Highlights in Pediatrics Toxicology Dr. Manal Al Maskati Oct, 2011
advertisement

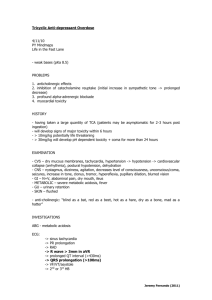
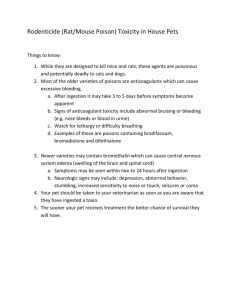
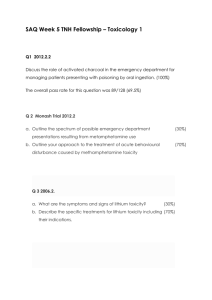
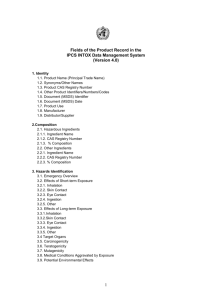
HIGHLIGHTS IN PEDIATRICS TOXICOLOGY Dr. Manal Al Maskati Oct, 2011 - Kuwait OBJECTIVES Few words about poisoning in Pediatrics. Key points in poisoning history and physical examination. Some important Toxidromes. Common cases of poisoning in Pediatric age group. INTRODUCTION Poisonings too common in pediatric world. Around 6,000,000 children ingest potentially toxic substance each year nationwide. Most frequently in children ages 1-5 years old. Most common exposures are substances found around the house (makeup, household chemicals, over the counter medicines, and houseplants). Substances either nontoxic or, if toxic, in insufficient amounts to cause significant problems. Second peak of exposures in adolescent population, most are suicide attempts. Drug or Poison Potentially Lethal Dose In 10 kg Child Camphor Chloroquine Codeine Desipramine Hydrocarbons (e.g. gasoline) Oral Hypoglycemics 1 teaspoon of 20% oil Imipramine Iron Lindane Methyl Salicylate Theophylline Verapamil 1 tablet (500 mg) 3 tablets (60 mg each) 2 tablets (75 mg each) One swallow (if aspirated) 2 Glyburide tablets (5mg each) 1 tablet (150 mg) 10 tablets (Full Adult Strength) 2 teaspoons Less that 1 teaspoon of Oil of Wintergreen 1 tablet (500 mg) 1 tablet (240 mg) HISTORY Three key questions in all poisoning cases: 1) WHAT substance(s) was ingested? 2) WHEN did the ingestion occur? 3) HOW MUCH was ingested? HISTORY Answers to questions will provide valuable information about: a) Severity of the ingestion. b) Potential benefits/efficacy of GI decontamination. c) Whether or not therapeutic interventions necessary. d) Accurate interpretation of specific drug levels. e) Disposition of the patient. TOXICOLOGIC PHYSICAL EXAMINATION a) Eyes: pupillary size, symmetry and response to light presence of nystagmus (vertical or horizontal). b) Oropharynx: moist or dry mucus membranes, presence/absence of the gag reflex, presence of any particular or distinctive odors. c) Abdomen: presence/absence and quality of bowel sounds. d) Skin: warm/dry, warm/sweaty or cool. e) Neurologic: level of consciousness and mental status, presence of tremors, seizures or other movement disorders, presence/absence and quality of deep tendon reflexes. TOXIDROMES Refer to specific constellation of signs and symptoms specific class or type of toxic substance. 1. Anticholinergics (atropine, antihistamines, cyclic antidepressants): Tachycardia, hypertension, tachypnea (red as a beet). Mydriasis (blind as a bat). Agitation, hallucinations/delirium, seizures, hypoactive bowel sounds( mad as a hatter). Warm/dry skin, dry mouth (hot as a hare ,dry as a bone). TOXIDROMES 2. Sympathomimetics (cocaine, amphetamines, PCP, decongestants, beta-agonists, theophylline): Tachycardia, hypertension, tachypnea. Mydriasis. Agitation, hallucinations, delirium, seizures, hypoactive bowel sounds. Warm/sweaty skin. TOXIDROMES 3.Cholinergics (organophosphate and carbamate insecticides): "D-U-M-B3-E-L-S" Defecation, Urinary incontinence, Miosis. Bradycardia/Bronchospasm/Bronchorrhea. Emesis, Lacrimation, Salivation. TOXIDROMES 4. Opioids (codeine, morphine, meperidine, heroin): Bradycardia, hypotension, bradypnea. Hypothermia, hyporeflexia, pinpoint pupils. 5.Sedative-hypnotics (ethanol, benzodiazepines, barbiturates): Bradycardia, hypotension, bradypnea. Hypothermia, hyporeflexia, miosis. CASE 1 A two year olds brought to the Pediatric Emergency Department by his mother following an ingestion of 20-22 cyproheptadine HCL tablets (4mg Periactin) 1-1.5 hours prior to presentation. According to his mother, the patient was acting "bizarre". VS: BP:130/70 P :160 T :98.4 Skin: Warm, dry, not flushed Neck: Supple Lungs: CTAB Heart: Tachycardic, otherwise WNL Abdomen: soft, NT Neurologic: Delerious. Patient grasping objects on the floor that were not present Unable to recognize mother, gait ataxic. DTR's normal, no focal findings. ANTIHISTAMINE TOXICITY (ANTICHOLINERGIC TOXIDROME) Management ABC's + supportive care. Sedation with benzodiazepines. Give false positive tricyclic immunoassay on urine screen hamper accurate diagnosis. Physostigmine not indicated unless patient's condition deteriorated. If hemodynamically stable, likely to respond well to sedation. CASE 2 A three year-old male is brought to the Emergency Department in severe respiratory distress. The mother states that she was polishing her dining room table and left to answer the phone. She subsequently found he child several minutes later drenched in the furniture polish solution. The child was noted to be coughing violently, and was anxious and irritable. VS: BP :100/60 P :120 RR :30 T :101.2 rectally. Gen: Anxious, dyspneic, crying infant, coughing violently. Mild cyanosis noted during coughing episodes. Use of accessory muscles and nasal flaring noted. Kerosene-like odor noted on patient's breath. Lungs: Diffuse crackles bilaterally. Heart: Tachycardia. Abd: soft, NT. Neuro: Unable to obtain adequate exam due to poor cooperation HYDROCARBON ASPIRATION Management Most hydrocarbon ingestions of small volume. ABC's to prevent further aspiration, may need intubation for airway protection and /or progressive respiratory distress. Skin decontamination is needed, by removing his clothing and washing with gentle soap and water. Observe for signs of pneumonia , aspiration cause aseptic chemical pneumonitis does not require antibiotics. Secondary bacterial pneumonia may need treatment Prophylactic antibiotics NOT indicated. Steroids also NOT indicated. Supportive treatment with oxygen and bronchodilators to counteract bronchospasm. Common Compounds Risk of Systemic Toxicity Risk of Aspiration Treatment No Systemic Toxicity, High Viscosity (Petrolatum Jelly, motor oil) Low Low None High Observe for pneumonia; do not empty stomach High Observe for pneumonia, Empty stomach if ingestion is > 2 mL/kg No Systemic Toxicity, Low Viscosity (Gasoline, kerosene, mineral seal oil, petroleum ether) Unknown of Uncertain Systemic Toxicity (Turpentine, pine oil) Systemic Toxins (Camphor, phenol, halogenated or aromatic compounds) Low Uncertain High High Observe for pneumonia; perform gastric lavage or give AC CASE 3 A 50 kg 14 year old female is brought to the Emergency Department in a comatose state. History, as obtained from the distraught parents, reveals that their daughter was very upset recently following the termination of her relationship with her closest friend. The child was found in a lethargic state when the parents returned home from the theater. An empty bottle of Darvocet N-100 was found in the bedroom near the patient. The mother confirms that the medication was prescribed by her family physician for back pain, and the prescription for 100 tablets had been filled one week ago. The parents last saw the patient approximately 5 hours ago. VS: BP: 80/40 P: 110 R :8 T :98.6 rectally Gen: Comatose female, responsive only to deep sternal pressure, vomitus on clothing, diaphoretic. HEENT: Pupils equal at 3mm bilaterally, sluggish. Lungs: CTAB Heart: WNL Abdomen: soft, NT Neurologic: Absent DTR's ACETAMINOPHEN TOXICITY OPIOID TOXICITY Darvocet N-100 is a combination analgesic that contains propoxyphene, a synthetic opioid, and 650mg of acetaminophen. Synthetic opioids that do not cause significant miosis (others Demerol and Dextromethorphan) Many of synthetic opioids do not show up on routine urine tox screens. This scenario carries high possibility of additional unknown coingestants ingestions. intentional overdoses often polydrug ACETAMINOPHEN TOXICITY OPIOID TOXICITY Management Close attention to ABC's. Intubation if there risk of aspiration. For opioid toxicity: Naloxone (Narcan) to be given at initial dose of 2mg. Further doses given until adequate effect achieved. Naloxone provide rapid (1-2 minutes) reversal of symptoms. Due to short duration of naloxone action (60 minutes), redosing will likely be necessary ,if opioid symptoms persist. Lack of response to narcan might point to coingestion of another CNS depressant (benzodiazepines or barbiturates). ACETAMINOPHEN TOXICITY OPIOID TOXICITY For acetaminophen toxicity APAP level should be sent. 4 hour post ingestion level key in determining need for treatment. If level is toxic based on nomogram ,treatment with NAC should be initiated. If level is subtoxic, then to be repeated within 4 hours to confirm it . Initial loading dose of NAC within 8 hrs of ingestion, good effect if given within 24 hrs of ingestion. NAC Loading dose 140 mg, followed by 70 mg q4h X 17 doses. CASE 4 A 15 year old female is brought to the Emergency Department in a confused state by her sister. Following an argument, the patient ingested an unknown amount of medication during the early morning hours. Her sister who was, awakened in the morning to find the patient mumbling incoherently. She brought her to the Emergency Department and quickly left. The patient herself can give no additional history. VS: BP:70/50 P:120 R:32 T:102.6 GEN: Disoriented, somewhat restless female HEENT: NCAT, TM's clear bilat., Pt c/o "noise in her ears", PERRLA, Pt. complains of blurred vision. Lungs: Crackles 2/3 of the way up bilat. Heart: Tachycardia, otherwise WNL Abd: 2+ Mid-epigastric tenderness with diminished bowel sound Skin: Warm and moist LAB WORK Sodium: 148 Potassium: 3.2 Chloride: 101 Bicarbonate: 13 ABG on Room Air pH: 7.21 pCO2: 10 pO2: 80 Urinalysis U/O over 1st hour: 5cc Specific Gravity: 1.029 with microscopic hematuria Radiographic Chest X-Ray: Bilateral hilar infiltrates SALICYLATE TOXICITY Elevated anion gap metabolic acidosis (AG=34). A combination of primary AG metabolic acidosis + primary respiratory alkalosis highly suggestive of salicylate poisoning. A serum salicylate level > 60, indicates major exposure. Level > 100, indicates severe poisoning. Mental status + acid/base status more important than serum concentration. Bedside, quick urine test ferric chloride test. Presence of salicylates purple color change. MANAGEMENT ABC's. Activated charcoal should be administered. Bicarbonate, both to correct the acidemia, and alkalinize the urine facilitate excretion of salicylates. Important to maintain serum potassium in normal range hypokalemia hamper efforts to alkalinize the urine. Dialysis to be considered for refractive acidosis or severe hypokelemia. TRICYCLIC ANTIDEPRESSANTS Significant source of poisonings. Toxic effects of TCA’s mediated through anticholinergic, alpha1 blockade, and quinidine-like Na channel blockade effects. TCA’s have low therapeutic to toxic ratio, doses < 10 times therapeutic sufficient to cause toxicity. Symptoms appear rapidly (within 1 hr of ingestion). Asymptomatic person for 6 hrs post ingestion unlikely to develop life-threatening events. Mechanism Cardiovascular Effects Anticholinergic Tachycardia Hypertension Alpha1 Blockade Peripheral Vasodilation Flushing Hypotension (tends to predominate over HTN) Na Channel Blockade Membrane Depression Conduction Disturbances Prolonged PR, QRS Arrhythmias (tachy, VF) CNS Effects Hyperthermia Agitation Delerium Coma Seizures (may be related to serotonin or norepinephrine mediated effects) DIAGNOSIS Urine screens can detect many of TCA’s, but a negative screen doesn’t rule out exposure. ECG key element to diagnose TCA toxicity. QRS prolongation + seizures + lethargy or coma , highly suggestive of TCA poisoning. Degree of QRS prolongation severity of CNS + cardiovascular toxicity. QRS >0.10 associated with seizures and >0.16 associated with arrhythmias. MANAGEMENT ABC’s Activated charcoal. Unlike pure anticholinergic toxicity, physostigmine should NOT be used in TCA overdose worsen seizures + conduction disturbances + increased risk for asystole. Most important therapy for TCA overdose sodium bicarbonate, QRS prolongation or hypotension. Initial dose 1 mEq/kg, repeated as boluses to maintain QRS < 0.10. Asymptomatic pts monitored for at least 6 hours, symptomatics should be admitted to ICU for at least 24 hours. BETA BLOCKERS CALCIUM CHANNEL BLOCKERS Beta Blockers Have negative inotropic + chronotropic effects. In toxic doses, myocardial depressant effects predominate (hypertension, ventricular arrhythmias). Calcium Channel Blockers Have negative inotropic + chronotropic effects , and/or vasodilation, depends on site of action. Site of Action Verapimil Vascular Smooth Muscle + ++ +++ Cardiac +++ ++ + Diltiazem Dihydropyridines MANIFESTATIONS Toxic doses for both classes varies from agent to agent. Both beta blockers and calcium channel blockers have very small therapeutic to toxic ratio. Signs of toxicity Most common features of overdose of both classes hypotension + bradycardia. ECG's show simply sinus bradycardia, with vaiable PR prolongation. Beta blockers blockers not. within therapeutic range. QRS prolongation, but calcium channel MANIFESTATIONS MANAGEMENT ABC’s Activated charcoal . Gastric lavage for significant ingestions( within 1/2 -1 hr of ingestion). Sustained release preparations may need whole bowel irrigation. No place for dialysis. Focused Therapy -- Beta Blockers Glucagon is antidote. Has positive inotropic + chronotropic. Given as bolus followed by continuous infusion. Epinephrine also effective. QRS prolongation treated with sodium bicarbonate. MANAGEMENT Focused Therapy -- Calcium Channel Blockers Calcium is antidote, helps to overcome the blockade of calcium channels. Given either as calcium chloride or calcium gluconate, repeated as needed. Calcium gluconate preferable (tissue damage with calcium chloride) 30 mL of calcium gluconate approximately 1 gram of calcium. Leads to rapid improvement in contractility, but no effect on conduction disturbances, sinus node depression or peripheral vasodilation. Glucagon and epinephrine beneficial in treating severe hypotension and/or bradycardia. TAKE HOME MESSAGE Prevention is always better than treatment. As early as the diagnosis and intervention as better as the results. Detailed history + Thorough examination + Reliable source + Little knowledge about toxicology Successful management.