Respiratory Bronchioles
advertisement

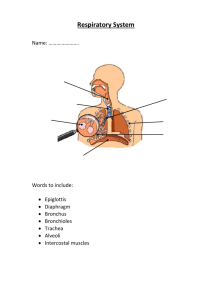
Histology of the Respiratory system By Safaa El Bialy (MD, PhD) Objectives • • • • • • Describe the histology of the respiratory epithelium, and demonstrate the ability to identify the different tissue layers making up the respiratory tract (i.e., mucosa, submucosa, cartilage layer and adventitia). Recognize the concept of the mucociliary blanket. Describe the structure of the alveoli Explain how the alveoli allow for gas exchange. Identify the components of the trachea, bronchi and bronchioles. Compare and contrast the conducting portion and the respiratory portion of the respiratory system. Respiratory system • • 1. 2. 3. • 1. 2. 3. 4. 5. Anatomically Consists of : Upper respiratory system Nasal cavities Sinuses Nasopharynx Lower respiratory system Larynx Trachea Bronchi Bronchioles and alveoli Respiratory system • 1. 2. 3. 4. 5. • • • Conducting portion: Nasal cavities Nasopharynx Larynx Trachea, bronchi Bronchioles and terminal bronchioles Function: Provide a conduit through which air moves to and from the lungs Condition the inspired air Respiratory portion 1. Respiratory bronchioles 2. Alveolar ducts 3. Alveoli Function : gas exchange Respiratory Epithelium 1. Most of the conducting system is lined with ciliated C pseudostratified columnar epithelium 2. Goblet cells G are also abundant in some areas (mucin secretion) 3. Brush cells B less abundant considered to be chemosensory receptors 4. Basal cells, small rounded cells on the BM, stem cells that give rise to other type of cells Respiratory Epithelium (brush cells) Respiratory Epithelium (basal cells) Trachea • • • • • • 14-16 cm long tube Extends from larynx (6th cervical vertebra) to carina (bifurcation) in front of sternal angle Lined with typical respiratory mucosa Numerous seromucous glands produce watery mucus In the submucosa, 16-20 C shaped rings of hyaline cartilage keep the trachea open The opened part is dorsal and bridged by trachealis muscle (smooth) and a sheet of fibroelastic tissue Trachea • Entire organ is surrounded by an adventitia Cartilage Submucosa Adventitia Trachealis muscle Trachea 1. Mucosa: Typical respiratory epithelium (E) 2. Submucosa: • Connective tissue (CT) • and seromucous glands (G). 3. Cartilage • C shaped rings Hayline cartilage (C) • perichondrium (P) 4. Adventitia Cartilage Submucosal mixed glands Cartilage Perichondrium Chondrocytes Extracellular matrix Bronchial Tree • • The trachea → 2 primary bronchi → 3 secondary lobar bronchi in the right lung and 2 in the left lung (same histology of the trachea) These Lobar bronchi → tertiary (segmental) bronchi → conducting bronchioles→ terminal bronchioles → respiratory bronchioles Bronchi • • • • Most cartilage rings completely encircles the lumen in 1ry bronchi The rings are gradually replaced with isolated plates of hyaline cartilage Abundant mucus and serous glands Smooth muscles in the lamina propria become more abundant in the smaller bronchioles Tertiary bronchus Histology of Bronchi versus Trachea • Mucosa of larger bronchi structurally similar to mucosa of trachea except for the cartilage & smooth muscle • Cartilage rings completely encircle the lumen of primary bronchi but as bronchial diameter decreases cartilage rings replaced by isolated pieces of hyaline cartilage • Bronchial lamina propria has spirally arranged smooth muscle which becomes more prominent in smaller bronchioles. Large bronchus smaller bronchus Bronchioles • • • • • No cartilage nor glands Ciliated pseudostratified columnar epithelium in larger bronchioles Ciliated simple columnar or cuboidal epithelium in the smaller terminal bronchioles (Clara cells) Lamina propria (smooth muscles and elastic fibers) Musculature of bronchi and bronchioles is under influence of vagus nerve (constricts) and SN system (dilates) A large bronchiole • • • • characteristically folded respiratory epithelium The lamina propria has become a thin band No glands The muscularis, which appears as discontinuous bundles of smooth muscle, is relatively thick A smaller bronchiole • The epithelium is simple columnar • High elastic content (arrowhead) associated with the muscle. A very small bronchiole • The epithelium (E) is reduced to simple low columnar and the several layers of smooth muscle cells (arrows) comprise a high proportion of the wall. Terminal Bronchioles a) Last part of conducting system before sites of gas exchange • Ciliated cuboidal epithelium (very few) • 1 or 2 layers of smooth muscles b) Clara cells 1. Bulging domes of apical cytoplasm with granules 2. Non ciliated 3. secrete surfactant and have various defensive roles. 4. Produce enzymes that help breakdown of mucus Respiratory Bronchioles • • • • • Transition zone between the conducting and respiratory zone Mucosa is similar to terminal bronchioles The walls are interrupted by the openings to saclike alveoli Epithelium in that region is continuous with the squamous alveolar lining cells More distally the number of the alveoli increases and the distance is reduced Respiratory Bronchioles • Very similar to that of a terminal bronchiole, • It has Clara cells lying almost directly over smooth muscle bundles. • The arrow shows where these Clara cells can be seen most clearly. • The alveoli which form outpocketings from the wall are lined by very squamous cells called alveolar type I cells not identifiable here. • Other alveoli are seen at the right of the field of view. Regular Vs terminal Vs respiratory bronchiole • • • • • Regular bronchiole with ciliated pseudostratified epithelium or ciliated columnar Terminal bronchiole ciliated cuboidal with non-ciliated Clara cells. The arrow is pointing at the last of the ciliated cells of the regular bronchiole. Respiratory bronchiole, marking the beginning of the respiratory portion of the respiratory tree (cuboidal with some Clara cells) The dip in the respiratory bronchiole is an alveolus, one of the air sacs in which gas exchange occurs. Histology of Bronchioles versus Bronchi • • Bronchioles lack cartilage & glands in mucosa Epithelium less complex in bronchioles; change from ( PsCc ) in larger bronchioles , with decrease in height to ciliated simple columnar /cuboidal in terminal bronchioles • Goblet cells disappear in terminal bronchiole • Terminal bronchioles 1. have exocrine bronchiolar cells called Clara cells, 2. serve as a region of transition between conducting & respiratory portions of respiratory system. Medical Application (FYI) • • • The bronchiolar muscle layer is greater than the bronchial one Increased airway resistance in asthma is believed to be due mainly to contraction of bronchiolar smooth muscle layer The increase in bronchiolar diameter in response to stimulation of the epinephrine and other sympathomimetic drugs are frequently used to relax smooth muscle during asthma attacks Mucociliary Escalator (Blanket) • • • • Covers most of the bronchi, bronchioles & nose. Composed of mucous producing goblet cells & ciliated epithelium Cilia beats continuously pushing mucous up & out of the throat Microorganisms are caught in the sticky mucous (blanket) and moved up by the mucociliary escalator Smoking Mucociliary Escalator (Blanket) • Smoking leads to reduction in ciliated cells caused by excessive intake of CO • Results in decreased movement of the mucous layer • Frequently leads to congestion of the smaller airways The respiratory zone 1. Respiratory bronchioles • Serve both as conducting and respiratory portions. The thin-walled alveoli open in their lumen. 2. Alveolar ducts • These have many of the alveoli opening into their lumen and their openings are separated by very small segments or knobs of smooth muscles. 3. Alveolar sacs • Each has many alveoli opening into its lumen & without any wall and muscles between their openings. 4. Alveoli • These are thin walled sacs, whose surfaces are sites of gas exchange . Alveolar Ducts • • • • Alveolar ducts AD and sacs AS are lined by attenuated squamous alveolar cells Sparse strands of smooth muscle are present in alveolar duct absent in alveolar sac & alveoli (A) Elastic & Reticular fibres, form a network encircling openings of alveolar sacs & alveoli Reticular fibres ; provide support & prevent over distension & damage to delicate capillaries & thin alveolar septa Alveoli • Sac like evaginations (honeycomb) • Walls are specialized to enhance diffusion between the external and internal environment • interalveolar septum is present between alveoli • Blood air barrier (respiratory membrane): 1. Alveolar cells 2. Endothelial cells 3. Fused basal laminae of alveolar cells and capillary endothelial cells Alveoli Alveolar sac Alveolus Alveoli Smooth muscles Alveolar Septa Type I alveolar cells (type I pneumocytes) • Squamous cells lining 97% of the alveolar surface • Function is to provide a barrier of large surface area and minimal thickness for efficient gas exchange between alveolar air and capillary blood. Type II alveolar cells (type II pneumocytes) • Interspersed between type I cells • Found where the alveolar walls unite • Contain lamellar bodies(secrete surfactant) • Type II pneumocytes also mitotically divide and differentiate into type I pneumocytes in response to injury Endothelial cells of capillaries Interstitial cells • Fibrobalsts 1. Produce collagen, elastin and PGs 2. Repair and remodelling Alveolar macrophages Interalveolar Septum Alveolar space Alveolar septum Capillary Pneumocyte I Pneumocyte II Alveolar Macrophages • • • • Dust cells Found in alveoli and interalveolar septum Slightly darker in the lungs due to their content of dust and carbon Filled macrophages migrate into bronchioles for removal in the pharynx or exit the lungs in the lymphatic drainage macrophage Medical application (FYI) • In CHF, the lungs become congested with blood, and erythrocytes pass in alveoli to be phagocytosed by macrophages • These macrophages are called heart failure cells • Identified by a positive histochemical reaction from iron pigment (hemosiderin) • Increased production of collagen is common and many diseases leading to respiratory distress are known to be associated with lung fibrosis Medical Application (FYI) • • • • • Pulmonary stress syndrome Deficiency of surfactant in the premature babies With surfactant alveoli need less inspiratory force to inflate Life threatening condition Alveoli are collapsed and respiratory bronchioles and alveolar ducts are dilated with edema fluid Medical Application (FYI) • • • • Emphysema Chronic lung disease Destruction of the interalveolar wall Enlargement of the air space distal to the bronchioles • Gradual and results in insufficiency • Cigarette smoking is a major cause Regeneration of the alveolar lining • • • Toxic gases can kill type I and II cells lining pulmonary alveoli Death of type I cells increases the mitotic activity in the remaining type II cells. The progeny of Type II cells become both cell types Summary Cartilage • Trachea C rings of cartilage: Primary & Secondary bronchi: cartilage completely encircle the lumen • Tertiary (segmental ) bronchi : isolated pieces of hyaline cartilage • Bronchioles: cartilage absent Epithelium 1. • 2. • Trachea to Bronchioles : Pseudostratified columnar ciliated with goblet cells. Terminal Bronchioles: Decrease in complexity of epithelium: simple columnar or cuboidal + ciliated.+ clara cells • No sero-mucinous glands & goblet cells disappear 3. Respiratory Bronchioles : • Cuboidal , simple & non ciliated (Clara cells). Cartilage absent Summary Histology Respiratory System • Smooth muscle: Trachea C shaped ring of cartilage bridged by trachealis muscle • Bronchi & bronchioles (terminal & respiratory) contain spiral bands of smooth muscle • Elastic Fibres: Abundant through all levels of respiratory system