Pulmonary Embolism
advertisement

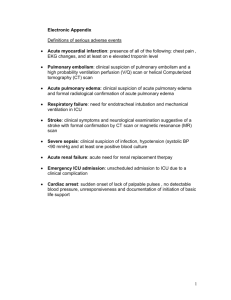
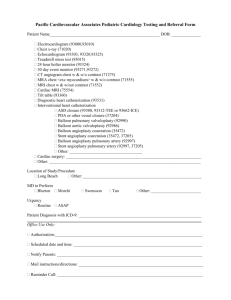
Asuncion Camille Ann, Mejia Maria Margarita, Liwanag Harvy Joy ASMPH Batch 2012 The Medical City – RADIOLOGY Rotation I. Case Presentation II. Salient Features A. B. III. Pertinent History Pertinent Physical Examination Differential Diagnoses and Diagnostics A. B. C. D. E. Asthma Pneumonia Coronary Artery Disease Dissecting Aortic Aneurysm Pulmonary Embolism IV. Diagnostic Approach (PIOPED and ESC) A. Triple Rule-Out by CT Angiography 1. 2. 3. 4. 5. 6. B. Procedure Indications Contraindications Applicability to age group Costing Expected Findings Other Considerations Primary Impression V. A. Epidemiology B. Pathophysiology C. Clinical Correlations VI. Summary 50 y/o chief complaint: chest pain and difficulty of breathing sudden in onset pain was stabbing and non-radiating DOB associated with bouts of cough Differentials? Fresh from a 17-hour flight Pain in the calf pain, relieved by rest Past Medical HPN, controlled DM, uncontrolled No previous surgeries Differentials? OB-Gyne G5P5 (5005) History of OCP intake Personal and Social Non-smoker, non-alcohol beverage drinker OFW from Europe Vitals: stable, afebrile Clear breath sounds, (-) retractions, (-) alar flaring Right leg edema with slight discoloration Unequal pulses in lower extremities ECG: Nonspecific ST wave elevation Urinalysis and CBC unremarkable Results of cardiac enzymes: pending Differentials? Differential Rule-in Rule-out Laboratories & Other Diagnostics Radiologic Studies Asthma (+) difficulty of breathing and cough (+) acute attack (-) history of asthma Clear breath sounds Blood WU: Eosinophils , IgE & allergic skin testing Pulmonary function tests Peak flow monitoring Metacholine- or histamine-challenge testing PA and lateral Chest X-rays to rule-out pneumomediastinum Pneumonia (+) difficulty of breathing and cough (+) acute onset (+) DM prone to infections Clear breath sounds (-) fever Normal WBC Sputum gram stain and/or culture and sensitivity CBC Bronchoalveolar lavage (BAL) PA chest xray Differential Rule-in Rule-out Laboratories & Other diagnostics Radiologic Studies Coronary artery disease (+) chest pain (+) acute attack (+) history of hypertension and DM (-) radiation Stable VS Non-specific ECG findings Blood WU: CBC, thyroid function tests Lipid profile Cardiac enzyme serum markers ECG Echocardiography CT angiography Intravascular ultrasound Optical coherence tomography Aortic dissection (+) chest pain Uneven pulses Stable VS Blood WU: CBC, (-) back pain BUN, creatinine, LDH, D-dimer Cardiac enzymes Smooth muscle myosin heavy-chain assay Echocardiography ECG PA Chest x-ray mediastinal widening (40%); right tracheal deviation; pleural effusion CT scan – for hemodynamically stable patients Differential Rule-in Pulmonary embolism (+) chest pain (+) history of air travel Multiparous (+) difficulty of breathing and coughing Acute attack Uneven pulses Rule-out ----- Laboratories & Other Radiologic Diagnostics Studies D-dimer Serum troponin Brain natriuretic peptide Arterial blood gases ECG Chest radiography (PA and lateral) CT Angiography Color flow doppler (for thrombophlebitis) Pulmonary Embolism RATIONALE Expected Findings ECG Assess status of R ventricle, risk T wave inversion (V1-V4), QR stratification Pattern (V1), S1Q3T3 type and incomplete or complete R bundle branch block CXR Exclude other causes of dyspnea and chest pain Plate-like atelectasis, pleural effusion, elevation of hemidiaphragm CBC Hemodynamic stability or anemia, check for infection Usually normal CARDIAC ENZYMES Markers of myocardial injury High ABG Assess blood oxygenation Hypoxemia but 20% have N PaO2 and D(A-a)O2 D-Dimer Rapid ELISA Indicates presence of an acute clot High First radiologic study done for chest pain and/or dyspnea Consider radiation exposure, age of patient, pregnancy Costing: P560-690 (TMC) Normal or near-normal Enlarged right descending pulmonary artery (Palla’s sign) Focal oligemia (Westermark’s sign) Peripheral wedge-shaped density above the diaphragm (Hampton’s hump) Westermark’s sign Palla’s sign Hampton’s Hump Clinical Judgment Prospective Investigation On Pulmonary Embolism Diagnosis (PIOPED) Clinical probability (low, moderate, high) ▪ Clinical prediction rules (Geneva, Wells) PIOPED I: V/Q scan PIOPED II: CTA PIOPED III: Gd-MRA PROCEDURE: Uses 64-MDCT technology Single, non-invasive test for “acute chest pain dilemma” CAD, PE, AD Protocol: Includes lung apex and base Longer contrast injection Patient Preparation: Beta-blockers and nitrates (lower heart beat and dilate coronaries) ECG gating Oxygen may be inhaled COSTING: P20,000-P27,000 (TMC) Halpern E, 2009 Low to moderate risk for acute coronary syndrome (ACS) Symptoms attributed to acute pathologic conditions of the aorta or pulmonary arteries (dyspnea, acute chest pain) Halpern E, 2009 ABSOLUTE CONTRAINDICATIONS RELATIVE CONTRAINDICATIONS Hypersensitivity to iodinated contrast agent History of allergies or allergic reactions to other medications Renal insufficiency (serum creatinine level of >1.5 mg/dL) Congestive heart failure History of thromboembolic disorders Multiple myeloma Hyperthyroidism Pheochromocytoma Atrial fibrillation Inability to perform breath hold for 15 s Hoffman et al., 2006 - central intravascular filling defect within the vessel lumen (“doughnut sign”, “Polo mint sign”) - eccentric tracking of contrast material around a filling defect - complete vascular occlusion http://radiographics.rsna.org/content/24/5/1219/F13.expansion.html - Smooth filling defects making an obtuse angle with a vessel wall http://radiographics.rsna.org/content/24/5/1219/F13.expansion.html - Lung Parenchyma oligemia - Lung Parenchyma pulmonary hemorrhage (peribronchovascular thickening, ground-glass attenuation, smooth interlobular septal thickening) http://radiographics.rsna.org/content/24/5/1219/F13.expansion.html - Lung Parenchyma pulmonary infarction (peripheral wedge-shaped pleural-based opacification) Acute Embolus Chronic Embolus Central, within vascular lumen Eccentric and contiguous with vessel wall Vessel cutoff sign Reduces arterial diameter by >50% Evidence of recanalization within thrombus Presence of an arterial web Central PE (Central Vascular Zones) Peripheral PE (Peripheral Vascular Zones) main pulmonary artery segmental and subsegmental arteries of the right upper lobe left and right main pulmonary arteries right middle lobe anterior trunk right lower lobe right and left interlobar arteries left upper lobe left upper lobe trunk lingula the right middle lobe artery left lower lobe right and left lower lobe arteries Second-line (to CTA) diagnostic test Radiologic modality for patients who cannot tolerate IV contrast Uses radio-labeled inhaled gases (e.g. xenon, krypton) High probability scan: two or more segmental perfusion defects with normal ventilation 90% positive predictive value for highprobability scans Pulmonary Embolism Category: acute pulmonary infarction or acute embolism without infarction Epidemiology: 1 per 1000 (USA) Pathophysiology • • • • • Venous thrombosis: venous stasis, injury to the intima, enhanced coagulation properties of blood Thrombus formation: platelet nidus on the valves of the veins of the lower extremities accretion & growth red fibrin thrombus break off (embolus) or occlusion Clinical Presentation: chest /abdominal pain, difficulty of breathing, productive cough, wheezing, fever, seizures, syncope, decreasing level of consciousness, new onset atrial fibrillation, flank pain, delirium (in elderly patients) Most common symptoms (PIOPED): dyspnea (73%), pleuritic chest pain (66%), cough (37%), hemoptysis (13%) Most common physical signs (PIOPED): tachypnea (70%), rales (51%), tachycardia (30%), fourth heart sound (24%), accentuated pulmonic component of the second heart sound (23%) Most common symptoms (PIOPED): dyspnea (73%), pleuritic chest pain (66%), cough (37%), hemoptysis (13%) Most common physical signs (PIOPED): tachypnea (70%), rales (51%), tachycardia (30%), fourth heart sound (24%), accentuated pulmonic component of the second heart sound (23%) Risk factors: immobilization, travel (4 hours or more in the past month), surgery (within the last 3 months), malignancy, history of thrombophlebitis, trauma, smoking, stroke, paresis, paralysis, heart failure, COPD Case application: Patient presented with dyspnea and chest pain History of travel (17 hours) and immobilization Pregnancy (G5P5) Thrombophlebitis – unilateral edema Use of OCPs Anticoagulation & Fibrinolysis Heparin, Warfarin Maintenance of hemodynamic stability Monitoring of oxygenation and cardiac function Consider embolectomy Combination of mechanical and pharmacologic modalities Compression stockings Mini-doses of anticoagulants (heparin) Helical CT Pulmonary Angiography for Acute Pulmonary Embolism [Appl Radiol 31(4):21-30, 2002. © 2002 Anderson Publishing, Ltd] http://www.medscape.com/content/2002/00/ 43/30/433087/433087_fig.html PIOPED II ESC CPGs on Pulmonary Embolism Harrisons Principles of Internal Medicine Asuncion Camille Ann, Mejia Maria Margarita, Liwanag Harvy Joy ASMPH Batch 2012 The Medical City – RADIOLOGY Rotation