Positive Expiratory Pressure (PEP) Therapy Overview
advertisement

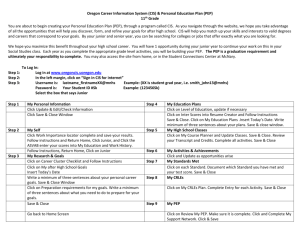
Positive Expiratory Pressure Therapy PEP Overview What is PEP? History of PEP Current PEP Devices Clinical Evaluation Conclusion What is PEP? PEP is a form of bronchial hygiene, and is one of the 3 adjuncts of positive airway pressure (PEP, CPAP, and EPAP). PEP involves active expiration through a oneway valve against a variable flow resistor. In modern PEP devices, flow resistance can be manipulated to adjust for a desired pressure. What does PEP do? Enhances secretion mobilization and removal Helps prevent infections Helps mitigate atelectasis Improved pulmonary mechanics and gas exchange How does PEP accomplish this? 2 ways: 1. Filling under-inflated or collapsed alveoli via collateral ventilation (pores of Kohn, Canals of Lambert).* 2. Helping to stint the airways open during expiration. History of PEP Origin of PEP -Traditional CPT with manual percussion, postural drainage, and vibration was first introduced in 1901 to assist airway clearance in children with bronchiectasis. -In the 1970’s PEP devices were developed in Denmark, as a means to aid the patient’s airway clearance with an effective, self-administered low-pressure device (mouth piece @ 5-20 cm H20). -High-pressure PEP therapy was developed in Austria (face mask @ 26-102 cm H20). -In 1991, PEP was introduced in the U.S. by Louise Lanafours from Sweden. -Since 1991, PEP devices have been modified and improved upon, which have produced devices such as the TheraPEP and Acapella. Current PEP Devices Airway Oscillation Devices (AOD) Provide standard PEP with the added benefit of oscillating pressure within the airway Oscillations reduce the viscoelasticity of mucus Oscillations provide short bursts of increased expiratory airflow to help with secretion mobilization Flutter Valve TheraPEP Acapella Current PEP Devices Flutter Valve Developed in Switzerland Pipe-shaped AOD with a steel ball resting in an angled bowl. On exhalation, the ball oscillates at approximately 15 Hz, and provides 1025 cm H20. Gravity dependent Current PEP Devices TheraPEP Designed by Smiths Medical Company Standard low-flow PEP device Built in pressure indicator Can be used with a mask or mouthpiece Has a 22mm OD which allows it to be docked with a nebulizer Inspiratory and expiratory valves Provides 10-20 cm H20 Current PEP Devices Acapella Designed by Smiths Medical Company Similar to the flutter valve but with greater functionality (AOD) Utilizes a counterweighted plug and magnet to achieve valve closure (not gravity dependent) 3 Models: Low flow ( < 15 L/min, adjustable resistance) High flow ( > 15 L/min, adjustable resistance) Choice (any flow, adjustable frequency) What’s so great about PEP? Readily accepted by patients Shorter treatment time compared to CPT Independent use Inexpensive (Acapella $32.00 @ Amazon) Portable BUT…is it as effective as other methods of bronchial hygiene? VS What does the research say? Cystic Fibrosis – Standard PEP Mortensen et al: PEP vs. PD&P Darbee et al: PEP vs. HFCWC Both showed the same increase in FVC, FEV1, and sputum clearance. McIlWaine et al: PEP vs. PD&P Equally effective in secretion clearance PEP had greater improvement in FEV1 and FVC Patients preferred PEP because they felt it was more effective, required less time, independent, and easier. Oberwaldner et al: PEP vs. PD&P PEP produced a significantly greater sputum volume, expiratory flow rate, and decreased hyperinflation compared to PD&P. Summary: These studies show conflicting results. At the least, we can conclude that standard PEP is just as effective as PD&P and HFCWC for CF patients. What does the research say? Chronic Bronchitis – Standard PEP Christensen et al: Diaphragmatic breathing /FET vs. PEP/FET PEP group had greater secretion clearance, lower exacerbation rate, lower rate of mucolytic and antibiotic use, and an increase in FEV1. What does the research say? Cystic Fibrosis – OPEP Newhouse et al: Flutter vs. IPPV Hominick et al: Flutter vs. PD&P Equally effective in sputum clearance Flutter was more effective at increasing FEV1 and FVC Konstan et al: Flutter vs. PD&P Equally effective in sputum production, and increasing expiratory flows. Flutter produced significantly more sputum. Flutter was assessed to be safe, cost effective, easy to use, and with greater patient adherence. Gondor et al: Flutter vs. PD&P Flutter showed significant improvement in FVC compared to PD&P No difference in length of hospital stay Summary: Again, these studies show conflicting results, but at the least OPEP is shown to be just as effective as traditional methods of CPT for CF patients. What does the research say? Chronic Bronchitis – OPEP Bellone et al: Flutter vs. PD&P Flutter had superior sputum production / clearance. Research Conclusions What conclusions can be drawn from the research? The majority of the research regarding the efficacy of PEP has been conducted on CF patients. In some studies, PEP and OPEP have been shown to have superior secretion clearance and improvements in pulmonary function than traditional methods of CPT. However, other research clearly refutes these results, placing PEP as only as effective as traditional methods. Thus, the choice to utilize PEP as a primary method of bronchial hygiene therapy should be made on the basis of other criteria, such as cost and patient compliance. Conclusion PEP devices such as the Acapella are small, portable, cost effective, and patient preferred. PEP devices haven’t been shown to be superior to other forms of CPT, but they haven’ been proven inferior either. Continued research on the efficacy of PEP devices needs to be conducted. At this time, the effectiveness of PEP devices has been shown to be equal or better than traditional methods of bronchial hygiene, and the decision to use PEP devices should be made on the basis of other factors, such as cost effectiveness. References Diomou G., Hristara-Papadopoulou A., Papadopoulou O., and Tsanakas, J. Current devices of respiratory physiotherapy. Hippokratia 2008 Oct-Dec;12(4):211–220. Kacmarek, R.M., Stoller, J.K., Wilkins, R.L. (2009). Egan’s Fundamentals of Respiratory Care (9th ed.). St. Louis, MO: Mosby Inc. Myers, Timothy R. "Positive expiratory pressure and oscillatory positive expiratory pressure therapies." Respiratory Care Oct. 2007: 1308+. Academic OneFile. Web. 25 Nov. 2011. University of Wisconsin-Madison. (2011). Health Informatin: TheraPEP [Data file]. Retrieved from http://www.uwhealth.org/healthfacts/B_EXTRANET HEALTH_IN FORMATION-FlexMember-Show_Public_HFFY_1115126486611.html Wilson, Richard., (Feb-March 1999) Positive Expiratory Pressure Therapy: The Key to Effective, Low-Cost Removal of Bronchial Secretions. RT Magazine. Retrieved from http://www.rtmagazine.com/issues/articles/1999-02_08.asp References Bellone A, Lascioli R, Raschi S, Guzzi L, Adone R. Chest physical therapy in patients with acute exacerbation of chronic bronchitis: effectiveness of three methods. Arch Phys Med Rehabil 2000;81(5): 558-560. Christensen EF, Nedergaard T, Dahl R. Long-term treatment of chronic bronchitis with positive expiratory pressure mask and chest physiotherapy. Chest 1990;97(3):645-650. Darbee JC, Kanga JF, Ohtake PJ. Physiologic evidence for high-frequency chest wall oscillation and breathing in hospitalized subjects with cystic fibrosis. Phys Ther 2005;85(12):1278-1289. Gondor M, Nixon PA, Mutich R, Rebovich P, Orenstein DM. Comparison of flutter device and chest physical therapy in the treatment of cystic fibrosis pulmonary exacerbation. Pediatr Pulmonol 1999; 28(4):255260. Homnick DN, Anderson K, Marks JH. Comparison of the flutter device to standard chest physiotherapy in hospitalized patients with cystic fibrosis. A pilot study. Chest 1998;114(4):993-997. Konstan MW, Stern RC, Doershuk CF. Efficacy of the Flutter device for airway mucus clearance in patients with cystic fibrosis. J Pediatr 1994;124(5 Pt 1):689-693. McIlwaine PM, Wong LT, Peacock D, Davidson AG. Long-term comparative trial of conventional postural drainage and percussion versus positive expiratory pressure physiotherapy in the treatment of cystic fibrosis. J Pediatr 1997;131(4):570-574. Mortensen J, Falk M, Groth S, Jensen C. The effects of postural drainage and positive expiratory pressure physiotherapy on tracheobronchial clearance in cystic fibrosis. Chest 1991;100(5):1350-1357. Myers, Timothy R. "Positive expiratory pressure and oscillatory positive expiratory pressure therapies." Respiratory Care Oct. 2007: 1308+. Academic OneFile. Web. 22 Nov. 2011. Newhouse PA, White F, Marks JH, Homnick DN. The intrapulmonary percussive ventilator and flutter device compared to standard chest physiotherapy in patients with cystic fibrosis. Clin Pediatr (Phila) 1998;37(7):427-432. Oberwaldner B, Evans JC, Zach MS. Forced expirations against a variable resistance: a new chest physiotherapy method in cystic fibrosis. Pediatr Pulmonol 1986;2(6):358-367.