Urethral Strictures - North West Urology Registrar Group
advertisement

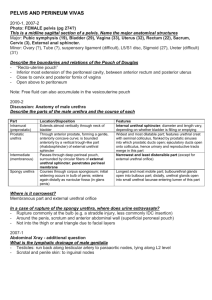
Urethral Strictures Causes Diagnosis Assessment Treatment options Prognosis References Curriculum • • • • • • • • • • • • Knowledge of the pelvis, male genitalia and urethra including embryology of urethra including hypospadias and epispadias Neuroanatomy as it relates to normal and abnormal bladder, urethral and pelvic floor function Causes, pathophysiology and complications of urethral strictures Pathophysiology of traumatic urethral injury Assessment of patient with urethral stricture Ability to determine appropriate surgical option for patients with urethral stricture Be able to advise on the surgical options and the appropriateness of surgery Knowledge of endourological techniques relevant to urethral stricture Techniques and complications of urethral reconstruction Management of postoperative consequences of urethral reconstruction Arrange appropriate follow up of patients with urethral reconstruction Liaison with other specialties e.g. radiology, orthopaedics, GI surgeons Definitions The term urethral stricture refers: • to anterior urethral disease • is a scarring process that involves the epithelium as well as the spongy erectile tissue of the corpus spongiosum. • Con- traction of the scar reduces the urethral lumen. In contrast, posterior urethral strictures are more correctly referred to as pelvic fracture urethral injuries; strictures of the prostatic urethra or bladder neck are properly referred to as contrac- tures or stenoses. Chapple et al, BJUI 2004 Anatomy Blood supply Neuroanatomy Neuroanatomy Neuroanatomy of the male urethra and perineum, BJUI 2003 Distribution • Anterior – 92.2% • Posterior – 7.8% Palminteri et al. Contemporary urethral stricture characteristics in the developed world. Urology 2013 Aetiology Unknown 41.3 Failed hypospadias repair 17.0 Catheter 9.9 Instrumentation 6.2 Radiotherapy 0.6 TURP 1.3 Trauma 15.8 LS 6.9 Infection 0.8 Congenital 0.2 Stein et al. A geographic analysis of male urethral stricture aetiology and location. BJUI, 2013 Aetiology Stein et al. A geographic analysis of male urethral stricture aetiology and location. BJUI, 2013 Pathology Noxious stimulus (bacterial, chemical, physical) Denuded epithelium Squamous metaplasia Fissures develop in epithelium Urine extravasation Fibrosis develops in the corpus spongiosum Fibrotic plaques coalesce Stricture Mundy et al. Urethral strictures, BJUI 2010 Pathology of anterior stricture Campbell’s Urology, 2011 Pathology of contractures/stenoses • Shearing forces transmitted through the perineal membrane and pubo-prostatic ligament • Distraction-avulsion most commonly at bulbomembranous junction • Transection by the bony fragments – rare • Partial or complete ruptures • Fibrosis interposed between the distracted ends Case 1 • 40 Male • 6/12 h/o flow problem presenting at your clinic.... Presentation • Obstructive LUTS: poor stream, incomplete bladder emptying, hesitancy, dribbling • Urinary tract infections • Acute urinary retention • Haematuria • Asymptomatic Investigations • The aim is to determine: location, length, depth and density of the stricture/spongiofibrosis. Campbell’s Urology. 2011 Investigations • Flow studies • Flexible endoscopy – urethral – suprapubic – Does not show length, proximal urethra • Radiology – Contrast studies- retrograde urethrogram, voiding cystogram. – USS useful for bulbar strictures? limited Case 1 • Flow studies: • Flexible cystoscopy: At 12 cm Urethrogram? ‘there are many urologists who think that a urethrogram is not necessary before deciding upon treatment, mainly because they are going to do a urethrotomy anyway. This is not the authors’ view. Urethrography gives a more complete assessment.’ Mundy et al. Urethral strictures. BJUI 2010 Treatment • Management •Cure Both the patient and the physician must have a good understanding of the goal of treatment before the treatment choice is made. To this end, treatment options should be discussed with the patient, with care taken to emphasize the anticipated outcome with regard to potential cure. Campbell’s Urology, 2011 Treatment ‘In the absence of complications, treatment is for symptoms and if the symptoms are not particularly troublesome, treatment is symptoms are not troublesome, treatment is unnecessary’ Mundy et al. Urethral strictures. BJUI 2010 Treatment • Reconstructive ladder – archaic • Dilatation: – oldest/simplest – epithelial stricture without spongiofibrosis – stretch the scar, avoid bleeding – Results equal to optical urethrotomy Treatment Mundy et al. Urethral strictures. BJUI 2010 Treatment - Optical urethrotomy - Where to cut? Thinnest portion of corpus spongiosum at 12 o’clock at bulb. Easy to penetrate the corpus cavernosum - Radial cuts better? - If wound contraction occurs before re-epithelisation then the stricture recurs. - Post-op catheter 3 days TONKIN et al. Management of distal anterior urethral strictures. Nat Rev Urol. 2009 Desmond et al. Critical evaluation of direct vision urethrotomy by urine flow measurement. Br J Urol 1981 Treatment - Optical urethrotomy Adjuvant modalities to reduce the rate of stricture recurrence include the following: • Intermittent self-catheterisation • Steroids injected at the site of IU • Anti-inflammatory medication by mouth • Mitomycin-C injected transurethrally • Brachytherapy using an intraurethral balloon filled with radio-active isotope • Captopril gel intra-urethrally Heyns. Urethral stricture: should we stop urethrotomies? EAU 2011 Treatment - Optical urethrotomy -Complications: 1. urine extravasation 2. pain 3. UTI 4. ED1 1. McDermott et al. Erectile impotence as complication of direct vision cold knife urethrotomy. Urology 1981 Recurrence post optical urethrotomy ? always? 49 50 Albers. J Urol 1996 40 30 25 26 Heyns. J Urol 1997 27 19 20 Pansadoro. J Urol 1996 Charbit. Ann Urol 1990 10 0 McAninch. AUA 2001 Long term success (> 4years) Recurrence post optical urethrotomy – factors • Length of the stricture (longer than 2 cm) • Extent of spongiofibrosis on ultrasound (or stricture diameter on retrograde urethrography) • Previous procedures (UD, IU, UP) • Shorter time to stricture recurrence after IU or UD • Longer duration of follow-up (although most strictures that recur, do so within 12 months) Heyns. Urethral stricture: should we stop urethrotomies? EAU 2011 Case 1 continued • 4/12 post urethrotomy pt is back in the clinic saying symptoms re-occurred... Treatment • Management •Cure Both the patient and the physician must have a good understanding of the goal of treatment before the treatment choice is made. To this end, treatment options should be discussed with the patient, with care taken to emphasize the anticipated outcome with regard to potential cure. Campbell’s Urology, 2011 Case 1 continued • Options: – 1. Repeat urethrotomy, UD, Laser, Stent • Rate of success v. low (6%)1 – 2. Open surgery (urethroplasty) • Rate of success depending on the pathological features of the stricture. 1. Santucci et al. Urethrotomy has a much lower success rate than previously reported. J Urol 2010 Treatment Laser – no evidence – Ideal laser should • totally vaporise tissue • cause negligible peripheral tissue destruction • not absorbed by water • suitable fibre – Carbon dioxide ideal, needs gas cystoscope, CO2 embolus – Argon/Nd:Yag causes thermal necrosis can injure peripheral tissues – Holmium YAG Treatment - Stents – Wallstent or UroLume® (Pfizer Inc., UK) which is incorporated into the urethral wall – Memokath® (Engineers & Doctors A/S Ltd., Hornbaek, Denmark) which is not. Results are v. poor- De Vocht et al BJU 2003. Makes reconstruction more difficult. UroLume® Memokath® Repeat urethrotomy • 1. A second DVIU/dilation can be indicated for recurrent urethral strictures with favourable characteristics (<1-2 cm, single, bulbar stricture) with recurrence >3 months after previous treatment (B). • 2. A third DVIU/dilation is not recommended, except if necessitated by patient comorbidities or economic resources (A). • 3. Urethral reconstruction over repeat DVIU/dilation should be offered for urethral strictures that recur within 6 months or are refractory to a second DVIU/dilation (A). Heyns et al. SIU/ICUD Consultation on Urethral Strictures: Dilation, Internal Urethrotomy, and Stenting of Male Anterior Urethral Strictures. Urology 2014 Repeat urethrotomy • Issue the cost effectiveness of a repeat DVIU vs urethroplasty • Greenwell et al. Repeat urethrotomy and dilatation for the treatment of urethral stricture are neither clinically effective not cost effective. J Urol 2004 • Rourke et al. Primary urethral reconstruction: the cost minimised approach to the bulbous urethral stricture. J Urol 2005 Open Trial in UK • Randomised, multicentre trial of open urethroplasty versus endoscopic urethrotomy • For men who have got 1st recurrence of stricture Case 1 continued • Pt opts for open surgery... Treatment Bulbar urethroplasty Penile urethroplasty Posterior urethral reconstruction Bulbar urethroplasty • Anastomotic or substitution? • Ventral or dorsal graft location? • One stage or two stage repair? Barbagli. EAU 2008 Treatment – anastomotic urethroplasty • Indications – < 2cm- historically – bulbar urethra – relies on mobilisation of corpus spongiosum • Best results – excise stricture – spatulated anastomosis – overlaping ends • Outcomes – long term success over 90 – 95%1-2 1. R.A. Santucci et al. Anastomotic urethroplasty for bulbar urethral stricture: analysis of 168 patients. J Urol. 2002 2. G. Barbagli et al. One-stage bulbar urethroplasty: retrospective analysis of the results in 375 patients. Eur Urol. 2008 Treatment – anastomotic urethroplasty Complications • • • • Ejaculatory dysfunction 20% Decreasedd glans sensitivity 18% Poor glans erection 11% Cold glans 1.6% Barbagli. EAU 2008 Augmented anastomosis with graft onlay Grafts/Flaps • Graft ‘tissue excised from a donor site which re-establishes its blood supply by revascularisation’ • Process by which revascularisation occurs = ‘take’ • Take = 3 to 4 days • 2 processes – imbibition and inosculation Imbibition • 48 hours • Graft survives by ‘drinking’ nutrients from host bed • Graft temperature lower than host temperature Inosculation • 48 hours • Development of true circulation • Graft temperature rises to that of host • Features affecting ‘take’: -Graft type -Donor site vascularity (tendon, smoking) -Infection -Movement Grafts examples • Skin (full thickness, split thickness) • Buccal mucosa • Bladder mucosa • Rectal mucosa Skin vs Buccal mucosa Cornified layer Oral epithelium Epidermis Superficial lamina (submucosa) Papillary dermis Deep lamina (submucosa) Reticular dermis Muscle and minor salivary glands Buccal Mucosa Graft • • • • • • • Easy to harvest Easy to handle Thick Panlaminar vascular plexus – good take Waterproof Antibacterial Resists skin diseases Harvesting buccal mucosa • • • • • • • • Normal intubation OK vs. nasal intubation Avoid Stensen’s duct opposite second upper molar Mark excision site 0.5% lignocaine and adrenaline Tenotomy scissors (superficial vs. deep) 2cm wide, at least 1cm from vermillion border Side effects worse for closure vs. secondary intention Lignocaine lozenges Flaps • Penile/preputial • Based on Dartos • Useful when infection or extensive fibrosos present • Transverse, Longitudinal, Circumferencial Onlay urethroplasty methods Augmented urethroplasty Barbagli dorsal onlay BMG Bulbar urethroplasty - outcomes • Ventral OMG – 90% • Lateral OMG – 83% • Dorsal OMG - 77 Barbagli. EAU 2008 Penile urethroplasty • One stage or two stage repair? • Flap or graft urethroplasty? Barbagli. EAU 2008 Penile urethroplasty Special circumstances • BXO – avoid skin flaps/grafts as it is a skin condition – buccal mucosa is better Special circumstances • Options – Dilatation – Holmium laser stricturotomy – Urethrotomy (avoid 6 o’clock) – Urethrotomy + AMS sphincter – Open reconstruction – Urinary diversion Post TURP stricture • Tend to be at bladder neck (incise) • More difficult at membranous urethra since incision here will compromise continence as bladder neck mechanism lost • Gentle ISD • Anastomotic urethroplasty + sphincter (problems with erosion) • Multistage scrotal flap technique Thank you