ppt
advertisement
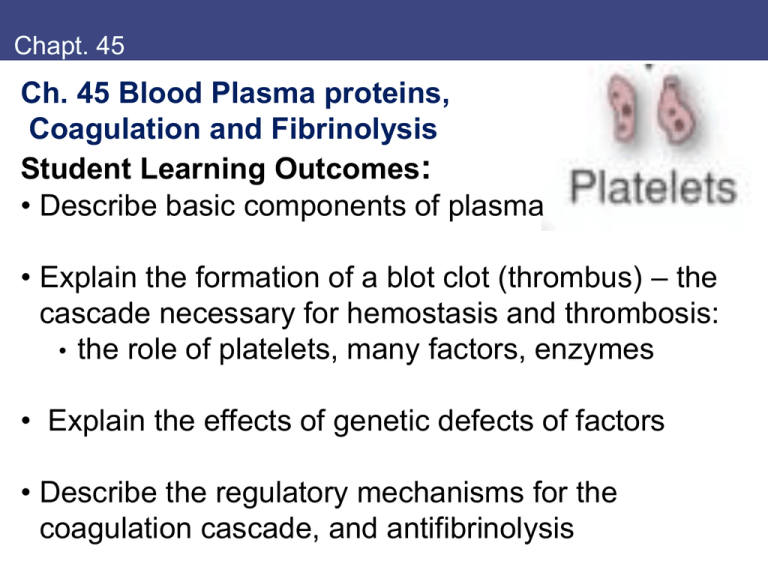
Chapt. 45 Ch. 45 Blood Plasma proteins, Coagulation and Fibrinolysis Student Learning Outcomes: • Describe basic components of plasma • Explain the formation of a blot clot (thrombus) – the cascade necessary for hemostasis and thrombosis: • the role of platelets, many factors, enzymes • Explain the effects of genetic defects of factors • Describe the regulatory mechanisms for the coagulation cascade, and antifibrinolysis Inheritance of X-linked gene for Factor VIII hemophilia A Pedigree of hemophilia transmission among Queen Victoria's descendants Hartl & Jones, Genetics Plasma components 1. Plasma proteins maintain proper distribution of water between blood and tissues • Plasma contains water, nutrients, metabolites, hormones, electrolytes, proteins • Same electrolyte composition as extracellular fluids • Many disease states alter plasma proteins – observe by electrophoresis • Osmotic pressure or plasma proteins is critical for bringing water back into blood from tissues Albumin and other proteins Albumin is major serum protein: • 69-kDa glycoprotein, 60% of total plasma protein • Carries free fatty acids, zinc, Ca2+, steroid hormones, many drugs Table 1 other serum proteins made in liver: Ceruloplasmin binds copper, storage Corticosteroid-binding globulin binds cortisol Haptoglobulin binds extracellular heme Lipoproteins bind cholesterol and fatty acids Retinol-binding protein binds vitamin A Sex hormone-binding globulin binds estradiol, testosterone Transferrin transports iron II. Other plasma proteins Immune response involves plasma proteins: • Immunoglobulins (antibodies) made by B lymphocytes – bind specific antigens • Complement proteins aid in clearance of Ag-Ab; also bind bacterial cell wall and lyse through C3b • Activation of complement is a proteolytic cascade Protease inhibitors in plasma control inflammatory response III. Plasma proteins maintain integrity of circulatory system Platelets are critical for clotting: If damage to endothelial lining of blood vessels exposes subendothelial layer: (Extracell matrix, smooth muscle cells) • Barrier (hemostatic plug, clot) forms • Platelets initiate, bind damage area • Clot formation is limited by regulation • Vessel heals, clot is degraded Platelets from megakaryocyte (~8 nuclei) → 4000 non-nucleated platelets Adhesion of platelets to subendothelium Platelets adhere to site of blood vessel injury: • Exposes collagen, vWF and other components (vWF (von Willebrand factor) is glycoprotein, is also in plasma, binds factor VIII to protect it; disorder → bleeding) • Then other GPs (glycoproteins) bind to fibrinogen, vWF • Platelet activation (release granules), brings more platelets (ADP is attractant); platelets release vasoconstrictors Fig. 1 Fibrinogen, fibrin Fibrinogen is cleaved to fibrin to form ‘soft clot’ • Fibrinogen in blood and in platelet granules • Assists platelet aggregation (of activated platelets) • Cleavage by thrombin protease releases fibrin monomers which aggregate • Thrombin also binds platelets through receptor, activates them Fig. 2 B. Blood coagulation cascade Thrombus (clot) is enhanced by thrombin activation • Proteins in plasma are proproteins (zymogens) • Activated by proteolytic cleavages, sequential • Highly regulated • Proenzymes: serine proteases: VII, XI, IX, X, prothrombin • Cofactor proteins bind: Tissue factor, V, VIII Fig. 3 PL, Ca are cofactors bound to phospholipids on platelet, vessel wall in Ca2+ complex Blood coagulation process Blood coagulation is complex cascade • Platelets adhere, plasma proteins react to subendothelium • Common path at Xa • Platelet membrane is scaffold for formation • g-carboxylated clotting proteins chelate to membrane surface (- PL, Ca2+) • Thrombin is critical: • Positive feedback • Accelerate process • Cleaves XIII → XIIIa Fig. 3 positive feedback by thrombin Table 45.2 Proteins of blood coagulation Factor descriptive name function/active form Coagulation factors I II III IV V VII VIII IX X XI XIII Fibrinogen Fibrin Prothrombin Serine protease Tissue factor Receptor, cofactor Ca2+ Cofactor Proaccelerin, labile factor Cofactor Proconvertin Serine protease Antihemophilia factor A Cofactor Antihemophilia factor B Serine protease Stuart-Prower factor Serine protease Plasma thromboplastin antecedent Serine protease Fibrin-stabilizing factor Ca2+-dep transglutaminase Regulatory factors Thrombomodulin endothelial cell receptor, binds thrombin Protein C activated by thrombomodulin-bound thrombin; serine protease Protein S cofactor; binds activated protein C Crosslink fibrin monomers 1. Fibrin molecules cross link to form hard clot: • • • • Thrombin forms Factor XIIIa Factor XIIIa catalyzes transamidation reaction (Gln-Lys) 3D mesh of fibrin fibers traps platelets, cells Factor XIIIa is only enzyme that is not a serine protease Fig. 4 g-carboxyglutamate in clotting factors Vitamin K is critical for clotting: • Coenzyme for g-carboxyglutamate • Modified residues on clotting proteases, done in liver • Proteases bind platelets through the Ca2+ and PLAssembly of factors, enzymes on complexes speeds up cascade Warfarin, rat poison, inhibits carboxylase, resembles VitK Fig. 5 Regulation of blood clotting Thrombin has prothrombotic role: (Fig. 3) • Feedback amplification • Stimulates its own formation by activating factors V, VII, XI • Activates platelet aggregation, release factor VIII from vWF, Thrombin has antithrombotic role: • Binds thrombomodulin, abolishes function of thrombin • protein C and cofactor protein S form activated protein C (APC) • Destroy factors Va, VIIIa Fig. 6 Serpins Serpins: Serine protease inhibitors: • • • • • Natural products ~10% of plasma proteins Each has reactive site like substrate, binds enzyme Antithrombin III (AT III) inactivates Thrombin Heparin (glycosaminoglycan) binds ATIII, allosteric enhance ATIII-heparin also inactivates XIIIa, Xa, IXa, Xa proteases ATT III + heparin Plasmin Plasmin degrades clot – highly regulated process: • • • • • Plasmin is serine protease, from plasminogen APC releases tPA from tissues (plasminogen activator) APC inactivates inhibitor of t-PA (PAI-I) Scu-PA is single-chain urokinase, can degrade fibrin Streptokinase binds plasminogen, allosteric modifier so that plasmin is formed • Circulating a-antiplasmin blocks soluble plasmin in blood T-PA and streptokinase treat Myocardial infarction Fig. 7 Key concepts Key concepts: • Plasma contains water, nutrients, hormones, electrolytes, proteins • Plasma proteins provide osmotic pressure for fluid balance • Plasma proteins and platelets maintain integrity of circulatory system • Clot formation is carefully regulated process to prevent overclotting (thrombosis) or underclotting (bleeding) • Hemophilia A is lack of Factor VIII • heparin, warfarin inhibit clotting; tPA dissolves Review question Review question: 3. A recent surgery patient receiving warfarin therapy was found to be bleeding internally. The clotting process is impaired in this patient because of which of the following? A. Inability of the liver to synthesize clotting factors B. Specific inhibition of factor XIII activation C. Inability to form clotting factor complexes on membranes. D. Reduction of plasma calcium levels E. Enhancement of protein C activity