Chapter 24: The Urinary System
advertisement
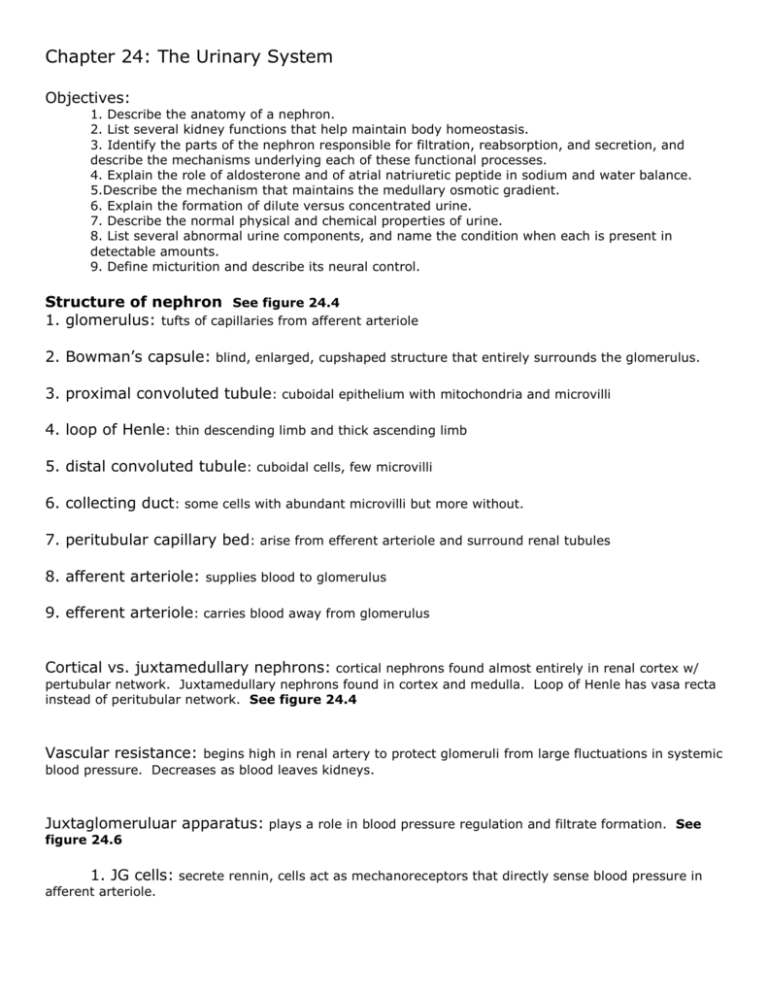
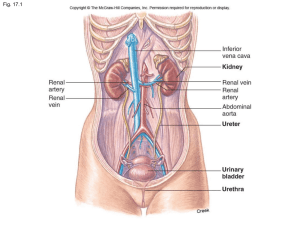
Chapter 24: The Urinary System Objectives: 1. Describe the anatomy of a nephron. 2. List several kidney functions that help maintain body homeostasis. 3. Identify the parts of the nephron responsible for filtration, reabsorption, and secretion, and describe the mechanisms underlying each of these functional processes. 4. Explain the role of aldosterone and of atrial natriuretic peptide in sodium and water balance. 5.Describe the mechanism that maintains the medullary osmotic gradient. 6. Explain the formation of dilute versus concentrated urine. 7. Describe the normal physical and chemical properties of urine. 8. List several abnormal urine components, and name the condition when each is present in detectable amounts. 9. Define micturition and describe its neural control. Structure of nephron See figure 24.4 1. glomerulus: tufts of capillaries from afferent arteriole 2. Bowman’s capsule: blind, enlarged, cupshaped structure that entirely surrounds the glomerulus. 3. proximal convoluted tubule: cuboidal epithelium with mitochondria and microvilli 4. loop of Henle: thin descending limb and thick ascending limb 5. distal convoluted tubule: cuboidal cells, few microvilli 6. collecting duct: some cells with abundant microvilli but more without. 7. peritubular capillary bed: arise from efferent arteriole and surround renal tubules 8. afferent arteriole: supplies blood to glomerulus 9. efferent arteriole: carries blood away from glomerulus Cortical vs. juxtamedullary nephrons: cortical nephrons found almost entirely in renal cortex w/ pertubular network. Juxtamedullary nephrons found in cortex and medulla. Loop of Henle has vasa recta instead of peritubular network. See figure 24.4 Vascular resistance: begins high in renal artery to protect glomeruli from large fluctuations in systemic blood pressure. Decreases as blood leaves kidneys. Juxtaglomeruluar apparatus: plays a role in blood pressure regulation and filtrate formation. See figure 24.6 1. JG cells: secrete rennin, cells act as mechanoreceptors that directly sense blood pressure in afferent arteriole. 2. Macula densa: (in DCT) near JG cells are chemoreceptors that respond to changes in solute content of filtrate. Filtration membrane: between blood and Bowman’s capsule. It is porous to allow free passage of water and solutes smaller than plasma proteins. It is similar to the respiratory membrane in thickness and function. See figure 24.7 Urine formation: 1000-1200 ml of blood passes through glomeruli/minute. 120-125 ml is forced out into tubules. The filtrate in the tubules is everything in plasma except proteins and cells. Urine, on the other hand, is metabolic wastes and unneeded substances. Of the 180 L of plasma processed everyday, only 1.5 L leaves the body as urine. Three processes are involved in urine formation: a) glomerular filtration b) tubular reabsorption c) secretion. See figure 24.8 Glomerular filtration: passive, nonselective process; uses hydrostatic pressure. By keeping proteins in plasma of capillaries, colloid osmotic pressure of glomerular blood is maintained. This ensures that all of the water in the plasma is not lost to the tubules. See figure 24.9 Presence of protein or blood in urine usually indicates some problem with filtration membrane. NFP: responsible for filtrate formation (net filtration pressure). NFP is about 10 mmHg. HPg: pushes water and solutes across membrane into capsule. OPg: pulls water back into glomerulus. HPc : pushes water back into glomerulus from capsule. Factors affecting glomerular filtration rate: GFR = 120-125 ml/min, 7.5 L/hr, 180 L/day 1. Total surface area available 2. Filtration membrane permeability 3. Net filtration pressure: a 15% drop in filtration pressure stops filtration altogether (due to change in glomerular blood pressure). BP, GFR; dehydration GFR Regulation of glomerular filtration: reabsorption depends on fate of glomerular filtration. If filtration is too fast and too much filtrate is lost to urine. Too slow and wastes are reabsorbed. See figure 24.10 1. Intrinsic control: within the kidney itself, the diameters of mainly the afferent, but also the efferent, arterioles are regulated. a. myogenic mechanism: this is the afferent arteriole smooth muscle response. Increasing systemic blood pressure causes the afferent arterioles to constrict. This restricts blood flow and lowers glomerular blood pressure (prevents it from rising to damaging levels). A decline in systemic blood pressure causes dilation of afferent arterioles and raises HP g. Both help maintain normal GFR. b. tubuloglomerular feedback: The macula densa exposed to slow flowing filtrate will cause vasodilation of afferent arteriole to raise GFR and speed up flow. When filtrate is moving rapidly or has a high Na/Cl content, the macula densa will make the JG cells produce a vasoconstrictor. This slows GFR so that the filtrate will have a longer time to be processed (reabsorbed). It also triggers the reninangiotensin mechanism. 2. Sympathetic control: When no sympathetic stimulation is occurring, renal vessels are maximally dilated and the kidney takes care of itself through intrinsic control. During times of stress, blood is shunted away from the kidneys and filtration is inhibited. 3. Renin-Angiotensin mechanism: triggered by the JG cells during low BP in renal blood vessels and therefore, low GFR. Renin from JG cells causes production of angiotensin II, a potent vasoconstrictor that causes MAP to rise. Also stimulates release of aldosterone that causes renal tubules to reclaim sodium from filtrate. Because water follows Na+, blood volume and blood pressure rise. Angiotensin causes the efferent arteriole to constrict more so that HP g rises (more blood stays in the glomerulus) and these all restore GFR to normal levels. Angiotensin II also stimulates hypothalamus to release ADH and make us thirsty. Tubular reabsorption (proximal convoluted tubule): passive and active transport occur here. Since our total blood volume is filtered into the tubules every 45 minutes, if our plasma wasn’t reabsorbed, it would drain away as urine. See figure 24.11, 24.12, Table 24.1 1. sodium reabsorption: active transport. Na/K pump puts it into interstitial space and then diffuses into peritubular capillaries. Also causes water to move into capillaries. 2. all nutrients: secondary active transport, carried into capillaries by cotransport using same carriers as Na+ 3. cations: active, cotransport with sodium 4. anions: passive transport 5. water: osmosis, driven by sodium reabsorption 6. urea and lipid soluble: passive diffusion 7. small proteins: endocytosis, then digested into amino acids for absorption Loop of Henle 1. Water is reabsorbed in the descending limb by osmosis 2. Na+, Cl-, K+; active transport in ascending limb 3. Ca2+, Mg2+; passive transport in ascending limb Distal convoluted tubule: most reabsorption from this point on depends on needs of the body and is regulated by hormones. ADH = water, aldosterone = sodium Tubular secretion: occurs in the distal convoluted tubule. H+, K+, creatinine, NH4+, organic acids, drugs, urea, and uric acid move from peritubular capillaries into the tubule. This is to dispose of substances not already in the filtrate, eliminate undesirable substances that were reabsorbed, to rid the body of excess K+, and control blood pH. Regulation of urine concentration and volume: Kidneys must keep solute load of body fluids constant (300 mOsm). Concentration of solute or # of solute particles in 1L of H 2O is osmolality. This is the body’s ability to cause osmosis. By regulating urine concentration and volume, the body fluids and plasma remain fairly uniform. Countercurrent mechanism: To excrete excess water (produce a dilute urine) it is necessary to dilute the filtrate as it passes through the tubule. This is achieved by reabsorbing a higher proportion of solutes than H2O. Normally, this would not occur because the filtrate has the same concentration of blood after 65% of filtrate is reabsorbed. So how does the concentration of filtrate go from 300 mOsm to 100 mOsm? This is the function of the Loop of Henle. See figure 24.14 Countercurrent multiplier 1. Descending limb of loop of Henle: impermeable to solutes and freely permeable to water and so filtrate become more concentrated as it reaches the bend in the Loop. 2. Ascending limb of loop of Henle: impermeable to water and actively transports NaCl into surrounding interstitial fluid. This dilutes the filtrate until it becomes very dilute (more than plasma or interstitial fluid) in the DCT. 3. Collecting ducts: permeable to urea to maintain high solute concentration in medullary interstitial fluid (1200 mOsm) 4. Vasa recta: Prevents too much reabsorption of salt and water that would decrease the nephron’s ability to dilute the urine. See figure 24.14 Formation of concentrated urine: in the presence of ADH, pores of the collecting duct and distal convoluted tubule enlarge and the filtrate loses water by osmosis as the duct passes through the medulla of the kidney. See figure 24.15, 24.16 Diuretics: chemical that enhance urinary output. Glucose (as in diabetes mellitus), alcohol (by inhibiting ADH), caffeine (inhibits sodium reabsorption). Composition of urine: See Table 24.2 urochrome, a yellow pigment from destruction of hemoglobin pH 6 nitrogenous wastes: urea and uric acid Na+ K+ Materials from tubular secretion