Calcium
advertisement

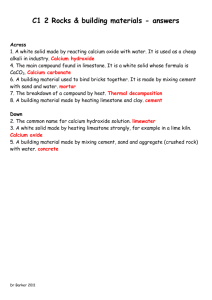
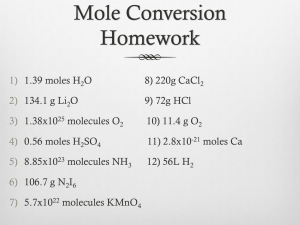
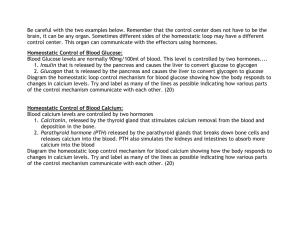
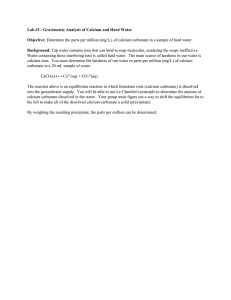
By Susan Skanderup Jensen Calcium facts • • • • • • • • • Soft grey alkaline earth metal Symbol Ca Number 20 Group II Divalent cation Atomic weight 40 g/mol Single oxidation state +2 Fifth most abundant element in Earth´s crust Essential for living organisms Calcium history • Latin calx or calcis meaning ”lime” • Known as early as first century when ancient Romans prepared lime as calcium oxide • Isolated in 1808 by Englishman Sir Humphrey Davy - Electrolyzed a mixture of lime & mercuric acid • In 1883 demonstrated Sydney Ringer the biological significance of calcium - Frog hearts needed the presence of calcium in the bathing solution in order to continue beating Calcium occurrence In nature • Does not exist freely • Occurs mostly in soil systems as limestone (CaCO3), gypsum (CaSO4*2H2O) & fluorite (CaF2) In the body • The most abundant mineral • Average adult body contains app. 1 kg • 0,1 % in the extra cellular fluid • 1 % in the cells • The rest (app. 99 %) in the skeleton (Bones can serve as large reservoirs, releasing calcium when extracellular fluid concentration decreases and storing excess calcium) Measuring calcium • Atomic absorption spectrometry (AAS) can measure total amount of Ca2+ in tissue • Fluorescent dyes can be used to measure Ca2+ in vivo • Calcium sensor (GFP-based) fluorescent protein “cameleon” is non invasive and can be targeted to various cellular compartments – enabling a study of spatial and organellar aspects of calcium homeostasis • Neutron activation analysis enables total body calcium to be measured in living persons • Bone mineral content (BMC) and bone mineral density (BMD) are used as indicators of calcium insufficiency and as predictors of increased risk of fracture, when compared to a reference range, adjusted for age and gender Calcium functions • Major structural element in the vertebrate skeleton (bones and teeth) in the form of calcium phosphate (Ca10(PO4)6(OH)2 known as hydroxyapatatite • Key component in the maintenance of the cell structure • Membrane rigidity, permeability and viscosity are partly dependent on local calcium concentrations Calcium functions (Bone) • Osteoclasts (bone cells) remodel the bone by dissolving or resorbing bone • Osteoblasts (bone forming cells) synthesize new bone to replace the resorbed bone - Found on the outer surfaces of the bones and in the bone cavities Calcium functions Plays important regulatory roles in the body A passive role: - As a cofactor for many enzymes (e.g. Lipase) and proteins As component in the blood clotting cascade An active role: as an intracellular signal - In the relaxation and constriction of blood vessels In cell aggregation and movement In muscle protein degradation In secretion of hormones as insulin In cell division In nerve impulse transmission Interactions • • • • Phosphate: ↓ calcium excretion in the urine Caffeine: ↑ urinary and fecal excretion of calcium Sodium: ↑ sodium intake, ↑ loss of calcium in urine Dietary constituents: Phytic acid can reduce absorption of calcium by forming an insoluble salt (calcium phytate) • Iron: calcium might have inhibitory effect on iron absorption Absorption and excretion • Usual intakes is 1000 mg/day • About 35 % is absorbed (350 mg/day) by the intestines • Calcium remaining in the intestine is excreted in the feces • 250 mg/day enters intestine via secreted gastrointestinal juices and sloughed mucosal cells • 90 % (900 mg/day) of the daily intake is excreted in the feces • 10 % (100 mg/day) of the ingested calcium is excreted in the urine • Calcium must be in a soluble and ionized form before it can be absorbed Absorption and excretion factors • Absorption increased by: • Excretion increased by: - - Body need Vitamin D Protein Lactose Acid medium Low parathyroid hormone (PTH) High extracellular fluid volume High blood pressure Low plasma phosphate Metabolic alkalosis • Absorption decreased by: • Excretion decreased by: - Vitamin D deficiency Calcium-phosphorus imbalance Oxalic acid Phosphorous Dietary fiber Excessive fat High alkalinity Also stresses and lack of exercise - High parathyroid hormone Low extracellular fluid volume Low blood pressure High plasma phosphate Metabolic acidosis Vitamin D3 Metabolism • Factors involved in calcium metabolism Transport mechanism Active and passive transport mechanisms • Active: is a saturable, transcellular process which involves calbindin (calciumbinding protein) – regulated by the active form of vitamin D • Passive: is a nonsaturable, paracellular low efficiency process, which is not affected by calcium status or parathyroid hormone • Both processes occur throughout the small intestine Regulation Vitamin D, parathyroid hormone and calcitonin • Vitamin D (in active form) - Has several effects on the intestine and kidneys that increase absorption of calcium and phosphate into the extracellular fluid Important effects on bone deposition and bone absorption • Parathyroid hormone (PTH) - Provides powerful mechanism for controlling extracellular calcium and phosphate concentrations by regulating intestinal reabsorption, renal excretion and exchange between the extracellular fluid and bone of the two ions • Calcitonin (a peptide hormone secreted by the thyroid gland) - Tends to decrease plasma calcium concentration In general, has effects opposite to those of PTH (quantitative role is far less than that of PTH in regulating Ca ion concentration) Regulation Activation of vitamin D3 - Cholecalciferol formed in the skin by sun - Converted in liver (feedback effect) - 1,25 DHCC formation in kidney - Controlled by PTH - Plasma calcium concentration inversely regulates 1,25 DHCC Regulation • • Compensatory responses to decreased plasma ionized calcium concentration mediated by PTH & vitamin D PTH regulates through 3 main effects: - By stimulating bone resorption By stimulating activation of vitamin D → ↑ intestinal Ca reabsorption By directly increasing renal tubular calcium reabsorption Adequate daily intake (AI) Life Stage Age Males (mg/day) Females (mg/day) Infants 0-6 months 210 210 Infants 7-12 months 270 270 Children 1-3 years 500 500 Children 4-8 years 800 800 Children 9-13 years 1,300 1,300 Adolescents 14-18 years 1,300 1,300 Adults 19-50 years 1,000 1,000 Adults 51 years and older 1,200 1,200 Pregnancy 18 years and younger - 1,300 Pregnancy 19 years and older - 1,000 Breastfeeding 18 years and younger - 1,300 Breastfeeding 19 years and older - 1,000 Calcium sources • Rich calcium sources (600-961mg/100g) - Cheese Wheat-soy flour Blackstrap molasses • Good sources (122-354mg/100g) - Dairy products as milk, yoghurt, sour cream, ice cream Green leafy vegetables as collard, kale and raw turnip Fish as trout, salmon and sardines Almonds, brazil nuts, dried figs, hazel nuts Also soybean flour and cottonseed flour • Poor sources - Most fresh fruit Deficiency • A negative calcium balance occurs when net calcium absorption is unable to replace losses • The most dramatic symptoms are manifested in the teeth and bones of young humans and animals → stunted growth, poor quality of bones and teeth and malformation of bones • Hypocalcaemia (low serum calcium levels in the blood cause the nervous system to become more excited) • Osteoporosis (bone resorption exceeds formation) - Occurs particularly in women. Increases in bone loss and osteoporotic fracture with age is a consequence of calcium deficiency • Osteomalacia, tetany and kidney stones are other calcium related diseases Causes of deficiency • • • • • Low Ca2+ intake Vitamin D deficiency Insufficiency or failure of parathyroid gland Chronic kidney failure Low blood magnesium level (in cases with severe alcoholism) • Diet high in phytate Toxicology • The UL for calcium is 2500 mg/day • MAS (Milk alkali syndrome) - Rare and potentially life threatening condition in individuals consuming large quantities of calcium and alkali - Characterized by renal impairment, alkalosis and hypercalcemia: cause progressive depression of the nervous system Human health studies • Resent studies showed - - - - Calcium may play a substantial contributing role in reducing the incidence of obesity and prevalence of the insulin resistance syndrome High calcium intake is associated with a plasma lipoproteinlipid profile predictive of a lower risk of coronary heart disease compared with a low calcium intake Dairy product intake (with recommended calcium levels) protect women consuming oral contraceptives from spine and hip bone loss Children who avoid drinking cow milk have low dietary calcium intakes and poor bone health Conclusion • Calcium is essential!!! • A important mineral for human health • Must meet adequate daily intake in order to maintain a healthy skeleton • A very exciting area for research Additional slide • Interaction with iron • An absorption depressing effect of calcium on iron absorption has been clearly demonstrated in single-meal studies and short-term diet intervention studies (Hallberg et al. 1991) • An addition of 150 mg of calcium to bread or a hamburger meal reduced iron absorption by 50 %. The interaction is suggested to take place within the mucosal cells as both haem and nonhaem iron is affected (Hallberg et al. 1993) • Long term calcium supplementation studies have failed to demonstrate any negative effect on iron status (Ilich-Ernst et al. 1998; Kalkwarf & Harrast, 1998; Minihane & FairweatherTait, 1998; Sokoll & Dawson-Hughes, 1992; Yan et al, 1996)