Assessment of Protein Status - Central Washington University
advertisement

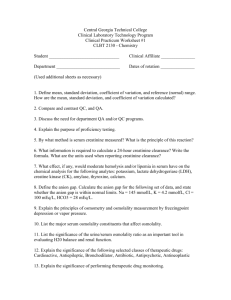
Assessment of Protein Status FCSN 442 - Nutrition Assessment Laboratory Dr. David L. Gee Central Washington University Assessment of Protein Status Anthropometric Assessment – body composition estimations – midarm muscle circumference/area Laboratory Assessment – serum albumin – other serum proteins (transferrin, prealbumin, retinol-binding protein) – urinary creatinine excretion – total lymphocyte count Midarm Muscle Area Estimate of MAMA is an estimate of overall muscle mass – single point vs serial measurements Assumptions – arm, muscle, bone are circular – TSF is 2X the thickness of fat – bone area is constant Midarm Muscle Circumference MAMC = AC - (.314 x TSF) – MAMC = midarm muscle circumference in cm – AC = arm circumference in cm – TSF = tricep skinfold in mm “…change in arm muscle area is greater than the change in mid-arm circumference. Consequently, changes in upper-arm musculature are not as easily detected by measurement of mid-arm circumference as by AMA. Therefore, AMA is the preferred nutritional index.” Arm Muscle Area AMA = ((MAC - (3.14 x TSF)2 ) / (4 x 3.14) – AMA = arm muscle area (cm2) – MAC = mid-arm circumference (cm) – TSF = tricep skinfold thickness (cm) • Or units of AMA, MAC, TSF all in mm • To convert mm2 to cm2, divide mm2/100 adjusted AMA – corrected for “bone free” AMA • Subtract constant from AMA to account for bone, nervous tissue, vascular tissue. – p-304 Table 7.6 Guidelines for Interpreting Percentile Values for Arm Muscle Area (appendix R) Percentile Category < 5th pct Wasted 5th -15th pct Below Average 15th - 85th pct Average 85th – 95th pct Above Average > 95th pct High Muscle Biochemical Assessment of Protein Status Two protein compartment model – Somatic protein (skeletal muscle protein) • ~75% of total body protein – Visceral protein (internal organs, blood cells, serum proteins) • ~ 25% of total body protein “No single test or group of tests can be recommended at this time as a routine and reliable indicator of protein status.” Young, 1990 “…a combination of measures can produce a more complete picture of protein status.” – Biochemical, anthropometric, dietary, and clinical findings Serum Albumin Major serum protein – Synthesized in liver – Maintains serum osmolarity – Serum carrier of small molecues Most common indicator of depleted protein status Serum Albumin Half life = 14-20 days – large body pool poor indicator of early protein depletion and repletion Levels affected by rate of synthesis (liver disease may reduce levels) May reflect level of physiological stress – Decreased during acute catabolic phase Serum Albumin Levels affected by abnormal losses – thermal burns – losses at burn site – nephrotic syndrome – losses in urine – protein-losing enteropathies – losses in feces Levels affected by fluid status – congestive heart disease & fluid overload • Reduced due to dilution – Dehydration • Increased due to concentration effects Normal values: 4.5 g/dL + 35-50 (SD) Serum Transferrin Function: transport protein for iron half-life = 8-9 days – better index of changes of protein status Influenced by other factors – Increased with iron deficiency – increased during pregnancy, estrogen therapy – reduced in protein-losing enteropathy, nephropathy, acute catabolic stress limited usefulness in protein status assess. Serum Prealbumin aka. transthyretin and thyroxine-binding prealbumin functions: – transport protein for thyroxine – carrier protein for retinol binding protein short half life (2-3d), small body pool – sensitive indicator of protein status – responds more rapidly than albumin or transferrin Serum Prealbumin Returns to normal at beginning of nutritional therapy – therefore do not use as endpoint for terminating nutritional therapy Influenced by other factors – increased in chronic renal failure on dialysis – reduced in acute catabolic states, post surgery, tissue trauma, sepsis generally considered preferable than albumin and transferrin Retinol Binding Protein Function: carrier for retinol – complexes with prealbumin (1:1) responds like prealbumin very rapid turnover (12 hours), very small body pool – may be too sensitive and complicates precise measurements generally not considered to be more useful than prealbumin Immunocompetence Immune system affected by nutritional status Tests of immunocompetence useful functional indicators of nutritional status Delayed Cutaneous Hypersensitivty (DCH) – intradermal injection of antigens Total Lymphocyte Count (TLC) Total Lympocyte Count White blood cell count – elevated with infections – used with % lymphocyte to get total lymphocyte count (TLC) TLC = (%lymp x WBC)x100 – ex: TLC=(37.2%x4100)x100 =1525 cells/mm3 Total Lympocyte Count Normal = 1200-1800 cells/mm3 Moderate PCM = 800-1200 Severe PCM = < 800 Urinary Creatinine Excretion Creatinine excreted in proportion to muscle mass LBM estimated by comparing 24-hr urine creatinine excretion with standard based on stature or reference values of 23 and 18 mg/kg for M and F Example: Joe is 5’10” tall, 178cm 70kg 24hr creatinine excretion = 1436 mg Expected creatinine @23mg/kg = 23 x 70 = 1610 mg % expected = 1436/1610 x 100 = 89% Creatinine Height Index CHI = (24 hr urine creatinine x 100) / (expected 24 hr urine creatinine for height) – CHI = 1436/1596 x 100 = 90% expected values in table 9-1 (p306) – – – – CHI > 80% = normal CHI = 60-80% = mild protein depletion CHI = 40-60% = moderate depletion CHI < 40% = severe depletion