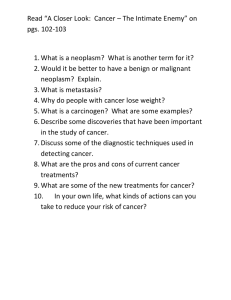
Neoplasia
advertisement

Neoplasia Pathophysiology of tumors and cancer 1 The following pictures and descriptions were found at: wwwmedlib.med.utah.edu/WebPath/NEOHTML 2 Cells normally differentiate, grow, mature and divide. These are regulated processes, balanced in a healthy system such that cell birth is nearly equal to cell death 3 Regulation of cell division includes: 1. Signaling by biochemicals released from one cell that interact with other cells growth factors or cytokines 2. Other external factors , such as contact inhibition 4 3. Genes and internal factors that promote and regulate cell division genes and chromosomal factors telomeres braking proteins – Rb proteins 5 A tumor cell’s growth is autonomous – independent of controls Neoplasm – a type of tumor – group of neoplasic cells Study of tumors is oncology from Greek for tumor 6 Two major types: Benign and Malignant (table 6.2) Benign: grow slowly low mitotic rate well differentiated not invasive; well-defined borders remain localized; do not metastasize 7 Any increase in tissue size is not necessarily neoplasia. Here is an example of left ventricular cardiac hypertrophy in which there has been an increase in the size of the myocardial fibers in response to an increased pressure load from hypertension. With hypertrophy, the cells increase in size, but the cells do not increase in number. Except for being larger, the cells are normal in appearance. Alterations in cell growth can be physiologic (normal responses to stimuli) or pathologic. These alterations of cell growth are potentially reversible and include: Hypertrophy: an increase in cell size. Increase in skeletal muscle fiber size is a physiologic response to exercise, but the cardiac hypertrophy shown above is a pathologic response to abnormally elevated blood pressure. Hyperplasia: an increase in the number of cells. Postpartum breast lobules undergo hyperplasia for lactation, but endometrial hyperplasia in a postmenopausal woman is abnormal. 8 9 The large fronds of endometrium seen in this uterus opened to reveal the endometrial cavity are a result of hyperplasia. This resulted from increased estrogen. With hyperplasia, there is an increase in cell numbers to produce an increase in tissue size. However, the cells are normal in appearance. Sometimes hyperplasias can be "atypical" and the cells not completely normal. Such conditions can be premalignant. 10 11 The first step toward neoplasia is cellular transformation. Here, there is metaplasia of normal respiratory laryngeal epithelium on the right to squamous epithelium on the left in response to chronic irritation of smoking. The two forms of cellular transformation that are potentially reversible, but may be steps toward a neoplasm, are: Metaplasia: the exchange of normal epithelium for another type of epithelium. Metaplasia is reversible when the stimulus for it is taken away. Dysplasia: a disordered growth and maturation of an epithelium, which is still reversible if the factors driving it are eliminated. 12 This is the next step toward neoplasia. Here, there is normal cervical squamous epithelium at the left, but dysplastic squamous epithelium at the right. Dysplasia is a disorderly growth of epithelium, but still confined to the epithelium. Dysplasia is still reversible. 13 Of course, neoplasms can be benign as well as malignant, though it is not always easy to tell how a neoplasm will act. Here is a benign lipoma on the serosal surface of the small intestine. It has the characteristics of a benign neoplasm: it is well circumscribed, slow growing, and resembles the tissue of origin (fat). 14 At low power magnification, a lipoma of the small intestine is seen to be well demarcated from the mucosa at the lower center-right. This neoplasm is so well-differentiated that, except for its appearance as a localized mass, it is impossible to tell from normal adipose tissue. 15 Remember that the most common neoplasm is a benign nevus (pigmented mole) of the skin, and most people have several, as seen here over the skin of the chest. As a general rule, benign neoplasms do not give rise to malignant neoplasms. 16 Malignant – cancer – from Latin for crab autonomy and anaplasia Grow rapidly ; high mitotic index, poorly differentiated; do not have a capsule; invade surrounding structures; can metastasize from the primary to a secondary site (metastasis). 17 Some epithelia are accessible enough, such as the cervix, that cancer screening can be done by sampling some of the cells and sending them to the laboratory. Here is a cervical Pap smear in which dysplastic cells are present that have much larger and darker nuclei than the normal squamous cells with small nuclei and large amounts of cytoplasm. 18 When the entire epithelium is dysplastic and no normal epithelial cells are left, then the process is beyond dysplasia and is now neoplasia. If the basement membrane is still intact, as shown here, then the process is called "carcinoma in situ" because the carcinoma is still confined to the epithelium. 19 This is a neoplasm. Neoplasia is uncontrolled new growth. Note the mass of abnormal tissue on the surface of the cervix. The term "tumor" is often used synonymously with neoplasm, but a "tumor" can mean any mass effect, whether it is inflammatory, hemodynamic, or neoplastic in origin. Once a neoplasm has started, it is not reversible. 20 This is the microscopic appearance of neoplasia, or uncontrolled new growth. Here, the neoplasm is infiltrating into the underlying cervical stroma. 21 This gastric adenocarcinoma is positive for cytokeratin by immunoperoxidase. This is a typical staining reaction for carcinomas and helps to distinguish carcinomas from sarcomas and lymphomas. Immunoperoxidase staining is helpful to determine the cell type of a neoplasm when the degree of differentiation, or morphology alone, does not allow an exact classification. 22 Here is a small hepatic adenoma, an uncommon benign neoplasm, but one that shows how well-demarcated an benign neoplasm is. It also illustrates how function of the normal tissue is maintained, because the adenoma is making bile pigment, giving it a green color. 23 In contrast, this hepatocellular carcinoma is not as well circumscribed (note the infiltration of tumor off to the lower right) nor as uniform in consistency. It is also arising in a cirrhotic (nodular) liver. 24 Malignant neoplasms are also characterized by the tendency to invade surrounding tissues. Here, a lung cancer is seen to be spreading along the bronchi into the surrounding lung. 25 This is an example of metastases to the liver. Note that the tan-white masses are multiple and irregularly sized. A primary neoplasm is more likely to be a solitary mass. Metastasis is the best indication that a neoplasm is malignant. 26 Here are three abnormal mitoses. Mitoses by themselves are not indicators of malignancy. However, abnormal mitoses are highly indicative of malignancy. The marked pleomorphism and hyperchromatism of surrounding cells also favors malignancy. 27 Nomenclature – In General : Tissue of origin + “-oma” indicates a benign tumor 28 Malignant tumors – use embryonic origin of tissue Carcinomas come from ectoderm and Endoderm - epithelial and glandular tissue Sarcomas arise from mesoderm connective tissue, muscle, nerve and endothelial tissues 29 Genetic Basis of cancer • Older theory : Initiation-promotionprogression • “Multi-hit” hypothesis • Cancer is a disease of aging • Clonal proliferation 30 Several cellular control pathways must be altered to produce cancer: Autonomy – proliferate in the absence of external growth signals autocrine stimulation increase in growth factor receptors post-receptor signal cascade inside the cell stuck in the “on” position 31 Overcome antigrowth signals: contact with basement membrane, other cells inactivation of tumor suppressor genes or activation of the cyclindependent kinases that drive the cell Prevention of apoptosis 32 Oncogenes in non-mutant state called proto-oncogenes stimulate cell growth and replication when turned “on” by mutation cause uncontrolled growth 33 Tumor suppressor genes negatively regulate proliferation antioncogenes want these to remain intact takes two “hits” to remove both genes 34 35 Gene silencing regions of genes normally turned off can spread without mutation and turn off tumor suppressor genes drugs that demethylate DNA may turn genes back on 36 Loss of caretaker genes Chromosomal instability 37 Angiogenesis angiogenic factors or vascular endothelial growth factor (VEGF) possible source of new therapies 38 Telomerase Other factors: decreased cell-to-cell adhesion secretions of proteases ability to grow in new locations 39 Genetics and cancer prone families to be passed down, mutations must occur in germ cells inherited mutations almost always in tumor suppressor genes (table 9-6) these individuals are targets for cancer screening 40 Viral causes of cancer: viruses assoc. with about 15 % of cancers world wide – us. Cervix or liver hepatitis B or C in chronic form Human papilloma virus spread through sexual contact HPV integrates into DNA and uses viral oncogenes 41 Epstein-Barr and Kaposi sarcoma both herpes viruses Human T cell leukemia-lymphoma virus blood transfusions, needles, sex and breast feeding infections may be asymptomatic may have high incidence, but low #’s of cancer cofactors increase the risk of cancer 42 Bacterial causes of Cancer Helicobacter pylori infects >1/2 world’s population assoc. with B cell lymphomas of the stomach treatment with antibiotics can cause regression of lymphoma Tumors arise in MALT -MALTomas 43 Environmental factors • • • • • • • • Tobacco use Diet Alcohol use Sexual and reproductive behavior Air pollution Occupation hazards – asbestos UV radiation and other radiation hormones 44 Gene-Environment Interactions: Exposure to environmental agents can cause increased risk of cancer cancer in lab animals – carcinogens Comparisons of populations genetics vs. lifestyle 45 “Genetics loads the gun; the environment pulls the trigger.” director of Nat’l Institute of Environmental Health & Safety 46 Diagnosis: screening procedures and blood tests: Tumor markers substances on plasma membranes in blood, spinal fluid or urine hormones, genes antigens or antibodies 47 Markers can be used: to screen and identify individuals at high risk to help diagnose the specific type of tumor to follow the course of the cancer 48 Tumor spread • Local spread – Cellular multiplication • Function of generation time • Growth if cell reproduction > cell death 49 Mechanical invasion along path of least resistance compresses blood vessels, leading to tissue death and increased space 50 Lytic enzymes proteases, collagenases, plasminogen activators, lysosomal enzymes some involved in producing new blood vessels 51 Decreased cell adhesion loss of anchoring molecules allows cancer to slip between normal cells 52 Increased motility essential for metastasis intravasation extravasation may secrete autocrine motility factor extend psuedopodia three step hypothesis: attachment to the matrix dissolution of the matrix locomotion through the matrix 53 Stages of cancer spread: Stage 1 – confined to site of origin Stage 2- cancer is locally invasive Stage 3 – cancer has spread to regional structures Stage 4- cancer has spread to distant sites 54 TNM system: tumor spread node involvement presence of distant metastasis Staging may influence choice of treatment 55 Staging TNM system 1.Size of tumor – T0, T1, T2,T3 2.Degree of local invasion – lymph node involvement 3.Extent of spread – metastasis 56 Patterns of spread: Metastasis • Direct or continuous extension • By lymphatics or blood stream – As clumps or as single cells – Lymphatics most common 57 Patterns of spread: Metastasis • Angiogenesis – Due to production of angiogenic factors – Due to drop in antiangiogenic factors 58 A metastasis grows when: vascular network is developed host defenses are evaded a compatible environment is available 59 Distribution and common sites of distant metastases • often occurs in the first capillary bed encountered •Others show “organ tropism” •Due to: •Local growth factors or hormones •Preferential adherence to the surface •Presence of chemotactic factors 60 Clinical manifestations of Cancer • Pain – Usually not in early stages – 60 – 80 % of terminally ill – Psychogenic, cultural and physiologic components – Due to pressure, obstruction, stretching, tissue damage or inflammation 61 Branches of peripheral nerve are invaded by nests of malignant cells. This is often why pain associated with cancers is unrelenting. 62 Clinical manifestations of Cancer Fatigue sleep disturbances biochemical changes loss of muscle function 63 Clinical manifestations of Cancer Cachexia – wasting anorexia early satiety weight loss anemia marked weakness taste alterations altered metabolism 64 Clinical manifestations of Cancer Anemia chronic bleeding malnutrition medical therapies malignancy in blood forming organs Administer erythropoietin 65 Clinical manifestations of Cancer Leukopenia and thrombocytopenia tumor invasion of bone marrow chemotherapy or radiation 66 Clinical manifestations of Cancer • Paraneoplastic Syndromes – Release of hormones by cancer cells – Hematological complications such as procoagulation factors – Causes weakness by attacking neuromuscular junction (similar to myasthenia gravis) 67 Clinical manifestations of Cancer • Infection • most significant cause of complications and death 68 Cancer Treatment • Chemotherapy – Cytotoxic drugs + body defenses • Single agent • Combination chemotherapy –Avoids single agent resistance –Can use lower dose –Better remission and cure rate 69 Cancer Treatment Radiation targets DNA kill tumor without damage to surrounding tissues tumor must be accessible 70 Cancer Treatment Surgery method of choice can remove entire tumor debulking adjuvant chemotherapy or radiation palliation 71 Cancer Treatment Immunotherapy Nonspecific enhancement of the immune system – interferons or interleukins protect against recurrence eliminates cancer cells only T- cell based or antibody responses Conjugated antibodies 72 Cancer Treatment • Targeted Therapies – Drugs that target the processes of cancer cells specifically • Thalidomide – Vaccines 73 Side effects of treatment • Gastrointestinal tract: – Oral ulcers – Malabsorption – Diarrhea – Vomiting – caused by effects on CNS 74 Side effects of treatment Bone marrow: chemo and radiation suppress bone marrow decrease in red blood cells, white blood cells and platelets 75 Side effects of treatment Hair and skin: alopecia skin breakdown and dryness 76 Side effects of treatment Reproductive tract: affects gametes premature menopause also due to damage of hypothalamus and/or pituitary sperm or embryo bank 77