Lymphatic system and Body Defenses
advertisement

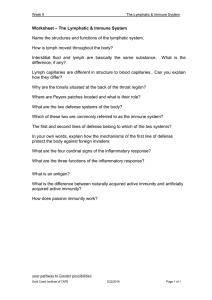
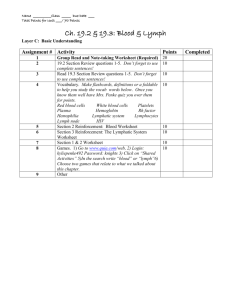
Lymphatic System and Immune System 2. Part 1 1. Function and Components of Lymphatic System Innate Defenses of Immune System Objectives 1. 2. 3. 4. 5. 6. Primary functions of lymphatic system Unique structure of lymphatic vessels and organs Connection of lymphatic and immune systems Two components of immune system Structures and cells of the innate division of immune system Steps of inflammatory response 2 semi-independent parts of Lymphatic System Lymphatic vessels • Meandering network of vessels and nodes • Transport back to blood any fluids that have escaped from the blood vascular system Lymphoid tissues, nodes and organs • Scattered throughout body • House phagocytic cells and lymphocytes… ready for body defense and resistance to disease Lymphatic Vessels 3 L per day of fluid seeps out of capillaries to become part of “interstitial fluid”…this would cause edema if not returned to blood vascular system Lymphatic vessels pick up this “lymph” Minivalve on lymph vessels Detours to lymph nodes to clean lymph of debris Returned to veins through large lymph ducts Lymph Leaked fluid from blood vessels that has become interstitial fluid and now must be returned to blood Contains plasma proteins Lymph means “clear water” About 3L per day Lymphatic Vessels One-way system, lymph flows toward the heart Lymph vessels (lymphatics) include: • Lymphatic capillaries • Lymphatic collecting vessels • Lymphatic trunks and ducts Venous system Arterial system Heart Lymphatic system: Lymph duct Lymph trunk Lymph node Lymphatic collecting vessels, with valves Blood capillaries Lymphatic capillary Tissue fluid Tissue cell Blood Lymphatic capillaries capillaries (a) Structural relationship between a capillary bed of the blood vascular system and lymphatic capillaries. Filaments anchored to connective tissue Endothelial cell Flaplike minivalve Fibroblast in loose connective tissue (b) Lymphatic capillaries are blind-ended tubes in which adjacent endothelial cells overlap each other, forming flaplike minivalves. Figure 19.1 Lymphatic Capillaries Similar to blood capillaries, except • Very permeable (take up cell debris, • pathogens, and cancer cells) Endothelial cells overlap to form one-way minivalves, and are anchored by collagen filaments, preventing collapse of capillaries Lymphatic Capillaries Absent from bones, teeth, bone marrow and the CNS Lacteals: specialized lymph capillaries present in intestinal mucosa • Absorb digested fat and deliver fatty lymph (chyle) to the blood Filaments anchored to connective tissue Endothelial cell Flaplike minivalve Fibroblast in loose connective tissue (b) Lymphatic capillaries are blind-ended tubes in which adjacent endothelial cells overlap each other, forming flaplike minivalves. Figure 19.1b Lymphatic Collecting Vessels Similar to veins, except Collecting vessels in the skin travel with superficial veins Deep vessels travel with arteries Nutrients are supplied from branching vasa vasorum • Have thinner walls, with more internal valves • Anastomose more frequently Lymphatic Trunks Formed by the union of the largest collecting ducts • Paired lumbar • Paired bronchomediastinal • Paired subclavian • Paired jugular trunks • A single intestinal trunk Lymphatic Ducts Lymph is delivered into one of two large ducts • Right lymphatic duct drains the right upper arm and • the right side of the head and thorax Thoracic duct arises from the cisterna chyli and drains the rest of the body Each empties lymph into venous circulation at the junction of the internal jugular and subclavian veins on its own side of the body Flow of Lymph Lymphatic Capillaries Lymphatic Collecting Vessels Lymphatic Trunks Lymphatic Ducts Terms to remember: Lacteals Right Lymphatic Duct/ Thoracic Duct Cisterna chyli Regional lymph nodes: Cervical nodes Internal jugular vein Entrance of right lymphatic duct into vein Entrance of thoracic duct into vein Axillary nodes Thoracic duct Cisterna chyli Lymphatic collecting vessels Aorta Inguinal nodes Drained by the right lymphatic duct Drained by the thoracic duct (a) General distribution of lymphatic collecting vessels and regional lymph nodes. Figure 19.2a Right jugular trunk Right lymphatic duct Right subclavian trunk Right subclavian vein Right bronchomediastinal trunk Brachiocephalic veins Superior vena cava Azygos vein Internal jugular veins Esophagus Trachea Left subclavian trunk Left jugular trunk Left subclavian vein Entrance of thoracic duct into vein Left bronchomediastinal trunk Ribs Thoracic duct Hemiazygos vein Cisterna chyli Right lumbar trunk Left lumbar trunk Inferior vena cava Intestinal trunk (b) Major lymphatic trunks and ducts in relation to veins and surrounding structures. Anterior view of thoracic and abdominal wall. Figure 19.2b Lymph Transport Lymph is propelled by • Contractions of smooth muscle in the walls of • • • • the lymphatic trunks Lymph vessels bundled together in connective tissue sheaths with blood vessels, so pulsations of nearby arteries propel lymph Milking action of active skeletal muscles so flows faster when active Pressure changes in thorax during breathing Valves prevent backflow Lymphoid Cells Lymphocytes the main warriors of the immune system Two main varieties T cells and B cells protect against antigens • T cells (T lymphocytes) • B cells (B lymphocytes) • Anything the body perceives as foreign • Bacteria and their toxins; viruses • Mismatched RBCs or cancer cells Lymphocytes T cells B cells • Manage the immune response • Attack and destroy foreign cells • Produce plasma cells, which secrete antibodies Other Lymphoid Cells Macrophages phagocytize foreign substances and help activate T cells Dendritic cells capture antigens and deliver them to lymph nodes Reticular cells produce stroma that supports other cells in lymphoid organs • Fibroblast-like cells Cell types Macrophage Extracellular matrix Ground substance Fibers • Collagen fiber • Elastic fiber • Reticular fiber Fibroblast Lymphocyte Fat cell Capillary Mast cell Neutrophil Figure 4.7 Macrophage Reticular cells on reticular fibers Lymphocytes Medullary sinus Reticular fiber Figure 19.3 Lymphoid Tissue Houses and provides a proliferation site for lymphocytes Furnishes a surveillance vantage point Two main types • Diffuse lymphatic tissue • Lymphatic follicles Lymphoid Tissue Diffuse lymphatic tissue comprises scattered reticular tissue elements in every body organ • Larger collections in the lamina propria of mucous membranes and lymphoid organs Lymphoid Tissue Lymphatic follicles (nodules) are solid, spherical bodies of tightly packed reticular elements and cells • Germinal center composed of dendritic and B • cells May form part of larger lymphoid organs Lymph Nodes Principal lymphoid organs of the body Embedded in connective tissue, in clusters along lymphatic vessels Near the body surface in inguinal, axillary, and cervical regions of the body Regional lymph nodes: Cervical nodes Internal jugular vein Entrance of right lymphatic duct into vein Entrance of thoracic duct into vein Axillary nodes Thoracic duct Cisterna chyli Lymphatic collecting vessels Aorta Inguinal nodes Drained by the right lymphatic duct Drained by the thoracic duct (a) General distribution of lymphatic collecting vessels and regional lymph nodes. Figure 19.2a Lymph Nodes Functions 1. Filter lymph—macrophages destroy 2. microorganisms and debris Immune system—lymphocytes are activated and mount an attack against antigens Structure of a Lymph Node Bean shaped External fibrous capsule Trabeculae extend inward and divide the node into compartments Two histologically distinct regions • Cortex • Medulla Structure of a Lymph Node Cortex contains follicles with germinal centers, heavy with dividing B cells Dendritic cells nearly encapsulate the follicles Deep cortex houses T cells in transit T cells circulate continuously among the blood, lymph nodes, and lymphatic stream Afferent lymphatic vessels Cortex • Lymphoid follicle • Germinal center • Subcapsular sinus Efferent lymphatic vessels Hilum Medulla: • Medullary cord • Medullary sinus Trabeculae Capsule (a) Longitudinal view of the internal structure of a lymph node and associated lymphatics Figure 19.4a Structure of a Lymph Node Medullary cords extend inward from the cortex and contain B cells, T cells, and plasma cells Lymph sinuses contain macrophages Follicles Trabecula Subcapsular sinus Capsule Medullary cords Medullary sinuses (b) Photomicrograph of part of a lymph node (72x) Figure 19.4b Circulation in the Lymph Nodes Lymph • Enters via afferent lymphatic vessels • Travels through large subcapsular sinus and • smaller sinuses Exits the node at the hilus via efferent vessels Fewer efferent vessels, causing flow of lymph to stagnate, allowing lymphocytes and macrophages time to carry out functions Cortex • Lymphoid follicle Afferent lymphatic vessels • Germinal center • Subcapsular sinus Efferent lymphatic Follicles vessels Trabecula Subcapsular sinus Hilum Medulla: Capsule • Medullary cord • Medullary sinus Medullary cords Trabeculae Capsule (a) Longitudinal view of the internal structure of a lymph node and associated lymphatics Medullary sinuses (b) Photomicrograph of part of a lymph node (72x) Figure 19.4 Homeostatic imbalance of Lymph Nodes Swollen Lymph Nodes • Trap large numbers of bacteria/ inflammed • Infected lymph nodes= buboes • Bubonic plague Cancer Sites • Secondary cancer sites as cancer cells • metastasize Cancer infiltrated lymph nodes are swollen but not painful Spleen Largest lymphoid organ Served by splenic artery and vein, which enter and exit at the hilus Functions • Site of lymphocyte proliferation and immune • surveillance and response Cleanses the blood of aged cells and platelets and debris Diaphragm Spleen Adrenal gland Left kidney Splenic artery Pancreas (c) Photograph of the spleen in its normal position in the abdominal cavity, anterior view. Figure 19.6c Spleen Stores breakdown products of RBCs (e.g., iron) for later reuse Stores blood platelets Site of fetal erythrocyte production (normally ceases after birth) Has a fibrous capsule and trabeculae Contains lymphocytes, macrophages, and huge numbers of erythrocytes Structure of the Spleen Two distinct areas • White pulp around central arteries • Mostly lymphocytes on reticular fibers and • involved in immune functions Red pulp in venous sinuses and splenic cords • Rich in macrophages for disposal of worn-out RBCs and bloodborne pathogens Capsule Trabecula Splenic cords Venous sinuses Arterioles and capillaries Splenic artery Splenic vein Hilum Red pulp White pulp Central artery (a) Diagram of the spleen, anterior view Splenic artery Splenic vein (b) Diagram of spleen histology Figure 19.6a,b Thymus Size with age • In infants, it is found in the inferior neck and • • extends into the mediastinum, where it partially overlies the heart Increases in size and is most active during childhood Stops growing during adolescence and then gradually atrophies Thymus Thymic lobes contain an outer cortex and inner medulla Cortex contains densely packed lymphocytes and scattered macrophages Medulla contains fewer lymphocytes and thymic (Hassall’s) corpuscles involved in regulatory T cell development Thymic (Hassall’s) corpuscle Medulla Cortex Figure 19.7 Thymus Differs from other lymphoid organs in important ways • It functions strictly in T lymphocyte maturation • It does not directly fight antigens The stroma of the thymus consists of starshaped epithelial cells (not reticular fibers) These thymocytes provide the environment in which T lymphocytes become immunocompetent Tonsils Simplest lymphoid organs Form a ring of lymphatic tissue around the pharynx • Palatine tonsils—at posterior end of the oral cavity • Lingual tonsils—grouped at the base of the tongue • Pharyngeal tonsil—in posterior wall of the nasopharynx • Tubal tonsils—surrounding the openings of the auditory tubes into the pharynx • Pharyngotympanic tube Tonsils Contain follicles with germinal centers Are not fully encapsulated Epithelial tissue overlying tonsil masses invaginates, forming tonsillar crypts Crypts trap and destroy bacteria and particulate matter Pharyngeal tonsil Palatine tonsil Lingual tonsil Tonsil Tonsillar crypt Germinal centers in lymphoid follicles Figure 19.8 Aggregates of Lymphoid Follicles Peyer’s patches • Clusters of lymphoid follicles • In the wall of the distal portion of the small • intestine Similar structures are also found in the appendix Peyer’s patches and the appendix • Destroy bacteria, preventing them from breaching • the intestinal wall Generate “memory” lymphocytes Lymphoid nodules (follicles) of Peyer’s patch Smooth muscle in the intestinal wall Figure 19.9 MALT: a Collection of Lymph tissues Mucosa-associated lymphatic tissue, including • Peyer’s patches, tonsils, and the appendix • (digestive tract) Lymphoid nodules in the walls of the bronchi (respiratory tract) Protects the digestive and respiratory systems from foreign matter Quick review of Lymphatics 1. 2. 3. 4. 5. Why do lymph nodes or tonsils swell? Which cells produce T cells?...antibodies? What is lymph node connection with cancer? What is lymph? How much transported? What lymph vessel empties into blood system? Where? Name the organ: 6. “youth organ” / doesn’t actively clean lymph 7. Destroys worn out RBC and returns to liver 8. Filters lymph/ has more afferent vessels than efferent 9. Stores platelets/ a blood reservoir 10. Simplest lymph organ/ helps immune cells create memory Immunity Resistance to disease Functional system rather than organ system Immune system has two intrinsic systems • Innate (nonspecific) defense system • Adaptive (specific) defense system Immunity 1. Innate defense system has two lines of defense • • First line of defense is external body membranes (skin and mucosae) Second line of defense is antimicrobial proteins, phagocytes, and other cells • • Inhibit spread of invaders Inflammation is its most important mechanism Immunity 2. Adaptive defense system • Third line of defense attacks particular foreign substances • Takes longer to react than the innate system Innate and adaptive defenses are deeply intertwined Surface barriers • Skin • Mucous membranes Innate defenses Internal defenses • Phagocytes • NK cells • Inflammation • Antimicrobial proteins • Fever Humoral immunity • B cells Adaptive defenses Cellular immunity • T cells Figure 20.1 Innate Defenses Surface barriers • Skin, mucous membranes, and their secretions • Physical barrier to most microorganisms • Keratin is resistant to weak acids and bases, bacterial enzymes, and toxins • Mucosae provide similar mechanical barriers Surface Barriers Protective chemicals inhibit or destroy microorganisms • Skin acidity – pH 3-5 • Lipids in sebum and dermcidin in sweat • HCl and protein-digesting enzymes of • • stomach mucosae Lysozyme of saliva and lacrimal fluid Mucus Surface Barriers Respiratory system modifications • Mucus-coated hairs in the nose • Cilia of upper respiratory tract sweep dustand bacteria-laden mucus from lower respiratory passages Internal Defenses: Cells and Chemicals Necessary if microorganisms invade deeper tissues • Phagocytes • Natural killer (NK) cells • Inflammatory response (macrophages, mast • • cells, WBCs, and inflammatory chemicals) Antimicrobial proteins (interferons and complement proteins) Fever Phagocytes: Macrophages Macrophages develop from monocytes to become the chief phagocytic cells • Free macrophages wander through tissue spaces • E.g., alveolar macrophages • Fixed macrophages are permanent residents of some organs • E.g., Kupffer cells (liver) and microglia (brain) Phagocytes: Neutrophils Neutrophils • Become phagocytic on encountering • infectious material in tissues Most abundant white blood cell Mechanism of Phagocytosis Step 1: Adherence of phagocyte to pathogen • Facilitated by opsonization—coating of pathogen by complement proteins or antibodies Innate defenses Internal defenses (a) A macrophage (purple) uses its cytoplasmic extensions to pull spherical bacteria (green) toward it. Scanning electron micrograph (1750x). Figure 20.2a 1 Phagocyte adheres to pathogens or debris. Lysosome Phagosome (phagocytic vesicle) Acid hydrolase enzymes (b) Events of phagocytosis. 2 Phagocyte forms pseudopods that eventually engulf the particles forming a phagosome. 3 Lysosome fuses with the phagocytic vesicle, forming a phagolysosome. 4 Lysosomal enzymes digest the particles, leaving a residual body. 5 Exocytosis of the vesicle removes indigestible and residual material. Figure 20.2b Mechanism of Phagocytosis Destruction of pathogens • Acidification and digestion by lysosomal • enzymes Respiratory burst • Release of cell-killing free radicals • Activation of additional enzymes • Oxidizing chemicals (e.g. H2O2) • Defensins (in neutrophils) Natural Killer (NK) Cells Large granular lymphocytes Target cells that lack “self” cell-surface receptors Induce apoptosis in cancer cells and virusinfected cells Secrete potent chemicals that enhance the inflammatory response Perforins/ granzymes Inflammatory Response Triggered whenever body tissues are injured or infected Prevents the spread of damaging agents Disposes of cell debris and pathogens Sets the stage for repair Inflammatory Response Cardinal signs of acute inflammation: 1. Redness 2. Heat 3. Swelling 4. Pain (And sometimes 5. Impairment of function) Inflammatory Response Macrophages and epithelial cells of boundary tissues bear Toll-like receptors (TLRs) TLRs recognize specific classes of infecting microbes Activated TLRs trigger the release of cytokines that promote inflammation and attract WBCs to area Inflammatory Response Inflammatory mediators • Histamine (from mast cells) • Blood proteins • Kinins, prostaglandins (PGs), leukotrienes, and complement •Released by injured tissue, phagocytes, lymphocytes, basophils, and mast cells Vasodilation and Increased Vascular Permeability Inflammatory chemicals cause • Dilation of arterioles, resulting in hyperemia • Increased permeability of local capillaries and edema (leakage of exudate) Exudate contains proteins, clotting factors, and antibodies Inflammatory Response: Edema Functions of the surge of exudate • Moves foreign material into lymphatic vessels • Delivers clotting proteins to form a scaffold for repair and to isolate the area Innate defenses Tissue injury Internal defenses Release of chemical mediators (histamine, complement, kinins, prostaglandins, etc.) Release of leukocytosisinducing factor Leukocytosis (increased numbers of white blood cells in bloodstream) Initial stimulus Vasodilation of arterioles Increased capillary permeability Local hyperemia (increased blood flow to area) Capillaries leak fluid (exudate formation) Attract neutrophils, monocytes, and lymphocytes to area (chemotaxis) Leukocytes migrate to injured area Margination (leukocytes cling to capillary walls) Physiological response Signs of inflammation Leaked protein-rich fluid in tissue spaces Result Heat Redness Locally increased temperature increases metabolic rate of cells Pain Swelling Possible temporary limitation of joint movement Leaked clotting proteins form interstitial clots that wall off area to prevent injury to surrounding tissue Temporary fibrin patch forms scaffolding for repair Diapedesis (leukocytes pass through capillary walls) Phagocytosis of pathogens and dead tissue cells (by neutrophils, short-term; by macrophages, long-term) Pus may form Area cleared of debris Healing Figure 20.3 Phagocyte Mobilization Neutrophils first, they become activated phagocytes Macrophages follow to inflamed sites Phagocyte Mobilization Steps for phagocyte mobilization 1. 2. 3. 4. Leukocytosis: release of neutrophils from bone marrow in response to leukocytosis-inducing factors from injured cells Margination: neutrophils cling to the walls of capillaries in the inflamed area Diapedesis of neutrophils Chemotaxis: inflammatory chemicals (chemotactic agent) promote positive chemotaxis of neutrophils Innate defenses Internal defenses Inflammatory chemicals diffusing from the inflamed site act as chemotactic agents. Leukocytosis. Neutrophils enter blood from bone marrow. 1 Margination. Neutrophils cling to capillary wall. 2 Chemotaxis. Neutrophils follow chemical trail. 4 Capillary wall Basement membrane Endothelium Diapedesis. Neutrophils flatten and squeeze out of capillaries. 3 Figure 20.4 Antimicrobial Proteins Interferons (IFNs) and complement proteins • Attack microorganisms directly • Hinder microorganisms’ ability to reproduce Interferons Viral-infected cells are activated to secrete IFNs IFNs enter neighboring cells Neighboring cells produce antiviral proteins that block viral reproduction Innate defenses Virus Viral nucleic acid 1 Virus enters cell. Internal defenses New viruses 5 Antiviral proteins block viral reproduction. 2 Interferon genes switch on. DNA Nucleus mRNA 4 Interferon 3 Cell produces interferon molecules. Interferon Host cell 2 Host cell 1 Binds interferon Infected by virus; from cell 1; interferon makes interferon; induces synthesis of is killed by virus protective proteins binding stimulates cell to turn on genes for antiviral proteins. Figure 20.5 Interferons Functions Genetically engineered IFNs for • Anti-viral • Reduce inflammation • Activate macrophages and mobilize NK cells • Antiviral agents against hepatitis and genital • warts virus Multiple sclerosis treatment Complement ~20 blood proteins that circulate in an inactive form Include C1–C9, factors B, D, and P, and regulatory proteins Major mechanism for destroying foreign substances Amplifies all aspects of the inflammatory response Kills bacteria and certain other cell types by cell lysis Enhances both nonspecific and specific defenses Complement Activation Two pathways 1. Classical pathway • • Antibodies bind to invading organisms C1 binds to the antigen-antibody complexes (complement fixation) 2. Alternative pathway • Triggered when activated C3, B, D, and P interact on the surface of microorganisms Complement Activation Activated complement • Enhances inflammation • Promotes phagocytosis • Causes cell lysis • C3b initiates formation of a membrane attack complex (MAC) • MAC causes cell lysis by inducing a massive influx of water • C3b also causes opsonization, and C3a causes inflammation Classical pathway Antigen-antibody complex + complex Opsonization: coats pathogen surfaces, which enhances phagocytosis Insertion of MAC and cell lysis (holes in target cell’s membrane) Alternative pathway Spontaneous activation + Stabilizing factors (B, D, and P) + No inhibitors on pathogen surface Enhances inflammation: stimulates histamine release, increases blood vessel permeability, attracts phagocytes by chemotaxis, etc. Pore Complement proteins (C5b–C9) Membrane of target cell Figure 20.6 Fever Systemic response to invading microorganisms Leukocytes and macrophages exposed to foreign substances secrete pyrogens Pyrogens reset the body’s thermostat upward Fever High fevers are dangerous because heat denatures enzymes Benefits of moderate fever • Causes the liver and spleen to sequester iron • and zinc (needed by microorganisms) Increases metabolic rate, which speeds up repair Adaptive Defenses The adaptive immune (specific defense) system • Protects against infectious agents and • • abnormal body cells Amplifies the inflammatory response Activates complement Adaptive Defenses • • • Adaptive immune response Is specific Is systemic Has memory Two separate overlapping arms 1. Humoral (antibody-mediated) immunity 2. Cellular (cell-mediated) immunity Antigens Substances that can mobilize the adaptive defenses and provoke an immune response Most are large, complex molecules not normally found in the body (nonself) Complete Antigens Important functional properties • Immunogenicity: ability to stimulate proliferation • of specific lymphocytes and antibodies Reactivity: ability to react with products of activated lymphocytes and antibodies released Examples: foreign protein, polysaccharides, lipids, and nucleic acids Haptens (Incomplete Antigens) Small molecules (peptides, nucleotides, and hormones) Not immunogenic by themselves Are immunogenic when attached to body proteins Cause the immune system to mount a harmful attack Examples: poison ivy, animal dander, detergents, and cosmetics Antigenic Determinants Certain parts of an entire antigen that are immunogenic Antibodies and lymphocyte receptors bind to them Most naturally occurring antigens have numerous antigenic determinants that • Mobilize several different lymphocyte populations • Form different kinds of antibodies against it Large, chemically simple molecules (e.g., plastics) have little or no immunogenicity Antibody A Antigenbinding sites Antigenic determinants Antigen Antibody B Antibody C Figure 20.7 Self-Antigens: MHC Proteins Protein molecules (self-antigens) on the surface of cells Antigenic to others in transfusions or grafts Example: MHC proteins • Coded for by genes of the major histocompatibility complex (MHC) and are unique to an individual MHC Proteins Classes of MHC proteins • Class I MHC proteins, found on virtually all body • cells Class II MHC proteins, found on certain cells in the immune response MHC proteins display peptides (usually selfantigens) In infected cells, MHC proteins display fragments of foreign antigens, which help mobilize Cells of the Adaptive Immune System Two types of lymphocytes • B lymphocytes (B cells)—humoral immunity • T lymphocytes (T cells)—cell-mediated immunity Antigen-presenting cells (APCs) • Do not respond to specific antigens • Play essential auxiliary roles in immunity