Module 5 – Pediatric Cardiac Disorders
advertisement

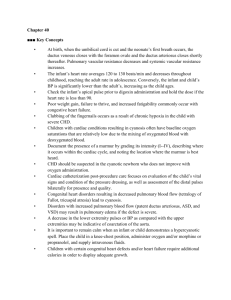
Module 5 Pediatric Cardiac Disorders Fetal Circulation Fetal Circulation Fetal Circulation What is the stimulus for the change in circulation? Intrauterine to Extrauterine Oxygen Saturation What is oxygen saturation? What is normal oxygen saturation levels? What values indicate hypoxemia? Why is it important for the nurse to know the oxygen saturation levels? Congestive Heart Failure What is wrong with the heart? Congestive heart failure What is the effect on: Heart rate Preload Contractitility Afterload Congestive Heart Failure Why does the pump fail? Etiology and Pathophysiology *Congenital defects *Acquired heart diseases Congestive Heart Failure What does the body do to compensate for this congestion and heart failure? Compensatory Mechanisms With a decrease in Cardiac Output Stimulation of the sympathetic nervous system Tachycardia - increases venous return to the heart which stretches the myocardial fibers and increases preload. Compensatory Mechanisms Decrease perfusion to the kidneys and glomerulus With a decrease in cardiac output Increased renin and ADH secretion Increase in Na and H2O retention to increase intravascular volume Early Signs of CHF The earliest signs are often subtle: Infant will have mild resting tachypnea Increasing difficulty feeding Signs and Symptoms Pulmonary congestion 1. Tires easily during feeding 2. Tachypnea, Dyspnea, orthopnea 3. Signs of respiratory distress 4. Wheezing, rales and rhonchi 5. Easily fatigue Impaired cardiac output 1. Tachycardia 2. Extremities cool, capillary refill >2 seconds 3. Diaphoretic, sweating, hypotension Signs and Symptoms Systemic venous congestion 1. Hepatomegaly 2. Edema 3. Weight gain High metabolic rate 1. Failure to thrive 2. Slow weight gain Goal of Treatment Decreasing Cardiac Workload Improving Cardiac Output Treatment of Congestive Heart Failure Medication Therapy Digitalis – increases contractility and decreases heart rate. ACE-inhibitors - blocks release of angiotensionaldosterone; arterial vasodilator / afterload reducing agent Diuretics - enhance renal secretion of sodium and water by reducing circulating blood volume and decreasing preload, pulmonary congestion. Beta Blocker - increases contractility Nursing Care How would the nurse recognize digitalis toxicity in an infant or child? What are the pulse rate criteria in administration of digitalis? Digitalis Digitalization Maintenance Given in divided doses Given daily, usually in two divided doses Therapeutic vs. Toxicity Therapeutic range – 0.8 to 2.0 ng/ml Toxicity **EKG changes – arrhythmia Slow pulse- bradycardia Vomiting – very rare in infants Digitalis Why are we so concerned with the potassium levels when the child is on digitalis therapy? Treatment of Congestive Heart Failure What is the type of Diet most commonly ordered? How would nursing measure are used to decrease stress on the heart? Feeding the child with CHF Feed the infant or child in a relaxed environment; frequent, small feedings may be less tiring Hold infant in upright position; may provide less stomach compression and improve respiratory effort If child unable to consume appropriate amount during 30-minute feeding q 3 h, consider nasogastric feeding Monitor for increased tachypnea, diaphoresis, or feeding intolerance (vomiting) Concentrating formula to 27 kcal/oz may increase caloric intake without increasing infant’s work Cardiac Catheterization Measure oxygen saturations and pressure in the cardiac chambers and great arteries Evaluate cardiac output Cardiac Catheterization This process involves passing a catheter through the femoral vein or artery into the heart. Performed to evaluate heart valves, heart function and blood supply, or heart abnormalities in newborns. Cardiac Catheterization Pre-care: History and Physical Lab work – EKG, ECHO cardiogram, CBC NPO Vital signs Preprocedural teaching Best Nursing Action During post procedure assessment, the nurse notes bleeding at the insertion site. What should the nurse do first? What additional interventions are implemented? Post Cardiac Catheterization Care Post Cardiac Catheterization Care Congenital Cardiac Anomalies Ask Yourself? What is the most common assessment finding indicating a cardiac anomaly? Answer: an audible heart murmur Patent Ductus Arterious Atrial septal defects Ventricle septal defects Atrial Septal Defect 1. Oxygenated blood is shunted from left to right side of the heart via defect 2. A larger volume of blood than normal must be handled by the right side of the heart hypertrophy 3. Extra blood then passes through the pulmonary artery into the lungs, causing higher pressure than normal in the blood vessels in the lungs congestive heart failure Treatment Medical Management Cardiac Catheterizaton Medications – digoxin Amplatzer septal occluder Open-heart Surgery Treatment Device Closure – Amplatzer septal occluder During cardiac catheterization the occluder is placed in the Defect Ventricle Septal Defect 1. Oxygenated blood is shunted from left to right side of the heart via defect 2. A larger volume of blood than normal must be handled by the right side of the heart hypertrophy 3. Extra blood then passes through the pulmonary artery into the lungs, causing higher pressure than normal in the blood vessels in the lungs congestive heart failure Treatment Surgical repair with a patch inserted Patent Ductus Arteriosus 1. Blood shunts from aorta (left) to the pulmonary artery (right) 2. Returns to the lungs causing increase pressure in the lung 3. Congestive heart failure Treatment for PDA Medical Management Medication Indomethacin - inhibits prostaglandin's . (When levels of prostaglandins are decreased, the ductus closes) Surgery Ligate the ductus arteriosus Treatment for PDA Cardiac Catheterization Insert coil – tiny fibers occlude the ductus arteriosus when a thrombus forms in the mass of fabric and wire Cardiac Anomalies - Treatment Pulmonic stenosis coarctation of aorta Pulmonic Stenosis Narrowing of entrance that decreases blood flow Increases preload causes right ventricular hypertrophy Obstructive or Stenotic Lesions Treatment: Medications – Prostaglandins to keep the PDA open Cardiac Catheterization Baloon Valvuloplasty Surgery Valvotomy Aortic Stenosis The aortic valve is thickened and rigid Stenosis creates left ventricular hypertrophy Left ventricle may not be large enough to eject a normal cardiac output. Aortic Stenosis Symptoms Poor peripheral perfusion, feeding difficulties, CHF Treatment Balloon valvoplasty Surgery Coarctation of the Aorta 1. Narrowing of Aorta causing obstruction of left ventricular blood flow 2. Left ventricular hypertrophy Signs and Symptoms 1. What are B/P findings support the diagnosis? 2. What is different in the pulses? 3. Why would the patient C/O leg pains? 4. What causes nose bleeds? Treatment Goals of management are to improve ventricular function and restore blood flow to the lower body. Medical management with Medication A continuous intravenous medication, prostaglandin (PGE-1), is used to open the ductus arteriosus allowing blood flow to areas beyond the coarctation. Baloon Valvoplasty Surgery for Coarctation of Aorta 1. Resect narrow area 2. Anastomosis Tetralogy of fallot Tetralogy of Fallot Four defects are: 1. 2. 3. 4. Signs and Symptoms 1. Failure to thrive 2. Squatting 3. Lack of energy 4. Infections 5. Polycythemia 6. Clubbing of fingers 7. Cerebral abscess 8. Cardiomegaly Ask Yourself? Why does Polycythemia occur in a child with a cardiac disorder? What nursing interventions should be included when planning care for this child? What lab test will be abnormal and assist in confirming the polycythemia? Ask Yourself ? Laboratory analysis on a child with Tetralogy of Fallot indicates a high RBC count. The polycythemia is a compensatory mechanism for: a. Tissue oxygen need b. Low iron level C. Low blood pressure d. Cardiomegaly Hypercyanotic Episode / “tet” spells Cyanosis suddenly worsens in response to activity, such as crying, feeding, or having a bowel movement. Signs - The infant becomes very short of breath with tachypnea and hyperpnea, and may lose consciousness. Treatment – calming, knee-chest position, oxygen, morphine , and beta-blockers Treatment Open-heart Surgical interventions Blalock – Taussig or Potts procedure – increases blood flow to the lungs. Something the Lord Made View the Movie Trailer About Blalock procedure to treat Tetralogy of fallot • • Truncus Arteriosus Transportation of Great Vessels These present the greatest risk to survival Truncus arteriosus A single arterial trunk arises from both ventricles that supplies the systemic, pulmonary, and coronary circulations. A vsd and a single, defective, valve also exist. Entire systemic circulation supplied from common trunk. Transposition of Great Vessels Aorta arises from the right ventricle, and the pulmonary artery arises from the left ventricle - which is not compatible with survival unless there is a large defect present in ventricular or atrial septum. artery aorta Microorganisms grow on the endocardium, forming vegetations, deposits of fibrin, and platelet thrombi. The lesion may invade adjacent tissues such as aortic and mitral valves. Subacute Bacterial Endocarditis / Infective Endocarditis: Assessment: Fever Fatigue Muscle and joint pain Headache Nausea and vomiting CHF Spleenomegaly Diagnosis: Blood cultures Echocardiogram Infective Endocarditis Diagnosis Blood cultures Echocardiogram Show the vegetation Who is more susceptible to develop infective endocarditis? What is the most therapeutic intervention for preventing infective endocarditis? Antibiotic Prophylaxis for Children at Risk for Infective Endocarditis Dental procedures, including cleaning, that may induce gingival or mucosal bleeding Tonsillectomy and/or adenoidectomy Surgery and/or biopsy involving respiratory or intestinal mucosa Incision and drainage of infected tissue Invasive GU and GI procedures Ineffective Endocarditis Treatment Monitor temperature Antibiotics – 2-8 weeks Patient teaching Good oral hygiene take antibiotics prior to surgery, dental work, or any invasive procedure, etc. discouraged from body piercing and tattoos as endocarditis may occur even with prophylaxis. A systemic inflammatory (collagen) disease of connective tissue that usually follows a group A beta-hemolytic streptococcus infection. This disorder causes changes in the entire heart (especially the valves), joints, brain, and skin tissues. Rheumatic Fever - Assessment Major Carditis Polyarthritis Chorea Erythema marginatum Subcutaneous nodules Minor Jones Criteria Arthralgia Fever Laboratory Findings: Erythrocyte sedimentation rate C-reactive protein Prolonged PR interval What additional laboratory test helps to confirm the diagnosis of Rheumatic Fever ? Rheumatic Fever Treatment Antibiotic Therapy Antipyretics - aspirin Anti-inflammatory agents –steroids Rest Heat and cold to joints Discharge Teaching Antibiotic therapy - be sure to complete all medication. Streptococcal Prophylaxis for the Child with Rheumatic Fever Damaged valves can become further damaged with repeated infections Streptococcal prophylaxis is lifelong if there is actual valve involvement Intramuscular penicillin, administered monthly, is the drug of choice Alternatives include oral penicillin twice daily or oral sulfadiazine once a day Multisystem vasculitis – inflammation of blood vessels in the body especially the coronary arteries with antigen-antibody complexes. Kawasaki Disease Signs and Symptoms / Treatment Three Phases of clinical manifestations: Acute Subacute Convalesant One of the most common symptoms used to diagnose Kawasaki disease is a high spiking fever over 1020 for 5 days. Acute Phase – 10-14 days Fever, which often is higher than 101.3 F, and lasts one to two weeks Extremely red eyes (conjunctivitis) without thick discharge Red, dry, cracked lips and an extremely red, swollen tongue ("strawberry" tongue) A rash on the main part of the body (trunk) and in the genital area Swollen, erythema on the palms of the hands and the soles of the feet Swollen cervical lymph nodes Subacute Phase 15-25 days Irritability Anorexia Desquamation of the skin on the hands and feet, especially the tips of the fingers and toes, often in large sheets Arthritis and Arthralgia Arrhythmias Coronary aneurysms Convalescent Phase From day 26 until the erythrocyte sedimentation rate returns to normal Nursing Care Give Medications Promote comfort Lubricate the lips Cool compresses Keep skin cool and dry Small feedings of soft foods and liquids that are not too hot or too cold. Facilitate joint movement Passive Range of Motion exercises Aspirin Intravenous Immunoglobulin Kawasaki Disease Which phase of Kawasaki is this child exhibiting? Inflamed, Cracked, Peeling Lips Strawberry tongue Kawasaki Disease