AP151 URINARY SLIDES-
advertisement

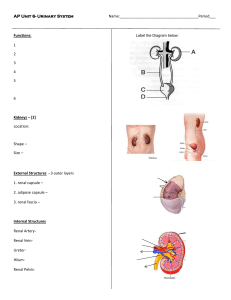
Fig. 17.1 Renal Function: • Remove organic wastes (urea, creatine, uric acid) • Control fluid volume/water balance – Influences blood pressure • Eliminate excess solutes from blood/control solute concentrations – Regulate solute concentration • Regulate pH Functions performed by nephrons (within kindeys) Renal corpuscle = glomerulus + glomerular capsule Renal tubule = PCT + nephron loop + DCT Fig. 17.5 RELAVENT SPACES/COMPARTMENT SUBSTANCE MOVE THROUGH BETWEEN TUBULE AND PLASMA Tubular fluid (originally filtrate) Peritubular fluid (interstitial fluid) Cytoplasm of plasma tubular cells Renal tubule in x.s. Peritubular capilary in x.s. Fig. 17.21 Renal Function is based on three process: 1. Filtration 2. Reabsorption 3. Secretion urine Conceptual Nephron Function/Urine formation Filtrate – Reabsorption + secretion = Urine Urine Production & Blood Volume • Urine is made from blood • Increased fluid retention = decreased urine output = decreased loss of blood volume (stabilization of blood volume) • Reduced fluid retention = increased urine output = increased loss of blood volume (reduced blood volume) Reabsorption Secretion Processes • Filtration: – The process in which substances from plasma leave blood and enter a nephron – From blood/plasma (of glomerulus) into glomerular capsule filtrate – Occurs in the corpuscle (glomerulus + bowmans capsule). Modification of Filtrate • Reabsorption: – Returns many substances that left glomerulus by filtration back into blood. – From renal tubule into interstitial space/blood then into plasma of peritubular capillaries – Occurs throughout the nephrons and collecting duct • Secretion – Eliminates additional substances from blood (of peritubular capillaries) by transporting them into renal tubule – From blood/plasma into renal tubule – In PCT, DCT, & collecting ducts Nephron Anatomy and Processes FILTRATION Filtration is the basis for all other renal events It occurs in the renal corpuscle FILTRATION: rate and composition We will examine two aspects of Filtration 1. How much filtration occurs is based on blood pressure • How much filtration occures = Glomerular Filtration Rate (GFR) 2. What enters filtrate (leaves blood) is based on size of substance Fig. 17.10 The amount of filtration that occurs = glomerular filtration rate (GFR) To function GFR must be: • 1. maintained within normal range despite changes in systemic BP • 2. Alterable to increase or decrease water loss through urine Filtrate Formation • Filtrate is formed when blood pressure in the glomerulus (glomerular hydrostatic pressure) causes substances to leave the glomerular capillaries and enter the nephron through the process of filtration. GFR is proportional to glomerular pressure: • Glomerular pressure ↑ GFR ↑ • Glomerular pressure ↓ GFR ↓ Filtrate Formation • The pressure in glomerular capillaries is unusually high (45-55 mmHg) because the efferent arteriole is narrower than the afferent arteriole. Glomerular pressure and therefore GFR is regulated by: 1. Dilation/constriction of afferent arteriole 2. Dilation/constriction of efferent arteriole GFR is regulated at 3 levels • Autoregulation – Maintains adequate GFR despite changes in blood flow to kidney – due to stretching of afferent arteriole – due to solute levels in filtrate • ANS – SD stimulation under periods of physical activity, stress, or in response to the baroreceptor reflex. • Hormonal regulation – Maintains adequate GFR despite changes in overall systemic BP – Renin (Renin-Angiotensin-Aldosterone-System) Autoregulation: Smooth muscle of the arterioles responds automatically to glomerular pressure (Myogenic control) • Increased blood pressure within afferent arterioles (which could lead to GFR being too high): – Stretching afferent arteriole Constriction of Aff Art decreased filtration pressure decreased GFR GFR stays within normal range • Decreased pressure within afferent arteriole causes (could lead to GFR being too low): – Less stretching of arteriolemuscle cells of Aff art relax aff art dilates increased filtration pressure increased GFRGFR stays within normal range Sympathetic Stimulation -- This tends to over-ride influence of other factors 1. Baroreceptor reflex (for BP regulation) – Decreasing BP causes ↑SD and constriction of afferent arteriole • • – Increasing BP causes ↓SD and dilation of afferent arteriole • • – Decreases GFR and filtrate/urine production Conserves fluid for blood helping maintain normal BP Increases GFR and filtrate production/urine output Eliminates excess fluid/blood volume helping reduce BP Strength of SD influence proportional to degree of BP change 2. Increases SD activity during prolonged exercise – shunts blood away from kidney to other organs needed to support other tissues (limited compensation for this by autoreg) – SD stimulation to shunt blood away from kidney and reduce water loss/urine output Fig. 17.11 Table 17.1 Hormonal Regulation • Renin—Angiotensin II – – – – – – In response to decreased GFR Juxtaglomerular apparatus (macula densa) releases renin Reninangiotensin II Angiotensin II vasoconstriction of efferent arteriole Increases glomerular pressure and GFR (also produces widespread systemic vasoconstriction to increase systemic BP) • Atrial Natriuretic Peptide (ANP) – – – – Increased BP stretch of atria walls Atria release ANP ANP dilation of afferent arteriole Dilation of afferent arteriole Increased GFR increasing urine production/water loss decreasing Blood volume BP goes down FILTRATION: What gets filtered (composition of filtrate) What enters filtrate (leaves blood) is based mostly on size of substance If substance is small enough to fit through gaps in glomerular capillaries and gaps between podocytes it will leave plasma, enter the corpuscle, and become filtrate • Plasma proteins (e.g., albumin), formed elements, and other proteins are too big to cross out of glomerulus • Water, ions, amino acids, glucose, urea, uric acid, creatine and other small organic molecules are small enough to leave glomerulus and become filtrate • When created the filtrate is isosmotic with interstitial fluid/peritubular fluid: – The solute concentration of filtrate and plasma is the same – See below and next slide Filtrate Modification • Reabsorption: – – – – Substances move from filtrate into interstitial space/blood. Occurs throughout the nephrons and collecting duct Primary location of reabsorption is the proximal tubule Re-captures substances that entered filtrate by that the body needs to retain/keep. – Based largely on passive diffusion and presence of various transport proteins • Transport proteins may be limited in reabsorptive capacity • Reabsorption can be selective in different regions based on which transport proteins are present – Reabsorption can be hormonally influenced/regulated Filtrate Modification • Secretion: – Moves substances from blood into filtrate – Eliminates/removes from blood substances that did not enter the filtrate or need to be eliminated at greater levels then achieved by filtration alone. – Typically based on transport proteins – Can be hormonally modified/regulated Tubular reabsorption: occurs throughout the tubule and collecting duct The PROXIMAL CONVOLUTED TUBULE: primary site of reabsorption • • Filtrate entering the PCT has a composition similar to plasma The PCT Will – – Reabsorbs 60-70% of filtrate (~108L of filtrate) Reabsorbs 99% of organic nutrients • E.g., Glucose, amino acids Reabsorption occurs through a complex combination of: • Active transport of ions creating gradients that power: – Passive movement through: • – – • Facilitate transport Cotransport Because the solute transport occurs through transport proteins each of which is specific to only one or several solutes: – – The reabsorption of specific solutes can be selectively regulated The transport proteins can potentially be saturated creating a maximum limit of how much of a solute can be reabsorbed • • Channels Tmax The reabsorption of water is always passive and secondary to the movement of a solute One set of reabsorption relationships is as follows: • Na+ is reabsorbed with pumps/active transport creating a electrical gradient • Cl- (an other anions) follows passively (attracted by + charges) • Water then follows solutes. 1. Na+ actively reabsorbed 2. Cl- passively reasbsorbed 3. H20 passively reabsorbed Creates concentration gradient Other routes of transport in PCT: • Glucose and amino acid reabsorption by co-transport with sodium • H+ secretion via counter transport • HCO3- reabsorbed with Na+ cotransport • Na+ reabsorption w/ K+ countertransport Secretion of various substances also occurs at the PCT but those will be considered later on a case-by-case basis Nephron loop (loop of henle) • The descending limb is permeable to water, but not to solutes • The ascending limb is relatively impermeable to water, but reabsorbs/pumps out Na+ and K+ • The Na+ and K+ pumped out of descending limb creates a high solute concentration in surrounding interstitial fluid/peritubular fluid that causes water to passively be reabsorbed from the descending limb. • This all results in a tubular fluid that is more concentrated with solutes by the time it reaches the end of the ascending limb. Distal Convoluted Tubule • Receives only 15-20% of original fluid of filtration • Variable reabsorption under the direction of hormones • Variable secretion of ions and xenobiotics (foreign molecules) Distal Convoluted Tubule: Reabsorption • Reabsorption in the DCT is mostly Na+ and Ca+ under hormonal control – Aldosterone causes increased production of incorporation of Na+ reabsorption proteins • Because Na is counter-transported for K, prolonged high aldosterone levels can lead to hypokalemia—dangerous – Ca+ reabsorption can be influenced by parathyroid hormone and calcitriol DCT: Secretion • When the concentration of some substances becomes high in blood, they diffuse into peritubular fluid where they will be picked up by tubular cells and transported into the renal tubule • Key substances Secreted include: – K+ • High blood K causes K+ secretion in exchange for Na+ (it is gradient driven) • By Na/K co-exchange – H+ • When blood becomes acidic peritubular cells secrete H+ into tubular fluid • The resulting HCO3- is transported into the peritubular fluid and then enters blood where it buffers pH • One H+ secretion pathway is Na+ reabsorption/aldosterone linked • So prolonged increased aldosterone can cause alkalosis Figure 26.15 The Effects of ADH on the DCT and Collecting Ducts Figure 26.15 Collecting Duct & DCT • Variable amounts of secretion • Variable amounts of reabsorption • We will focus on role of CD in water reabsorption and control of urine volume Regulation of Urine Volume: regulated through Na reabsorption and water permeability • Urine originates with the filtrate • If it is in urine, then it originally came from blood – Normal urine output ~1.2L/day • Increase urine output – Increased water to solute ratio – Increased water loss from body (potential blood volume decrease) • Decreased urine output – Decreased water to solute ration – Decreased water loss from body (stabilizes blood volume) A Summary of Renal Function Figure 26.16a Figure 26.11b Urine Volume is Regulated primarily by ADH (in conjunction with aldosterone) • ADH causes increased water permeability of DCT and CD – Causes incorporation of aquaporins • Increased ADH Results in – increased water reabsorption – Concentrates urine – Less water lost from plasma • Aldosterone enhances this by increasing the solute concentration of the peritubular fluid through increased Na reabsorption. The Effects of ADH on the DCT and Collecting Ducts dots represent solutes Figure 26.15a, b Fig. 17.20 ADH and water reabsorption NOTE: increased plasma osmolality can also be cause by increased solutes (Na+) in blood) Solute concentration Solute concentration ADH (vasopressin) • ADH released by Post Pit when osmoreceptors in hypothalamus detect high osmolality – From excess salt intake or dehydration – Causes thirst – Stimulates H2O reabsorption from urine • Homeostasis maintained by these countermeasures 14-25 Table 17.3 ACID BASE REGULATION • Homeostasis = H+ production/intake = H+ loss • When H+ formation > H+ loss = fluids more acidic • When H+ formation < H+ loss = fluids more alkaline or when base increases Normal blood pH range, acidosis, and alkalosis Fig. 18.06 Sources of H+ in body CO2 * * Volatile acid Metabolic* and fixed acids Buffers temporarily minimize pH changes (“neutralize” H+) This minimizes pH changes and damages to local tissues They do NOT eliminate H+ Lungs and Kidneys REMOVE H+ from body Also present in ICF but most important in ECF Bi-carbonate Buffer System: • From organic and fixed acids • NOT from CO2 production of aerobic respiration • in this process H+ are “fixed” as part of H20 and bicarbonate is reformed with the elimination of CO2 from body Eliminated through ventilation/exhalation “regenerates” HCO3- which accepts/buffer more H+ Acid base balance can maintained by: First: existing buffer systems • These work instantaneously • Limited (when all buffers are bound this system stops working) Second: physiological activity of: 1) respiratory system (responds in minutes, begins compensating within minutes) 2) renal systems (responds in hours to days)which can compensate through: • Secretion or absorption H+ • Secretion or absorption of acids and bases • Generation of additional buffers Accomplished by respiratory and renal compensations GENERAL BASIS FOR ACIDOSIS AND ALKALOSIS Types of pH imbalances • Respiratory acidosis: resp system failure to eliminate sufficient CO2 ( hypercapnia low pH) – Most common • Respiratory alkalosis – Too much CO2 eliminated (through hyperventilation) – hypocapnia high pH – Generally uncommon, but happens routinely at high altitude • Metabolic Acidosis – Commonly due to increase lactic acid and ketone bodies – Inability to secrete H+ at kidneys & severe bicarbonate loss – Second most common • Metabolic alkalosis – – – – Relatively uncommon Elevated levels of HCO3 Combined metabolic and respiratory acidosis Caused because oxygen started tissues perform anaerobic respiration Fig. 18.11 Mechanisms of Respiratory Acidosis Failure of receptors Fig. 18.13 Mechanisms of Respiratory alkalosis Fig. 18.12 Mechanisms of Metabolic Acidosis Fig. 18.14 Mechanisms of metabolic alkalosis Renal and Respiratory Compensation: responses to acidosis or alkalosis • Respiratory System: – Alter breathing rate to: • Remove H+ by “tying them up” in H2O • Producing HCO3- • Renal/Urinary System – Secrete H+ into urine – Reabsorb HCO3- Respiratory Influences/Compensations • Breathing/ventilating – Eliminates H+ and maintains available HCO3 • Increased breathing rate/ventilation more bicarbonate and less H+ decreased acidity (i.e., more alkaline) • Decreased breathing rate/ventilation less bicarbonate and more H+ increased acidity • Takes minutes to compensate for significant changes in plasma pH • Normal respiration is regulated by in pH of blood Increased respirations Decreased respirations Renal Influences/Compensation • Kidneys normally: – Secrete H+ or add H+ to blood • Ability to do so is limited by buffers in filtrate which help maintain H+ gradient – Reabsorb HCO3 (enters blood as NaHCO3) • These activities are dependent on carbonic anhydrase • Take days (1-3 d) compensate for significant changes in plasma pH • In response to alkalosis H+ is released into blood • Secretion of H+ into tubular fluid paired with release of HCO3- into blood • In starvation state, glutamine is metabolized causing release of HCO3- into blood GENERAL COMBINED RESPONSES TO ACIDOSIS H+ from body fluids/plasma causing acidosis GENERAL COMBINED RESPONSES TO ALKALOSIS H+ enters body fluid/plasma