Clinical Evaluation of PE - Ipswich-Year2-Med-PBL-Gp-2
advertisement

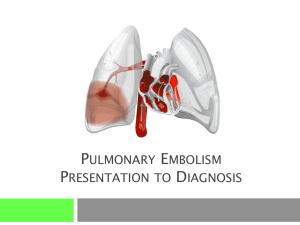
Clinical Evaluation of PE This is an important and interesting topic because an incorrect diagnosis has serious consequences regarding both a false negative (patient with PE is undiagnosed) or false positive (patient without PE is treated with anticoagulants increasing risk of bleeding complications). A lot of work has been done on developing diagnostic algorithms, allowing the doctor to make a rapid judgement of suspected PE, allowing him to go on to ordering further tests that lead to a definitive diagnosis. I’ll start off with the patient presenting with typical signs and symptoms then focuses on specific risk factors PC Most common presenting complaint: dyspnoea Chest pain Syncope Cough Leg pain HPC Dyspnoea is sudden and unexplained Chest pain. The classic presentation is “sudden onset”, however, 40% have experienced nagging pain for weeks prior to diagnosis and admission (or death). The pain can manifest as either: o Non pleuritic chest pain (visceral) including upper abdominal pain, back pain, shoulder pain o Pleuritic chest pain (infarction) that arises within the chest wall; is tender, severe, sharp and increases on inspiration. Syncope indicates a massive PE Fever, diaphoresis, apprehension due to inflammation Palpitations, tachycardia Hemoptysis, cough Signs of DVT Summary of Risk Factors 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Prolonged immobilization (> 3 days) Postoperative state Trauma to lower extremities Pregnancy and early puerperium Cancer (lung, pancreas, alimentary and genitourinary tracts) Trauma, burns Advanced age (>60) Obesity Hematologic disease (e.g., antithrombin III deficiency, protein C deficiency, protein S deficiency, lupus anticoagulant, polycythemia vera, dysfibrinogenemia, paroxysmal nocturnal hemoglobinuria, factor V Leiden mutation, G20210A prothrombin mutation) COPD, diabetes mellitus Prolonged air travel Oestrogen-containing birth control pills Prior history of DVT or PE CHF Examination Often unremarkable Pleuritic rubbing sound may be auscultated indicating an infarct. Crackles may also be heard. Tachypnoea Cardiovascular changes following a massive PE: o Shock o o Elevated JVP Right ventricular heave (heel of hand is placed over left parasternal region and lifted off with each systole) o Mitral regurgitation o Increased S3 on inspiration (the galloping heart has a sound like the “Kentucky Derby”: Ken(S1)tuck(S2)-y(S3) at the lower left sternal border and the –y increases with inspiration) o Loud, early P2 component (pulmonary valve closure) of S2 (in other words, the second heart sound (S2 made up of P2 and A2) is split because of early closure of the pulmonary valve (P2) ahead of the aortic valve (A2) due to increased pulmonary artery pressure caused by the embolism Evidence of DVT (calf swelling, pain, inflammation). Below is an example of a risk based algorithm (Wells Clinical Prediction Tool) but there are others and each hospital has its own variation: Table. Risks for Pulmonary Embolism Variable Points Clinical signs and symptoms of deep vein thrombosis (pain and leg swelling with palpation of the deep veins) 3 Alternative diagnosis less likely than pulmonary embolism 3 Heart rate > 100/minute 1.5 Immobilization > 3 days or surgery in the previous 4 weeks 1.5 Previous pulmonary embolism or deep venous thrombosis 1.5 Haemoptysis 1 Malignancy treated within the last 6 months 1 Risk score interpretation (probability of DVT): >6 points: high risk (78.4%); 2 to 6 points: moderate risk (27.8%); <2 points: low risk (3.4%) Therefore, the goal is to determine the pre-test risk of the patient having a PE and the subsequent testing regime will be determined by this ie: So, relating this to our case of big Bill; he as clinical signs of a DVT (swelling, leg pain, discolouration, Homan’s test+) and haemoptysis and it is arguable whether he has been immobile for at least 3 days (sedentary yes, but not necessary immobile). Therefore his pre-test probability of having a PE is moderate (28%). Therefore, starting him off on D-Dimer Rapid ELISA was correct and was found to be positive, necessitating further investigations (if his D-dimer was –ve then we’d have to look for other causes for his leg pain – a good discussion point). The pre-test probability is important in interpreting subsequent CT angiography because, the higher the pre-test probability (based on your clinical assessment), the lower the negative predictive value of a negative CT angiogram and may necessitate further testing (MRI venography). The opposite is true if there is a low pre-test probability because subsequent CT angiography has a lowered PPV (58%), necessitating further testing, such as MRI venography. The following tables summarise this: Finally, a high pre-test probability means +ve CT angiography almost certainly means he has a PE (PPV 96%) whereas there’s greater doubt over a negative scan (NPV 60% requiring further imaging.