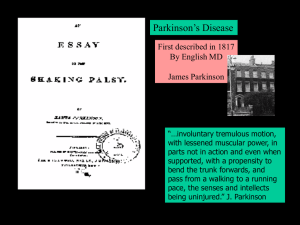
Parkinson's Disease
advertisement
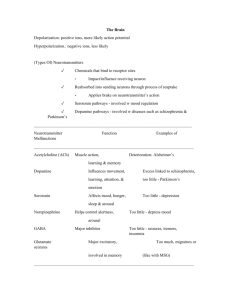
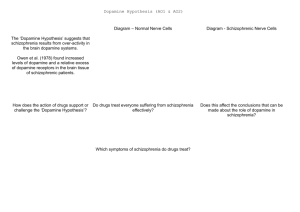
Proseminar in Biological Psychology Lecture 5 Too Much… Too little Dopamine PD & Schizophrenia Parkinson’s Disease First described in 1817 By English MD James Parkinson “…involuntary tremulous motion, with lessened muscular power, in parts not in action and even when supported, with a propensity to bend the trunk forwards, and pass from a walking to a running pace, the senses and intellects being uninjured.” J. Parkinson PD: Motor System Disorder • Chronic • Progressive • Non Fatal -1 to 1.5 million cases in the US strikes 1 in every 100 over 50 - Equal opportunity disease… men, women all ethnicities slightly higher rate among whites vs blacks Disease of Aging – onset 55 (idiopathic) Early Onset: 5-10% diagnosed Idiopathic 400,000 nigral cells in SN 2,400 cells die each year (Apoptosis)…80yrs X 2,400 = 200,000 …50% cell death = mild symptomology PD Pts = less than 100,000 cells So PD accelerated…why? • environmental? • genetic? • Head injury (parkinsonism) Monozygotic Dizygotic Parkinson's Disease •Lewy body in a substantia nigra neuron Caused by alpha synuclein & Parkin: gene responsible for making these proteins suspect early onset Environmental… Pesticides Herbicides Insecticides Well-Drinking Water Rural Living Higher incidence in agriculture workers…. Environmental… Metals: Manganese Copper Aluminum Pathology: Basal Ganglia Striatum Dopaminergic Cell bodies Nigrostriatal Pathway 80% die – degeneration of pathway..bingo NO Dopaminergic transmission Parkinson’s Disease Disease of the Basal Ganglia Globus Pallidus Substantia Nigra Caudate & Putamen Sub Thalamic Nuclei Excites the pathway Inhibits the pathway D2 D1 D2 receptors neurons from putamen fire excessively…loss of control of motor function Excitatory: green -- Inhibitory: red 1. Substantia Nigra axons inhibit the putamen 2. Axon loss increases excitation in Globus Pallidus 3. Globus Pallidus has increased inhibition to Thalamus 4. Then decreased excitation from the Thalamus to Cortex Symptoms 1. Rigidity •Muscular stiffness and increased muscle tone •Patients usually unaware of rigidity, troubled with slowness •More apparent to doctor than patient •Cogwheeling – ratchet like movement 2. Hypokinesia & 3. Bradykinesia •Hypokinesia: inability to initiate a voluntary movement •Bradykinesia: slowness of movement •Decrease in: Eyeblink Facial expression Eating and chewing 4.Tremor Involuntary movement: head, limbs, body • Most apparent when limb rested • Increases with stress • Ceases during sleep • Decreases with intentional movements •‘Pill rolling tremor' most prominent in fingers & hand •Most bothersome, yet least disabling of all symptoms Treatment... HEY LETS JUST GIVE DOPAMINE!!! Dopamine doesn’t cross the blood brain barrier…. But levodopa does (l-dopa)! Phenylalanine Problems: 1. doesn’t address the cell death 2. in time l-dopa is not effective (good for early to intermediate stages) Tyrosine L- Dopa Aromatic L amino acid decarboxylase •Sinemet: l-dopa+carbidopa (BBB) Dopamine l-dopa quickly converted to DA in PNS decarboxylase inhibitor • 75% respond to drug Selegiline (MAOI) •Delays Parkinsonian disability and the need for levodopa therapy by 9-12 months •Inhibits dopamine degradation •Allows for 20% smaller doses of levodopa •Exacerbation of levodopa-associated side effects •Insomnia, postural hypotension •inhibiting monoamine oxidase-B more pre-synaptic dopamine Also…inhibits this enzyme …converts MPTP to MPP+ (bad stuff) “on-off” of PD “I need to explain the "on-off" phenomenon. This Jekyll and-Hyde melodrama is a constant vexation for the P.D. patient, especially one as determined as I was to remain closeted. "On" refers to the time when the medication is telling my brain everything it wants to hear. I'm relatively loose and fluid, my mind clear and movements under control. Only a trained observer could detect my Parkinson's. During one of my "off" periods, even the most myopic layperson, while perhaps not able to diagnose P.D. specifically, can recognize that I am in serious trouble.” -Michael J. Fox, an excerpt from Lucky Man http://www.michaeljfox.org/ Thalamotomy: remove thalamus (M.J. Fox - 1998) Pallidotomy: remove the globus pallidus Helps the symptoms of tremor, dyskinesia, rigidity & bradykinesia -however, irreversible destruction of brain tissue -Overtime the benefits decline -May compromise other intact brain processes: speech, vision etc. New Treatment Strategy…..DBS (deep brain stimulation) - US Food and Drug Administration recently approved (Jan. 15, 2002) - Tiny electrodes on the scalp – connecting wire to implanted pulse generator under the collarbone - 80% reduction of tremor & bradyk. - can modify stimulation based on severity of symptoms DBS •Thalamus •Globus pallidus •Sub Thalamic (best) Thalamus: tremor, safer then lesion •Globus pallidus: dyskinesia safer than lesion •Sub Thalamic: improve all Symptoms improvement of motor scores 40-60% during “off” 10% during “on” Epidemiology • Prevalence ~1%; male = female Right now over 2 million adult Americans have schizophrenia • Seen in all cultures at similar frequency • Onset usually late adolescence to young adulthood, earlier in males than females (reactive: leaving home, loss of parent, 1st sex experience) • Increased chance of being born in the winter or early spring Schizophrenics have: • Increased mortality rate from accidents and natural causes: – life span is shortened by about a decade – some under-diagnosis of medical illness is present • ~10-15% suicide; ~50% attempt – – – – early in illness and young age high premorbid function depression the latter two often contributing to demoralization • Illness seems concentrated in urban settings, i.e., it is somewhat correlated with population density in larger cities • Illness seems concentrated in lower socioeconomic classes (1/3 of homeless) Subtypes – Catatonic • Catatonic behavior dominates (catalepsy-muscle rigidity/agitation) • Less common nowadays – Disorganized (hebephrenic) • Disorganized speech, behavior, and affect (flat or inappropriate) – Paranoid • Delusions and/or auditory hallucinations • Not limited to persecutory themes • Tends to have a later onset and better course Etiology of Schizophrenia Genetic Influences Adoption Studies - Genetic Implies genetic factors not environmental Genetics and Family Studies Etiology of Schizophrenia Brain Abnormalities Hippocampus Due to virus (Flu) 2nd trimester: adhesion molecules causing pathological migration Frontal Lobe Issues Functional brain imaging (PET, rCBF) • Failure to increase blood flow to the dorsolateral prefrontal cortex while performing the activation task of the Wisconsin Card Sorting Test • Reduced blood flow to the left globus pallidus (an even earlier finding in the course of illness) suggests a problem in the system connecting the basal ganglia to the frontal lobes • Correlation with severity of disease present Wisconsin Card Sorting Task • Subjects are asked to sort each upcoming card on to one of the four piles (they are not directed but may use shape, color or number). They are told correct/incorrect. Whichever category they choose is correct for a given number of categories then is met with an “incorrect” response. Subjects must “switch sets” to get a correct response. Failure to switch sets is termed “perseveration”. • Schizophrenic subjects perseverate relative to normal controls, Green et al, 1992 Ventricles Enlarged MRI – Discordant (bigger differences in males - ventricle size) Post-Mortem Neuroanatomy Disturbed connection between thalamus and PFC Serendipity Strikes Again!!!! 1960 – discovery that striatums (caudate putamens) depleted of Dopamine Dopamine Hypotheses of Schizophrenia • Dopamine – Schizophrenia due to over activity Dopamine Antagonist Clorpromazine (Carlsson, 1963) - expected DA levels to decrease -Metabolite increased -D2 receptor blockers work not because to much dopamine but Because to many receptors or too Sensitive… Dopamine Hypotheses of Schizophrenia (revised) • Dopamine – Positive symptoms of schizophrenia attributed to hyperdopaminergic function (more receptors or increased sensitivity, etc, D2) Evidence in Support and Against… Evidence in Support •Dopamine hypothesis - weaknesses: –Does not account for negative symptoms of schizophrenia Evidence against DA hypothesis of Schizophrenia – Glutamate??? • Disorganized thought symptoms of schizophrenia attributed to hypofunctional glutamate system • Glutamate antagonists such as PCP and ketamine mimic disorganized thought, may also cause psychosis and negative symptoms?