Acid Base Balance - The Ohio State University College of Veterinary
advertisement
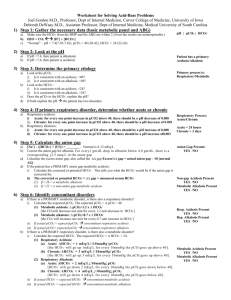
Acid Base Balance • Stephen P. DiBartola, DVM • Department of Veterinary Clinical Sciences • College of Veterinary Medicine • Ohio State University • Columbus, OH 43210 The Nephronauts Acid Base Balance • Who cares about acid base Now that I have this data, what balance? does it mean? Acid Base Balance: Why pH? • Nanoequivalent concentration of H+ versus milliequivalent concentrations of other electrolytes (Na+, K+, Cl-, HCO3-) in body fluids • Normal ECF [H+] is 40 nEq/L or 0.00004 mEq/L versus [K+] of 4.0 mEq/L Acid Base Balance • pH = -log10[H+] = log10(1/[H+]) • [H+] = 40 nEq/L = 4 X 10-8 Eq/L • pH = -log10(4 X 10-8) = 7.4 • Normal pH = 7.37-7.42 and extreme range compatible with life is 6.8 to 8.0 Acid Base Balance • HA = + • Acid = Proton donor (HA) • Base = Proton acceptor (A-) + H A Acid Base Balance: Daily metabolism • Metabolism of sulfur-containing amino acids in proteins yields sulfuric acid and metabolism of phospholipids yields phosphoric acid: 40-80 mEq/day of FIXED or NON-VOLATILE acid • Metabolism of carbohydrates and fats yields 15,000-20,000 mMol CO2 or VOLATILE acid Acid Base Balance • Why is CO2 an acid? (How can it be a proton donor?) • Carbonic anhydrase in red cells and renal tubular cells facilitates the reaction: CO2 + H2O = H2CO3 • Carbonic acid is an obvious proton donor: H2CO3 = H+ + HCO3- Acid Base Balance: Buffers • A substance that can accept protons (H+ ions) and minimize a change in pH • A solution of a weak acid and its salt mEq strong Titration curve of a buffer solution Buffer zone pKa +/- 1.0 pH unit pKa pH Acid Base Balance: Buffers • Effectiveness of a buffer depends upon: • Prevailing pH of body fluid to be defended • Concentration of buffer in that body fluid • pKa of buffer • “Special circumstances” (e.g., bicarbonate is part of an open system) Important body buffers • Extracellular fluid (ECF) • Bicarbonate • Intracellular fluid (ICF) • Phosphates • Proteins (e.g., Hb in RBC) • Bone carbonate Important body buffers: Bicarbonate • pKa is 1.3 units below physiologic pH • ECF concentration is high (24 mEq/L) • In equilibrium with CO2 (i.e. part of an open system) CO2 + H2O = H2CO3 = H+ + HCO3- Important body buffers: Phosphate • Important in ICF where concentration is high (40 mEq/L) • Relatively unimportant in ECF where concentration is low (2 mEq/L) • Important in urine (titratable acidity) due to pKa of 6.8 (distal tubular fluid pH = 6.0 to 7.0) Important body buffers: Proteins • Plasma proteins play limited role in ECF buffering • Intracellular proteins (especially Hb in RBC) play major role in buffering Important body buffers: Bone carbonate • Very large store of potential buffer • Important role in long term response to chronic acidosis Henderson-Hasselbach equation • • • • • HA H+ + A- (v1 = k1[HA]) H+ + A- HA (v2 = k2[H+][A-]) At equilibrium: v1 = v2 k1[HA] = k2[H+][A-] k1/k2 = Ka = [H+][A-]/[HA] Henderson-Hasselbach equation • Ka = [H+][A-]/[HA] • pH = pKa + log([A-]/[HA]) Henderson-Hasselbach equation • pH = pKa + log([HCO3-]/[H2CO3]) • CO2 dissolved in plasma potentially can form H2CO3 so: pH = pKa + log([HCO3-]/[dissolved CO2 + H2CO3]) Henderson-Hasselbach equation • At the temperature and ionic strength of ECF there are 6,800 HCO3- ions and 340 molecules of dissolved CO2 for each molecule of H2CO3. Therefore, H2CO3 can be neglected. • Dissolved CO2 is related to pCO2 by its solubility coefficient: Dissolved CO2 = 0.03 X pCO2 Henderson-Hasselbach equation (clinically relevant form) • pH = pKa + log([HCO3-]/.03xpCO2) • pH = 6.1 + log([HCO3-]/.03xpCO2) • Shows that pH is a function of the RATIO between bicarbonate and pCO2 Acid Base Balance: Physiologic lines of defense • Physicochemical buffering by ECF and ICF buffers (seconds) • Alterations in ventilation to produce a change in pCO2 (seconds to minutes) • Renal readjustment of body HCO3stores (hours to days) • pH = pKa + log(KIDNEYS/LUNGS) Primary Acid Base Disorders • Metabolic disturbances • Metabolic acidosis • Metabolic alkalosis • Respiratory disturbances • Respiratory acidosis • Respiratory alkalosis Acid Base Disorders Acidosis and alkalosis versus Acidemia and alkalemia Acid Base Disorders: Principles of interpretation • Each primary (metabolic or respiratory) disturbance is accompanied by a secondary (opposing) response in the other system (respiratory or metabolic) • pH is returned nearly but not completely to normal • Overcompensation does not occur Acid Base Disorders Disorder Metabolic acidosis Metabolic alkalosis Respiratory acidosis Respiratory alkalosis pH [H+] Primary Secondary disturbance response [HCO3-] pCO2 [HCO3-] pCO2 pCO2 [HCO3-] pCO2 [HCO3-] Acid Base Disorders • Simple Primary disturbance and expected adaptive (secondary) response • Mixed Two separate primary disturbances present simultaneously in the same individual Must know expected adaptive (compensatory) response to recognize mixed disturbances Acid Base Disorders Primary disorder Compensatory response Metabolic acidosis 0.7-1.2 mm pCO2 per 1.0 mEq/L HCO3- Metabolic alkalosis 0.7 mm pCO2 per 1.0 mEq/L HCO3- Acute respiratory acidosis 0.15 mEq/L HCO3- per 1.0 mm pCO2 Chronic respiratory acidosis 0.35 mEq/L HCO3- per 1.0 mm pCO2 Acute respiratory alkalosis 0.25 mEq/L HCO3- per 1.0 mm pCO2 Chronic respiratory alkalosis 0.55 mEq/L HCO3- per 1.0 mm pCO2 Compensation for metabolic acidosis • H+ buffered by ECF HCO3- & Hb in RBC; Plasma Pr and Pi: negligible role (sec-min) • Ventilation lowers pCO2 (min) • H+ buffered by interstitial HCO3- (30 min) • H+ buffered by ICF Pr and Pi (hrs) • Renal regeneration of HCO3(2-6 days) Compensation for metabolic acidosis • H+ buffered by ECF HCO3& Hb in RBC; Plasma Pr and Pi: negligible role (sec-min) • Ventilation lowers pCO2 (min) • H+ buffered by interstitial HCO3- (30 min) • H+ buffered by ICF Pr and Pi (hrs) • Renal regeneration of HCO3- (2-6 days) Compensation for respiratory acidosis Bicarbonate cannot participate in buffering of H+ arising from respiratory acidosis: CO2 + H2O = H2CO3 = H+ + HCO3- From respiratory acidosis Compensation for respiratory acidosis • Bicarbonate is formed as the CO2 + H2O = H2CO3 = H+ + HCO3- equilibrium is pushed to the right • H+ formed is buffered by Hb in RBC (seconds to minutes) • H+ enters other cells and is buffered by proteins and phosphates (hours) • Renal excretion of H+ and generation of new bicarbonate follows (2 to 6 days) Compensation for acid base disturbances • Respiratory compensation for metabolic disorders should be complete in 24 hours • “Acute” is < 24-48 hrs • “Chronic” is > 24-48 hrs • Metabolic (renal) compensation for respiratory disorders is slower and requires 2 to 6 days Concept of Anion Gap Acid Base Disorders: Interpretation • Is an acid base disturbance present? • What is the primary disturbance? • Is the secondary (adaptive) response as expected? • What underlying disease process is responsible for the acid base disturbance? Acid Base Disorders: Interpretation • Arterial blood gas from a dog: pH 7.27, HCO312 mEq/L, pCO2 27 mmHg (normal: pH 7.39, HCO3- 22 mEq/L, pCO2 37 mmHg) • Is an acid base disturbance present? • YES (look at the pH) • Of what general type? • ACIDOSIS (pH 7.27 < 7.39) • Metabolic or respiratory? • pCO2 is LOW (can’t be respiratory acidosis) • HCO3- is LOW (must be METABOLIC ACIDOSIS) Acid Base Disorders: Interpretation • Is secondary (adaptive) response as expected? • Observed HCO3- is 10 mEq/L lower than “normal” (22-12) • “Normal” dog can lower pCO2 1 mmHg for every 0.7-1.2 mEq/L decrement in HCO3- (use 1.0 mEq/L as “average”) • Expected pCO2 = 37-10 = 27 mmHg • Observed pCO2 = 27 mmHg • Conclusion: YES, adaptive response is as expected. This is a simple metabolic acidosis with respiratory compensation Acid Base Disorders: Interpretation • Arterial blood gas from a dog sick for 1 week: pH 7.33, HCO3- 29 mEq/L, pCO2 57 mmHg (normal: pH 7.39, HCO3- 22 mEq/L, pCO2 37 mmHg) • Is an acid base disturbance present? • YES (look at the pH) • Of what general type? • ACIDOSIS (pH 7.33 < 7.39) • Metabolic or respiratory? • HCO3- is HIGH (can’t be metabolic acidosis) • pCO2 is HIGH (must be RESPIRATORY ACIDOSIS) Acid Base Disorders: Interpretation • Is secondary (adaptive) response as expected? • Observed pCO2 is 20 mmHg higher than “normal” (57-37) • “Normal” dog can increase HCO3- 3.5 mEq/L for every 10 mmHg increment in pCO2 (in “chronic” disturbance) • Expected HCO3- = 22+7 = 29 mEq/L • Observed HCO3- = 29 mEq/L • Conclusion: YES, adaptive response is as expected. This is a simple respiratory acidosis with metabolic compensation Acid Base Disorders: Interpretation • Even in simple disturbances, calculated compensatory pCO2 and HCO3- values usually won’t match observed values because calculations are based on “average” values • Do not diagnose a mixed disturbance unless calculated value is > 2 to 3 mmHg (pCO2) or mEq/L (HCO3-) different from observed value Acid Base Disorders: Interpretation • Arterial blood gas from a dog: pH 7.05, HCO312 mEq/L, pCO2 44 mmHg (normal: pH 7.39, HCO3- 22 mEq/L, pCO2 37 mmHg) • Is an acid base disturbance present? • ABSOLUTELY! (look at the pH) • Of what general type? • ACIDOSIS (pH 7.05 << 7.39) • Metabolic or respiratory? • pCO2 is HIGH (could be respiratory acidosis) • HCO3- is LOW (could be metabolic acidosis) Acid Base Disorders: Interpretation • Is secondary (adaptive) response as expected? • NO • If simple metabolic acidosis, pCO2 should be low in response • If simple respiratory acidosis, HCO3- should be high in response • Conclusion: This is a mixed metabolic and respiratory acidosis. The extremely low pH alerts you to the possibility of a mixed disturbance Acid Base Disorders: Interpretation • Arterial blood gas from a dog with sudden onset of gastric dilatation/volvulus: pH 7.38, HCO3- 12 mEq/L, pCO2 21 mmHg (normal: pH 7.39, HCO3- 22 mEq/L, pCO2 37 mmHg) • Is an acid base disturbance present? • If so, it’s not obvious from pH • Of what general type? • From pCO2 could be respiratory alkalosis or from HCO3- could be metabolic acidosis • Metabolic or respiratory? • pCO2 is LOW (could be respiratory alkalosis) • HCO3- is LOW (could be metabolic acidosis) Acid Base Disorders: Interpretation • Is secondary (adaptive) response as expected? • If primary metabolic acidosis • 10 mEq/L decrement in HCO3- (22-12) • Expected pCO2 = 27 mmHg (37-10) • Observed pCO2 = 21 mmHg • If primary acute respiratory alkalosis • 16 mmHg decrement in pCO2 (37-21) • Expected HCO3- = 18 mEq/L (22-4) • Observed HCO3- = 12 mEq/L • Conclusion: Mixed metabolic acidosis and respiratory alkalosis Acid Base Disorders: Interpretation • Is mixed metabolic acidosis and respiratory alkalosis compatible with acute gastric dilatation/volvulus? • YES • Metabolic acidosis due to shock and decreased tissue perfusion • Respiratory alkalosis due to hyperventilation induced by pain or septicemia Acid Base Disorders: Interpretation • What if dog had been sick with some other disorder for 1 week? • If primary chronic respiratory alkalosis • 16 mmHg decrement in pCO2 (37-21) • Expected HCO3- = 13.2 mEq/L (22-8.8) • Observed HCO3- = 12 mEq/L • Difference is < 2 mEq/L • Conclusion of simple chronic respiratory alkalosis would be justified Renal regulation of acid base balance • Role of kidneys is preservation of body’s bicarbonate stores. Accomplished by: • Reabsorption of 99.9% of filtered bicarbonate • Regeneration of titrated bicarbonate by excretion of: • Titratable acidity (mainly phosphate) • Ammonium salts All of these things are accomplished by secretion of hydrogen ions All of these things are accomplished by secretion of hydrogen ions … • If secreted H+ ions combine with filtered bicarbonate, bicarbonate is reabsorbed • If secreted H+ ions combine with phosphate or ammonia, net acid excretion and generation of new bicarbonate occur It all depends on what buffer the secreted H+ encounters in the tubular fluid, which in turn is a function of where we are in the nephron! Renal reabsorption of bicarbonate • Proximal tubule: 70-85% • Loop of Henle: 10-20% • Distal tubule and collecting ducts: 4-7% Factors affecting renal bicarbonate reabsorption • • • • Filtered load of bicarbonate Extracellular fluid volume Prolonged changes in pCO2 Plasma chloride concentration • Plasma potassium concentration • Hormones (e.g., mineralocorticoids, glucocorticoids) Titratable acidity • Occurs when secreted H+ encounter & titrate phosphate in tubular fluid • Refers to amount of strong base needed to titrate urine back to pH 7.4 • 40% (15-30 mEq) of daily fixed acid load • Relatively constant (not highly adaptable) Ammonium excretion • Occurs when secreted H+ combine with NH3 and are trapped as NH4+ salts in tubular fluid • 60% (25-50 mEq) of daily fixed acid load • Very adaptable (via glutaminase induction) Ammonium excretion • Large amounts of H+ can be excreted without extremely low urine pH because pKa of NH3/NH4+ system is very high (9.2)