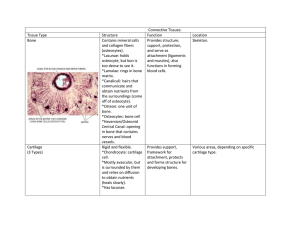
Cartilage
advertisement

Session3 Dr. Maria Zahiri Lecture outline Overview ( special connective tissue) Cartilage: morphology Type Histogenesis Bone: morphology Type Histogenesis Cartilage Cartilage: is a flexible connective tissue in animals, including the joints between bones, the rib cage, the ear, the nose, the bronchial tubes and the intervertebral discs. It is not as hard and rigid as bone, but it is stiffer and less flexible than muscle. Important for: - support to softer tissues - formation and growth of long bones Because of its rigidity, cartilage often serves the purpose of holding tubes open in an animal's body. Example: rings of the trachea, such as the cricoid cartilage and carina cartilage Consists of: Cells ECM - collagen and/or elastin fibers - proteoglycans - water CELLS: CHONDROBLAST Progenitor of chondrocytes Lines border between perichondrium and matrix Secretes type II collagen and other ECM components Chondrocytes Chondrocytes are chondroblasts which are surrounded by matrix and are quiescent They produce and maintain the cartilaginous matrix, which consists mainly of collagen and proteoglycans. Mature cartilage cell Reside in a space called the lacuna ECM: Collagen provides tensile strength and durability For example, if you inject papain (an enzyme that digests the protein cores of proteoglycans) into the ears of a rabbit, after a few hours the ears will loose their stiffness and droop. The combined properties of collagens and aggrecan in articular cartilage MORE FEATURES OF CARTILAGE Cartilage is an avascular tissue and relies on diffusion of nutrients and waste through the matrix The vasculature located in adjacent perichondrium and in absence of perichondrium, synovial fluid nurishes the cartilage Cartilage has no innervation, and no lymphatic vessels Chondrocytes have low metabolic activity Perichondrium o Perichondrium is a vascular sheath of dense irregular connective tissue surrounding cartilage (type I collagen) perichondrium perichondrium has 2 layer: • inner cellular layer • outer fibrous layer The cellular layer of the perichondrium contains chondrogenic cells that undergo division and differentiate into chondroblasts In embryo it serves as skeleton until replacement by bones, and form template for many bones It is also exist in epiphyseal plate, nose, bronchi, ends of ribs adjacent to sternum MORE FEATURES OF HYALLIN CARTILAGE Cells: Outer chondrocytes are elliptical with long axis parallel to surface Deeper ones are round, may be in groups of up to 8 - isogenous group Isogenous groups of chondrocytes: are the result of mitotic divisions of the cells during interstitial growth, several chondrocytes occupy a single lacuna. In epiphyseal plate chondrocytes located in rows They are often shrunken in histological sections Amorphous ground substance Territorial matrix: adjacent to chondrocytes stains darker than non-territorial matrix, because matrix around lacuna is poor in collagen but rich in chondroitin sulfate Interterritorial matrix: which is the bulk of cartilage is richer in type II collage Pericellular capsule: just around the lacuna is made of fine meshwork of collagen fibers and basal lamina like substances which protects the chondrocytes from mechanical stress Matrix of Hyaline Cartilage o Fiber: collagen type II , IX, X, and XI o Proteoglycan: Aggrecan o GAGs of Aggrecan is chondroitin 4-sulfate, chondroitin 6-sulfate, and heparan sulfate o Glycoprotein: Chondronectin o water Cartilage Growth o Interstitial growth: Existing chondrocytes mitotic division Isogenous groups (enlarging cartilage from within) o Appositional growth: o Chondrogenic cells (from inner layer of perichondrium) differentiation new chondroblasts (That adding matrix to periphery of cartilage) MORE FEATURES OF ELASTIC CARTILAGE It is similar to hyaline cartilage, but with many branching elastic fibers Yellow in colour Chondrocytes are more abundant and larger but matrix is less than hyaline cartilage Perichondrium is also rich in elastic fibers Fibrocartilage Usually merges with adjacent dense connective tissue Chondrocytes in rows or groups with thick bundles of collagen between them matrix is scant (rich in chondroitin and dermatan sulfate), and exhibit bundles of type I collagen which stain acidophilic It has no perichondrium Intervertebral Disks It is located between vertebrae Each disk has two components; Nucleus pulposus and Annulus fibrosus) Nucleus pulposus: is a gel-like matrix rich in hyaluronic acid and cells Annulus fibrosus: is made of fibrocartilage in overlapping layers Herniation : results from rupture of annulus fibrosus and expulsion of nucleus pulposus which can compress spinal cord or nerves Bone Bone is a specialized connective tissue of: calcified bone matrix 3 cell types: Osteocytes that are located in lacunae Osteoblasts that make new matrix and maintain old matrix Osteoclasts are multinucleated giant cells that phagocytose bone matrix in remodeling bone Osteoblasts Synthesize and maintain matrix (collagen, proteoglycans, and glycoproteins) bone forming cells typically rounded or cuboidal in shape Osteoblasts are basophilic as a result of abundance of rough endoplasmic reticulum Become osteocyte when surrounded by matrix Osteoid is newly made uncalcified matrix that separates osteoblasts and osteocytes from the calcified matrix Osteocyte mature bone cells are connect to other osteocytes by long processes via gap junctions Narrow canaliculi house cytoplasmic processes of osteocytes Canaliculi also contain extracellular fluid that carrying nutrients and metabolites Osteocytes maintain bone matrix Osteocyte Osteoclasts Large, multinucleated, and motile cells responsible for resorbing bone Their precursor located in bone marrow in common with monocytes Acidophilic cytoplasm, many lysosomes, many mitochondria Secrete organic acids, collagenase and other proteases that break down the matrix Osteoclasts They occupy shallow depressions that is called resorption bay (Howship’s lacunae) ruffled membrane: The region of the osteoclastic cytoplasm adjacent to the bone matrix which is being resorbed This is an area of numerous microvilli closely applied to the bone that is being hydrolyzed by the enzymes secreted by the osteoclast CO2+H2O H2CO3 H⁺+ HCO3⁻ Bone Matrix Inorganic part calcium and phosphate (Hydroxy apatite crystals [Ca10(Po4)6(OH)2]) Organic part Fiber: type I collagen bundles Glycoproteins: (Osteonectin, osteopontin) Proteoglycans: keratan sulfate and chondroitin sulfate bind to hyaluronic acid and form aggrecan composites Bone sialoprotein is another matrix protein that has binding site for integrins of bone cells and matrix components Periosteum dense irregular connective tissue that covers outer surface of bone Sharpey’s fiber inserting periosteum to the bone Outer fibrous layer: contains collagen bundles and fibroblasts of periosteum, distribute blood vessels and nerves to bone Inner cellular layer: has osteoprogenitor cells and osteoblasts Osteoprogenitor cells can form new osteoblasts Endosteum lines all internal bone surfaces It is a specialised thin connective tissue composed a single layer of osteoblasts, osteoclasts, and osteoprogenitor cells Types of Bone There is two different kind of mature bone Compact bone (no cavities) Cancellous (spongy bone) Long bones have ends (epiphyses) of spongy bone covered by a thin layer of compact bone; shaft (diaphysis) is mostly compact bone with small amount of spongy bone around marrow cavity Short bones have core of spongy bone surrounded by compact bone Spongy bone Spongy bone is composed of branching bone trabeculae and spicules Spongy bone is lamellar but there is not any haversian system It is extended from inner circumferential system of compact bone into marrow cavity Lamellae are arranged in irregular manner Spaces between lamellae contain bone marrow bone marrow Red bone marrow: where active hemopoiesis is taking place contains stem cells Yellow bone marrow: is inactive in hemopoiesis but acts as a reserve tissue It contains many unilocular adipocytes روزتان پرازخیر