Presentation Handout
advertisement

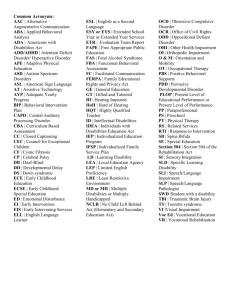
Overview of Dementia, Depression and Schizophrenia in the Elderly Peter Betz, M.D. Hierarchical Levels of Human Mental Life Components of Psychological Life Modes of Mental Disorder Treatment Initiatives Personal Chronicle Disruptive Life Stories Rescript Constitutional Dimensions Problematic Dispositions Guide Motivational Rhythms Behavior Disorders Interrupt Cerebral Faculties Psychiatric Diseases Remedy McHugh and Slavney Dementia is now ‘Neurocognitive Disorder’ (NCD) Further Defined as ‘Major’ or ‘Minor’ What’s in a name? Greater phenomenological correctness – especially with the growing base of literature defining specific aetiologies Broader term - can include syndromes with only one cognitive domain affected (e.g. ‘amnestic d/o’) NCD is often the preferred term in the literature and in practice – such as in younger individuals or those with TBI Dementia is ok to still use if it helps communicate the nature of the illness Neurocognitive Disorder Major Minor Concern of the individual, informant or clinician Concern of the individual, informant or clinician ‘significant’ cognitive decline – needs IADL assistance ‘modest’ cognitive decline – preserved IADLs but needs compensatory strategies or accommodation Not due to delirium or another mental disorder Not due to delirium or another mental disorder Alzheimer Disease Insidious onset and gradual progression without plateaus Impairment in Memory/Learning and one other area No mixed etiologies Probable – all 3 331.0 + 294.10 or 294.11 Possible – not all 3 331.9 No coding +/behavioral disturbance Vascular NCD *Onset temporally related to cerebrovascular event(s) -orProminent impairment in complex attention (processing speed) or executive function (planning, organizing, sequencing, abstraction) Hx, PE &/or *Imaging shows evidence of sufficient vascular disease Probable (290.4) if * is present in your decision tree Possible (331.9) if no * No coding +/- behavioral disturbance for either possible or probable NCD with Lewy Bodies Core Features Fluctuating cognition Well defined VH Parkinsonism onset subsequent to cognitive decline Suggestive Features REM sleep disorder Severe neuroleptic sensitivity Probable 2+ bullets including at least one core feature 331.82 + 294.10/294.11 Possible 1 bullet 331.82 No coding +/behavioral disturbance Frontotemporal NCD Behavioral Variant 3 or more bullets: Behavioral disinhibition Apathy or inertia Loss of sympathy or empathy Perseverative, stereotyped or compulsive/ritualistic behavior Hyperorality and dietary changes Relative sparing of learning /memory and perceptualmotor function Language Variant Prominent decline in one: Form of speech production Word finding Object naming Grammar Word comprehension Relative sparing of learning /memory and perceptualmotor function Frontotemporal NCD Probable Evidence of disproportionate frontal &/or temporal involvement 331.19 + 294.10/294.11 Possible 331.9 No coding +/- behavioral disturbance Common Complications of AD Anosognosia (50%) e.g. unawareness of illness, not “psychological” denial Apathy (25-50%) inanition, poor persistence Psychosis delusions (20%), hallucinations(15%) Mood Disorders depression (20%), anxiety (15%) Agitation / Aggression (50-60%) wandering, restlessness, verbal and physical attacking Sundowning (25%) Textbook of Alzheimer Disease and Other Dementias, Weiner & Lipton, 2009 Interventions - Medication Cholinesterase Inhibitors tacrine, donepezil, rivastigmine, galantamine Memantine Vitamin E Monoamine Oxidase Inhibitor selegeline Ginko Biloba Anti-Inflamatory Agents Estrogen Replacement Therapy Lipid Lowering Agents ‘Non-Medicinal’ Interventions Education, support, counseling, community resources for the patient AND the caregiver Long-Term Planning state and private resources will durable power of attorney advance directive ‘Non-Medicinal’ Interventions Environmental / Home Safety remove dangerous objects Medications, clutter beware: water temperature, stairs, sharp furniture, glassware, windows, locks, kitchen equipment assess activities of daily living institutionalization driving FDA Approved Treatments for Complications of AD Behavioral Management Environmental vs. Medication meds are a last resort The “4D Approach” adapted from Practical Dementia Care by Rabins, Lyketsos, and Steele Our Assumptions: Behavioral dyscontrol can have multiple etiologies. They can be distinguished from each other. Identifying the cause can directly lead to treatment strategies. There is rarely “one-best” approach to address these issues. Directed “trial and error” is the rule, not the exception. The “4D Approach” Define and Describe Decode Devise a treatment plan Determine “does it work?” Behavioral Management Environmental vs. Medication meds are a last resort If you chose a medication… Which One? antipsychotics typical vs. atypical benzodiazepine other e.g valproate CATIE-AD Lon S. Schneider et. Al. Primary outcome – time to discontinuation for any reason great “real world” approach to study design Atypicals were no better “tolerated” Big media spin after data released: Known higher mortality per FDA. Now evidence of “lack of efficacy.” Therefore, doctors are abusing elderly patients. Actually, study shows: Placebo stopped more due the lack of benefit than S.E. Atypicals stopped more due to S.E. than lack of benefit. What you (and your patients) should watch for: EPS Torsades de pointes Dystonia Postural hypotension Akathisia Weight gain NMS Agranulocytosis TD Glucose Dyscontrol Cholesterol Dyscontrol Delirium Increased risk of all cause death What About Anticonvulsants? Initial trials were promising, but… Most recent studies show far less benefit if not more behavioral discontrol However, can be helpful in some augmenting strategies or in catastrophic reactions. What NOT To Use Benzodiazepine Side Effects Sedation Deliriogenic Behavioral disinhibition Emotional lability Cognitive impairment – particularly amnesia Ataxia Respiratory depression Rebound insomnia and anxiety Withdrawal / Physiologic dependence Major Depression DSM-5 – 5 of 9 *Depressed mood (reported or observed) *Markedly diminished interest /pleasure >5% weight loss or gain Insomnia or hypersomnia Psychomotor slowing or agitation (observable) Fatigue or loss of energy Worthlessness or inappropriate guilt (not of being sick) Poor concentration Recurrent thoughts of death Betz – 2 of 3 Dysphoric change in mood sadness, irritability, no ‘yeah’ Impaired self-attitude low self-esteem, worthlessness, guilt, etc. Neurovegitative symptom impairment eating, sleeping, energy, conc., sex drive, etc. Dysthymia (>2 years) DSM – 5 Depression 2 of 6 Poor appetite or overeating Insomnia or hypersomnia Low energy or fatigue Low self-esteem Poor concentration or difficulty making decisions Feelings of hopelessness Betz – 2 of 3 Dysphoric change in mood sadness, irritability, no ‘yeah’ Impaired self-attitude low self-esteem, worthlessness, guilt, etc. Neurovegitative symptom impairment eating, sleeping, energy, conc., sex drive, etc. Premenstrual Dysphoric Disorder 5 of 9 symptoms present in week before menses Improves within a few days of onset of menses Absent (or minimal) the week post menses At least one: Affective liability Depressed mood, hopelessness Anxiety, tension At least one: Apathy Poor concentration Anergia, lethargy Sense of being overwhelmed Physical symptoms (e.g. bloating, breast tenderness, joint pain etc.) My Most Worrisome Issues Hopelessness Suicide NIMH 18% of total in those ≥ 65yo (only 13% of pop) 6x higher risk if ≥ 80yo suicidal thoughts in 7% of elderly suicidal thoughts in 30% of elderly with MDD 20% saw physician within 24 hours 41% saw physician within 1 week 75% saw physician within 1 month Acute Management: Antidepressant + psychotherapy Alternate: Mild – meds alone or psychotherapy alone Severe – meds alone or ECT What Antidepressants? SSRI escitalopram, citalopram, sertraline (avoid paroxetine, fluoxetine, fluvoxamine) SNRI venlafaxine, duloxetine buproprion mirtazapine TCA NTP, protriptyline, desipramine (avoid others such as amytriptyline) What NOT To Use ECT Psychosocial Interventions Psychotherapy supportive, cog-behav, problem solving, interpersonal Education Family Counseling Visiting nurse to help with meds Bereavement groups Senior citizen center Schizophrenia 1 Month: Two or More (has to include 1 of first 3): Delusions Hallucinations Thought Disorder Catatonia Negative Symptoms Ambivalence, Autism, Affect, Associations Functional Impairment Continued disturbance for 6 months may be just negative symptoms No longer has subtypes (except w or w/o catatonia) Psychosocial Interventions Psychotherapy supportive, cog-behav, problem solving, interpersonal Education Family Counseling Visiting nurse to help with meds Bereavement groups Senior citizen center Lets Define the Atypicals Atypical: “Deviating from what is usual or common or to be expected” – Websters So, what are Typical Antipsychotics? Drugs that had high probability of inducing Extrapyramidal Side Effects (EPS) EPS ≡ Parkinsonism via high D2 antagonism High Potency vs. Low Potency EPS generally mitigated by anticholinergic activity exception is risperidone which uses 5HT2 antagonism Examples: high: haloperidol, fluphenazine, droperidol, pimozide low: chlorpromazine, thioridazine, Lets Define the Atypicals – not a class created of equals Clozapine (Clazaril) Aripiprazole (Abilify) Risperidone (Risperdal) Paliperidone (Invega) Olanzapine (Zyprexa) Asenapine (Saphris) Quetiapine (Seroquel) Iloperidone (Fanapt) Ziprasidone (Geodon) Lurasidone (Latuda) Clinical Recepterology Receptor we antagonize: What we watch for: D2 EPS, (+) symptom relief, hyperprolactinemia 5-HT2a (-) symptom relief, mitigates EPS 5-HT2c Antidepression α1 Postural hypotension H1 Weight gain, sedation M1 Weight gain, sedation, urinary retention, confusion, constipation, dry mouth etc… Dissociation Constants Drug D1 D2 D3 D4 5-HT2a 5-HT2c α1 H1 ACh Haloperidol 210 1 2 3 45 >10,000 6 440 5,500 Clozapine 85 160 170 50 16 10 7 1 2 Olanzapine 31 44 50 50 5 11 19 3 2 Quetiapine 460 580 940 1,900 300 5,100 7 11 >1,000 Risperidone 430 2 10 10 0.5 25 1 20 >1,000 Ziprasidone 525 4 7 32 0.4 1 10 50 >1,000 Aripiprazole 410 0.52 7.2 260 20 15 57 61 >1,000 Asenapine 1.4 1.3 0.42 1.1 0.06 0.03 1.2 1.0 8128 Iloperidone 216 6.3 7.1 5.6 42.8 36 473 >1000 Lurasidone 262 0.99 15.7 29.2 0.47 262 >1000 >1000 25