Hemotologic Disorders - Faculty Sites
advertisement

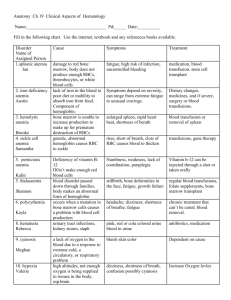
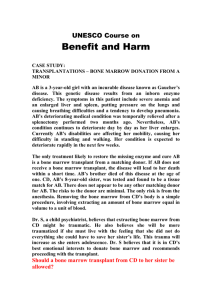
Hemotologic Disorders By Diana Blum RN MSN Metropolitan Community College NURS 2140 Should be subjective Should be objective Assessment Blood is a type of connective tissue Immunological aspects also important ◦ Transports nutrition ◦ Transports oxygen ◦ Transports hormones ◦ Critical to body defense ◦ ◦ ◦ ◦ Maintains temperature Controls PH Removes toxins Regulates electrolytes Anatomy Hematopoiesis: Bone Marrow: Stem Cell: Plasma: Leukocyte: Reticulocyte: WBC: RBC: Erythrocyte: Platelet: Cell Types (page 1991-94) Responsible for removing excess fluid protein and large particles from cells Main functions: ◦ fluid balance maintenance ◦ Defense ◦ Fat absorber Lymphatic system Stores 20-40 ml blood Removes old cells Filters and destroys antigens before they enter system Stores platelets (1/3 of body’s store) Spleen Stopping of blood flow 2 phases: ◦ Primary ◦ Secondary Hemostasis (page 1995) Be able to explain tests to pts Be able to explain why tests being done Know normal from abnormal Be good communicator with physician Be able to consider anticipated actions ◦ Ex. When blood transfusion needed Critical thinking here Hemoglobin is low Oxygen is low Not a disease but an underlying condition 2 types: hypoproliferative and hemolytic ◦ Hypoproliferative: marrow can’t produce adequate erythrocytes Lack of factors, chemicals, marrow damage ◦ Hemolytic: premature destruction of erythrocytes. Leads to tissue hypoxia Abnormality like sickle cell, direct injury Anemia (page 2008) Stimulation of RBCs by erythropoietin Erythropoietin: hormone produced by kidneys during periods of hypoxia to ensure growing tissues will have sufficient oxygen. Erythropoiesis Based on: ◦ Marrow ability to respond to decreased erythrocytes ◦ Manner of maturity for young erythrocytes ◦ The presence or absence of end products of erythrocyte destruction within the circulation Determination between types Rapidity with the anemia has developed Duration of anemia Metabolic requirements of patient Other disorders Cardio: tachycardia, hypoxia, MI symptoms Respiratory: SOB in varying degrees Neuro: headache, poor concentration, vertigo, irritibility, confusion Compensation also may occur Clinical manifestations (pg 2010) Prioritize activities Plan rest periods Eats healthy foods rich in iron, vitamins, and proteins Use nutrition supplements as needed Report palpitations, dizziness, dyspnea Monitor vitals Monitor edema Monitor neuro status Safety techniques Education Low RBC Low HGB andHCT Low serum Iron level Low ferritin level High TIBC level Results from diet low in iron Results from body not absorbing enough iron from GI tract ◦ Not enough hemoglobin made as result s/s: sore tongue, brittle nails, fatigue, pallor, orthostatic changes (in severe cases) Dx: bone marrow aspiration, lab work Tx: iron supplements, iron rich foods (liver, oysters, red meat, fish, dried fruits, legumes, dark green veggies, whole grain breads and cereal)---orange juice or other vitamin C product will enhance iron absorption ◦ What is the major side effect of IV iron? Iron Deficiency Anemia Pts don’t become severely anemic til creatinine levels exceed 3mg/100ml Hematocrit decreases Causes: ◦ shorted RBC lifespan ◦ Deficiency of erythropoietin ◦ Long term hemodialysis Tx: monitor serum levels of iron, hematocrit, and vitals Anemia and Renal Disease Only inflammation, infection, and malignancy cause It is nonprogressive Develops over 6-8 weeks Many don’t require treatment Anemia and chronic disease Most cases are idiopathic Infection and pregnancy, medication, chemicals or radiation can trigger ◦ Airplane glue, arsenic, pestisides Complete failure of the bone marrow Low RBC count Low WBC Low Platelet cts S/S: pallor, fatigue, tachycardia, sob, hypotension, prolonged/spontaneous bleed, frequent infections, purpura, retinal hemorrhages are common Tx: transfusion of RBC and Platelet, antibiotics, corticosteroids, bone marrow transplant, ICU setting, monitor for signs and symptoms of infection and bleeding, neutropenic precautions Aplastic Anemia Pt does not absorb vitamin B12 from stomach ◦ Higher incidence of gastric cancer Pt may lack intrinsic factor-essential for b12 absorption Assess hx: gastrectomy, crohn’s, family history,etc. s/s: weakness, sore tongue, numbness of hand and feet Tx: B12 injections monthly, endoscopy q1-2 years---if untreated can develop heart failure and lead to death ◦ Monitor oral cavity, and skin. Monitor for jaundice, monitor gait, provide small frequent bland diet Dx: Obtain shilling test Pernicious Anemia Most frequent in SE Asian, African, and Mediterranean descent Thalassemia Folate is in green leafy veggies and liver Alcohol increases need for folic acid S/S same as pernicious anemia except no neuro symptoms Dx: folate level Tx: replacements Folic Acid Deficiency RBCs normally disc shaped In sickle cell they are sickle shaped Easily rupture Obstruct blood flow Genetic in nature Most common in African Americans Sickle cell is recessive (inherit from mom and dad) Sickle cell anemia 3 types: ◦ sickle crisis: most common---obstructive ◦ aplasic crisis---from infection from parvovirus ◦ sequestrian crisis---result from other organs pooling sickled cells Spleen is most common Also in liver and lungs S/S: tachycardia, fever, decreased HGB, infiltrates on chest x-ray Pulomary HTN is a symptom that is not usually detected until damage is irreversible Monitor x-rays, CT scan, Echo, HGB level Tx: treat symptoms, Bone marrow transplant, transfusions, Hydroxyurea, Arginine Sickle Cell Crisis This is a deficiency in the gene that is essential for membrane stability Hemolysis only occurs with stressful situations Mostly affects african americans, greek or italian decent as well as asians and jewish origins Inherited on x chromosome S/S: asymptomatic, or jaundice, pallor, hemoglobinuria Dx: serum G-6-PD Tx: stop offending med, transfusion, educate about meds to avoid, instruct to wear medic alert bracelet Glucose -6-Phospate Dehydrogenase Deficiency Enough RBCs made but they are destroyed once they are released into circulation Causes: infection, drug reaction, cancer s/s: pallor, fatigue, tachycardia, sob, hypotension, jaundice, high bilirubin levels Positive direct coombs antiglobulin test Tx: blood transfusions, corticosteroids, spleenectomy Recovery in few days to weeks Autoimmune Hemolytic Anemia Too many RBCs produced s/s: headache, dizziness, ringing in the ears, blurred vision, ruddy complexion, HTN, pruritis, gout problems, burning fingers and toes DX: o2 sat, CBC with DIFF Complications: CVA, MI, BLEED issues Tx: hydroxyurea, interferon, plavix, ASA Treat symptoms Teach pt: don’t cross legs, quit smoking, stay active, minimal alcohol, avoid excess iron phlebotomize blood ◦ Blood more viscous Use 18 gauge needle In antecubital vein and remove I unit of blood Polycythemia Vera Defect in the WBC stem cell Abnormal reproductions Unknown cause, may be from chemical or radiation exposure Symptom onset is abrupt Leukemia Defective stem cell Incidence rises with age 60+ Prognosis variable Younger pts may survive 5 years S/S: fever, infection, weakness, fatigue, bleed tendency, pain Dx: no warning, CBC Complications: bleeding (petechiae, ecchymosis), infection, DIC TX: chemo, transfusions, infection treatment, growth factor agents, bone marrow transplant, palliative care AMLAcute Myeloid Leukemia Uncommon in pts under 20 Life expectancy 3-5 years s/s: asymptomatic, dyspnea, mild confusion, enlarged liver, wt loss, anorexia Tx: tyrosine kinase inhibitor, avoid antacids and grapefruit juice, interferon, cytosine, leukopheresis, bone marrow transplant CML Most common in young kids 4-14 Uncommon s/s: decreased cbc counts, pain, enlarged liver, enlarged spleen, headache, vomiting Tx: bone marrow transplant, chemo, corticosteroids Complications: infection Acute Lymphocytic LeukemiaALL Common in older adults Most common form in US and Europe More frequent in men s/s: asymptomatic, lymphadenopathy, pain, hepatomegaly, spleenomegaly, anemia, fevers, drenching sweats, wt loss, infections Tx: treat symptoms, chemo, monoclonal antibodies CLL Characterized by reed- sternberg cells in the lymph nodes Highest occurance is in 20s and50s Men are more likely than women to have Tx: radiation, chemo, bone marrow transplant, stem cell transplant Survival rates vary 5 yr survival rate is 82% Hodgkins Disease 6th most common type of cancer and cancer death in US ◦ Avg age of dx is 60 Stages ◦ Low grade ◦ Intermediate grade ◦ High grade The higher the grade the more aggressive Tx: chemo, radiation, bone marrow transplant, stem cell transplant 5 year survival rate is 52% Non Hodgkins Lymphoma Cancer of the plasma cells Most common over the age of 60 No known cause s/s: bone pain, hyperuricemia (kidneys), anemia, hypercalcemia, fractures, spinal cord compression, renal failure Diagnosis: radiographs, serum and urine protein electrophoresis, bone marrow biopsy No known cure Tx: chemo and radiation to treat symptoms, vertebroplasty, antiemetics, pain management ◦ Genetics and radiation exposure play a part Multiple Myeloma Bleeding disorders http://www.mhhe.com/biosci/esp/2002_general/Esp/folder_structure /tr/m1/s7/trm1s7_3.htm Clotting Cascade Too few platelets ◦ Causes: cancer treatment Too many platelets being destroyed ◦ Causes: idiopathic thrombocytopenic purpura, thrombic thrombocytopenic purpura Dx: bone marrow bx, CBC s/s: petechiae, purpura, gingival bleed, epistaxis, prolonged bleeding Tx: transfusions, spleenectomy, chemo, stop med that is causing, stop ETOH, treat infection Thrombocytopenia Most common among kids and young girls Usually 1-6 wks after viral infection Cause unknown, h. pylori may play role s/s: asymptomatic, low platelet count, petechiae, hemoptysis Dx: bone marrow bx, platelet ct Tx: stop med, immune globulin, chemo, Nsg: assess lifestyle, teach symptoms, avoid constipation, avoid valsalva, avoid teeth flossing, use only electric razors, use only soft bristled tooth brush, monitor for osteoporosis Immune thrombocytopenic purpura Example of drug induced immune mediated thrombocytopenia Rare Related to heparin therapy Tx: observation, assessment, monitor lab values HIT Most common inherited bleeding disorder 1-2% international population s/s: Mucosal and cutaneous bleeding, porlonged bleed times Tx: DDAVP, FFP, Cryoprecipitate, bleed precautions Von Willebrand’s Disease Thrombic Thrombocytopenic Purpura Genetic Lack of blood clotting factor 1-2 cases per 20,000 persons Types ◦ A: factor VIII is missing-higher incidence ◦ B: factor IX is missing Trait is carried on x chromosome Rare for women to have s/s: uncontrolled bleed especially in joints, skin, GI tract Tx: no cure. Transfusions, pain treatment (IV morphine is common)..monitor for addiction to opiods. Hemophilia Not a disease Triggers: sepsis, trauma, cancer, shock, abruptio placentae, allergic reactions Life threatening condition Initially coag time is normal S/S: are manifested in organs with either clots or bleeding. Bleeding from all orifaces(tear ducts, gums, IV sites, rectum, urethra, etc.) Dx: PT, PTT, D-Dimer Tx: treat the cause, replace fluids, o2, fix electrolyte imbalances, administering vasopressors are vital, cryoprecipitate to replace factor 5 and 7, FFP, heparin DIC Universal donor= O◦ Does not contain A, B, or Rh antigens Universal recipients= AB+ ◦ Blood contains A, B, and RH antigens Usually blood banks exactly match the pt blood Blood typing for transfusion Pt needs 18 or 20 gauge IV needle so cells are not lysed (destroyed) Prior to administration, blood needs to be checked by 2 licensed nurses. Check the expiration date, name, medical record number, type of blood, blood band id, pt birthday ◦ Check vitals prior to administration **blood must be initiated with in 30 minutes of arrival from lab to floor Use blood tubing for administration Monitor for blood reactions Monitor vitals continuously during administration adminstration on blood Hemolytic: fever, chills, nausea, dyspnea, chest pain, back pain, hypotension ◦ Antigen/antibody rx to transfusion ◦ Happens shortly after initiation ◦ Tx: stop the transfusion, call md, supportive therapy to maintain HR and BP Anaphylactic: urticartia, wheezing, dyspnea, hypotension ◦ Type 1 hypersensitivity rx to plasma proteins ◦ Occurs within 30 minutes of initiation ◦ Tx: stop transfusion, call md, be ready for epi and steroids Febrile: fever, chills ◦ Recipients antibodies rx to donor leukocyte ◦ Occurs within 30-90minutes of initiation ◦ Tx: stop infusion, call md Circulatory overload: cough, frothy sputum, cyanosis, decreased BP ◦ cardio system is unable to manage the additional fluid load ◦ Occurs anytime during transfusion and up to several hours after completion ◦ Tx: stop infusion, call for help, be prepared for code, be prepared to administer oxygen and Lasix Blood reactions Minimize the # of invasive procedure Avoid prolonged tourniquet use Avoid IM injections Instruct the client to use soft bristled tooth brush No strait edge razor shaving only use electric razor Avoid NSAIDS Bleeding precautions Nrsg diagnosis Risk for injury r/t bleed. Goal: cessation of bleeding aeb no visual signs of bleeding and stable vs Acute pain r/t bleeding into closed spaces(creating pressure on nerves. Goal: pain relief aeb: patient states pain is relieved and appears to be in relaxed manner. Ineffective therapeutic regimen management r/t lack of knowledge about dx process and self care. Goal: effective management of condition aeb patient accurately describes condition and demonstrates self care measures. ANY QUESTIONS???