harm Study Date of admissions Number of hospital admissions Adverse event rate (% admissions) California Insurance Study 1974 20864 4.65 * Harvard Medical Practice Study 1984 30195 3.7 Utah-Colorado 1992 14052 2.9 Australian 1992 14179 16.6 United Kingdom 1999 1014 10.8 Denmark 1998 1097 9.0 New Zealand 1998 6579 11.2 France ** 2002 778 14.5 Canada 2000 3745 7.5 The unreliability of healthcare Surgical Equipment Checks 120 % Checked 100 80 YES 60 NO 40 20 0 Surg Instruments op specific equip diathermy suction Undre et al, 2006 Understanding why things go wrong The safety paradox Healthcare staff are: – Highly trained & motivated – Committed to their patients – Use sophisticated technology Errors are common and patients are frequently harmed Understanding why things go wrong Chain of events Complexity and contributory factors The importance of cumulative minor errors and deviations Tackling safety on many levels Contributory factors: 7 levels of safety Patient Task Individual staff Team Working conditions Organisational Government and regulatory Vincent, Adams, Stanhope 1998 Teams create safety I Reliability of ward care (1) How well do you understand the goals of care for this patient today? (2) How well do you understand what work needs to be accomplished to get this patient to the next level of care? Less than 10% of nurses or doctors could answer these questions Pronovost et al, 2003 The Impact of Daily Goals Structured and organised care for each patient Reliability – reducing the gap between what should be happening and what is actually happening Reduced length of stay from 2.5 to 1.3 days Pronovost, 2003 II Patient handover Monitor Ventilator ODA Consultant Anaesthetist Power Anaesthetic Registrar Pump Drain s Pump CCC Reg / Nurse Nurse Nurse Urine Surgeon Multiple specialists Complex tasks Complex interfaces Time pressure Need for accuracy Catchpole et al, 2007 Process Organisation Pit Stop Task sequence A rhythm and order to events Task allocation Team members have defined tasks Leadership – Who is in charge Discipline and composure Explicit communication strategies to ensure calm and organised atmosphere Handover Stages in process clearly defined Ventilation: Anaesthetists Monitoring: ODA Drains: Nurses Anaesthetist has overall responsibility Defined moment for transfer to intensivist Comms limited during equipment phase Order for briefing (Anes; Surg; Discuss;Plan) No interruptions Catchpole et al, 2007 Performance improvements with new handover protocol Observation of 23 pre- and 27 post- handovers, balanced for operative risk 7 4 14 6 12 3 5 10 4 8 2 3 6 4 2 1 2 1 0 0 0 Before After Number of Errors Before After Information Omissions Before After Duration (mins) III Care bundles & organisational change Decreasing catheter related bloodstream infections Hand washing Full barrier precautions during the insertion of central venous catheters Cleaning the skin with chlorhexidine Avoiding the femoral site if possible Removing unnecessary catheters Median rate of infection per 1000 catheter days decreased from 2.7 at baseline to 0 at 3 months Mean rate at baseline decreased from 7.7 to 1.4 at 16-18 months follow up Care bundles & organisational change A focus on systems Local ownership and engagement Encouraging local adaptation of the intervention Creating a collaborative culture Time and resources Pronovost et al, 2008 So what should we try to communicate? Becoming aware Communication in Emergency Care – Tracking the process `I just could not believe we were doing all this’ – Observing the handover `Staggering, jaw dropping’ Putting on my `second hat’ (Krishna Moorthy) The essentials of patient safety The human tragedies Scale of error and harm The safety paradox Reflecting on one’s own environment The informal nature of many healthcare processes The many levels of influence and intervention The potential for simple changes That they can make a difference Safety in clinical practice I I do not undertake any procedure unless I am sure I am competent in performing it or have adequate supervision. Senior clinicians say they want juniors to err on the side of safety yet many younger clinicians fear seeming weak. I make a point to reminding myself day after day that I want to be safe first and brave afterwards. Spending longer with patients explaining and discussing the risks and benefits of treatment Being obsessive about hand washing. I am now very aware of why we are asked to do this and so less irritated about the time it takes Having enough humility to recognize when you are stepping beyond your depth and willingness to ask for help (Jacklin, Undre, Olsen) Safety in clinical practice II Being more vigilant in terms of errors that occur in day to day practice which I may have missed in the past. Being willing to address loose ends rather than say this is not part of my problem. Involving the patient in their care. For example always asking the patient which side they thought they were having the operation. Being more explicit about my instructions, discussing everything I think or intend to do to with the patient At handover always summarising the situation, outlining the plan and being absolutely clear about what to monitor and at what point I want to be called (Jacklin, Undre, Olsen) Further Information Clinical Safety Research Unit www.csru.org.uk Centre for Patient Safety & Service Quality www.cpssq.org