2nd respiratory ppt
advertisement

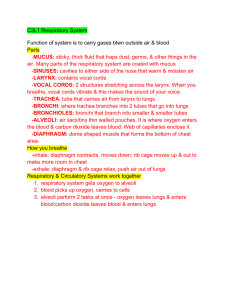
Respiratory System Respiratory zone ◦ Site of gas exchange ◦ Consists of bronchioles, alveolar ducts, and alveoli Conducting zone ◦ Provides rigid conduits for air to reach the sites of gas exchange ◦ Includes all other respiratory structures (e.g., nose, nasal cavity, pharynx, trachea) Respiratory muscles o diaphragm and other muscles that promote ventilation Quiz Picture p. 701 Figure 22.1 ◦ Pulmonary ventilation – moving air into and out of the lungs (breathing) ◦ External respiration – gas exchange between the lungs and the blood ◦ Transport of respiratory gases – Oxygen and Carbon dioxide transport in blood ◦ Internal respiration – gas exchange between systemic blood vessels and tissues ◦ Providing an airway for respiration ◦ Moistening & warming incoming air ◦ Filtering inspired air ◦ Resonating chamber for speech ◦ Contains olfactory receptors Quiz Picture 1. 2. Nasal cavity Mucous membranes ◦ Olfactory Mucosa◦ lines superior region of nose (olfactory receptors=smell) goblet cells, mucous and serous glands Secrete 1 qt mucus/day Respiratory Mucosa- ciliated pseudostratified columnar epithelial Lysozyme – antibacterial enzyme Traps foreign debris and cilia moves to throat Mucosa-Have rich vascular supply-warm air Conchae- makes air turbulent- increases mucosal surface area Rhinitis inflammation of nasal mucosa - Mucus build up, stuffy nose Surround nasal cavity Lighten the skull and help to warm and moisten the air Mucus drains into nasal cavity Sinusitis inflammation of sinus mucosa, infection of mucus in sinus -Swelling prevents movement of mucus out of sinuses = pressure -Sinus headache Quiz Picture p. 702 Figure 22.2b Connects nasal cavity to larynx and esophagus Throat (5”) Skeletal muscle 3 regions ◦ Nasopharynx – Air only Goblet cells produce mucus Swallowing- uvula closes off nasopharynx Contains pharyngeal tonsils ◦ Oropharynx – Food and Air Continuous with nasopharynx Contains palatine and lingual tonsils ◦ Laryngopharynx – Air and Food During swallowing food has priority Voice Box Superiorly attaches to hyoid bone, inferiorly with trachea Functions: ◦ To provide an opening from pharynx to trachea ◦ To act as a switching mechanism to route air and food into the proper channels ◦ To make sound Cartilages (hyaline) of the larynx ◦ Thyroid cartilage with a midline laryngeal prominence (Adam’s apple) ◦ Cricoid cartilage- below thyroid cartilage Epiglottis – elastic cartilage (valve) that covers the entrance to larynx during swallowing Glottis-opening between vocal cords ◦ Normally open-closed swallowing True Vocal Cord- sound production – elastic fibers False Vocal Cords- Closed when swallowing Figure 21.4a, b Speech – intermittent release of expired air while opening and closing the glottis Pitch – determined by the length and tension of the vocal cords Loudness – depends upon the force at which the air rushes across the vocal cords The pharynx resonates, amplifies, and enhances sound quality Sound is “shaped” into language by action of the pharynx, tongue, soft palate, and lips Figure 21.5 Laryngitis inflammation of vocal cords -Swelling prevents movement -Overuse, dry air, bacteria, pollutants Flexible and mobile tube Larynx to the primary bronchi Composed of three layers ◦ Mucosa – made up of goblet cells and ciliated epithelium –smoking destroys cilia ◦ Submucosa – connective tissue deep to the mucosa ◦ Adventitia – outermost layer made of C-shaped rings of hyaline cartilage- keeps open during inspiration Figure 22.6a Right and left primary bronchi-formed by division of trachea Air reaching the bronchi is: ◦ Warm and cleansed of impurities ◦ Saturated with water vapor Bronchi subdivide into secondary bronchi, each supplying a lobe of the lungs Air passages undergo 23 orders of branching in the lungs Tissue walls of bronchi mimic that of the trachea As conducting tubes become smaller, structural changes occur ◦ Cartilage support structures change ◦ Epithelium types change ◦ Amount of smooth muscle increases Bronchioles ◦ Consist of cuboidal epithelium ◦ Have a complete layer of circular smooth muscle ◦ Lack cartilage support and mucus-producing cells Presence of alveoli; begins as terminal bronchioles feed into respiratory bronchioles Respiratory bronchioles lead to alveolar ducts, then to terminal clusters of alveolar sacs composed of alveoli Approximately 300 million alveoli: ◦ Account for most of the lungs’ volume ◦ Provide tremendous surface area for gas exchange Figure 22.8a Figure 22.9b Type I cells -simple squamous epithelium, simple diffusion Dust cells – alveolar macrophages Type II cells – secrete surfactant ◦ Reduces alveolar surface tension ◦ Coats membrane 1. Alveoli 2. Alveolar sac 3. Simple squamous epithelium 4. Blood vessel Figure 22.9.c, d Surface tension – the attraction of liquid molecules to one another at a liquid-gas interface The liquid coating the alveolar surface is always acting to reduce the alveoli to the smallest possible size Detergent –like lipoprotein Breaks up water molecules Increases surface area of alveoli Left lung – separated into upper and lower lobes by the oblique fissure Right lung – separated into three lobes by the oblique and horizontal fissures ◦ Apex – under clavicle ◦ Base – rests on the diaphragm ◦ Hilum – medial surface of each lung-entrance /exit point Pulmonary arteries and veins – supply systemic venous blood to be oxygenated and then back to heart Bronchial arteries – nourish lungs ◦ Arise from aorta ◦ Supply all lung tissue except the alveoli Bronchial veins – drain lungs Pleura - Thin, double-layered serosa ◦ Visceral pleura – inner membrane Covers external lung surface ◦ Parietal pleura – outer membrane Covers the thoracic wall and superior face of the diaphragm Continues around heart and between lungs Pleura Fluid -serous fluid (lubrication) Pleural cavity Pleurisy Inflammation of pleural membranes Friction and sticking of membranes Feels like heart attack ◦ Inspiration – air flows into the lungs ◦ Expiration – air leaves lungs Boyle’s Law Large Volume Small Volume High Pressure Low Pressure = Change in Pressure = Gas Flow to Equalize the Pressure Atmospheric – exerted by air surrounding the body ◦ Sea level 760 mm Hg Intrapulmonary – within alveoli ◦ Equalized with atmospheric pressure Intrapleural - in pleural cavity ◦ Negative ◦ Less than intrapulmonary pressure-keeps lungs expanded Intrapulmonary pressure > Intrapleural pressure Atmospheric pressure > Intrapleural Pressure Causes adhesion of pleural membranes Homeostatic Imbalance Intrapleural pressure > Intrapulmonary pressure Pneumothorax◦ ◦ ◦ ◦ Knife wound, gun shot Air moves into pleural cavity May affect only one lung Treatment: Close hole and draw air out. 1. 2. 3. 4. Diaphragm and external intercostal muscles (inspiratory muscles) contract = Rib cage rises Lungs are stretched and intrapulmonary Volume increases Intrapulmonary pressure decreases below atmospheric pressure (1 mm Hg) Air flows in the lungs, down its pressure gradient, until intrapleural pressure = atmospheric pressure Inspiratory muscles relax and the rib cage descends due to gravity Thoracic cavity Volume decreases Elastic lungs recoil passively = intrapulmonary Volume decreases Intrapulmonary Pressure rises above atmospheric pressure (+1 mm Hg) Gases flow out of the lungs down the pressure gradient until intrapulmonary pressure is equal to atmospheric Figure 21.13 Tidal volume (TV) – air that moves into and out of the lungs with each breath (approximately 500 ml) Inspiratory reserve volume (IRV) – air that can be inspired forcibly beyond the tidal volume (2100–3200 ml) Expiratory reserve volume (ERV) – air that can be evacuated from the lungs after a tidal expiration (1000–1200 ml) Residual volume (RV) – air left in the lungs after strenuous expiration (1200 ml) Inspiratory capacity (IC) – total amount of air that can be inspired after a tidal expiration (IRV + TV) Functional residual capacity (FRC) – amount of air remaining in the lungs after a tidal expiration (RV + ERV) Vital capacity (VC) – the total amount of exchangeable air (TV + IRV + ERV) Total lung capacity (TLC) – sum of all lung volumes (approximately 6000 ml in males) Large Breath (Max) Normal Breathing Total air can use Air never used Includes Anatomical dead space – volume of the conducting respiratory passages (150 ml) Alveolar dead space – alveoli that cease to act in gas exchange due to collapse or obstruction Total dead space – sum of alveolar and anatomical dead spaces Alveolar ventilation rate (AVR) – measures the flow of fresh gases into and out of the alveoli during a particular time AVR (ml/min) = frequency (breaths/min) X (TV – dead space) (ml/breath) Slow, deep breathing increases AVR and rapid, shallow breathing decreases AVR Henry’s Law Dalton’s Law Talked earlier-Boyle’s Law When a mixture of gases is in contact with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure More of the gas and faster process 80% Oxygen 20% Oxygen Gas Liquid The amount of gas that will dissolve in a liquid also depends upon its solubility Various gases in air have different solubilities (into liquid portion of blood): ◦ Carbon dioxide is the most soluble ◦ Oxygen is 1/20th as soluble as carbon dioxide ◦ Nitrogen is practically insoluble in plasma Total pressure exerted by a mixture of gases is the sum of the pressures exerted independently by each gas in the mixture The partial pressure of each gas is directly proportional to its percentage in the mixture 78.6 % N2 20.9 % O2 0.04 % CO2 ATMOSPHERE 74.9 % N2 13.7 % O2 5.2 % CO2 ALVEOLI Familiar Concept - High pressure to low pressure Gases move from higher partial pressures to lower partial pressures. 78.6 % N2 20.9 % O2 0.04 % CO2 ATMOSPHERE 74.9 % N2 13.7 % O2 5.2 % CO2 ALVEOLI Alveolar Air PO2=104 mm Hg PCO2=40 mm Hg Oxygen Carbon dioxide RAPID DIFFUSION OF OXYGEN Carbon dioxide leaves the blood at the lungs because of its high solubility. Ventilation – the amount of gas reaching the alveoli Perfusion – the blood flow in pulmonary capillaries Ventilation and perfusion must be tightly regulated for efficient gas exchange Figure 22.19 1. 2. Bound to hemoglobin 98.5% Dissolved in plasma Hemoglobin-consists of 4 subunits The four subunits bind oxygen in a cooperative manner, so that binding of oxygen to one subunit makes it easier for the other subunits to bind to oxygen. Temperature - increases causes affinity of hemoglobin for oxygen to decrease pH - as pH drops, affinity of hemoglobin for oxygen decreases Active muscles-produce CO2 (low pH), heat and lactic acid Carbon dioxide is transported in the blood in three forms ◦ Dissolved in plasma – 7 to 10% ◦ Chemically bound to hemoglobin – 20% is carried in RBCs as carbaminohemoglobin ◦ Bicarbonate ion in plasma – 70% is transported as bicarbonate (HCO3–) Major Buffer As CO2 enters the plasma, it may react with water to form carbonic acid. Carbonic acid then quickly dissociates into bicarbonate and protons. CO2 + H2O H2CO3 HCO3- + H+ The conversion of CO2 and water to carbonic acid is generally a very slow reaction. However, erythrocytes contain an enzyme called carbonic anhydrase, which greatly speeds up this reaction. CO2 = carbonic acid = blood pH Medulla – sets rhythm (Pacemaker) A. Dorsal respiratory group (DRG) - pacemaker for breathing Neurons in the DRG fire - send signals to stimulate the diaphragm and external intercostals = inspiration Neurons stop firing- expiration occurs passively. Normal rate of stimulation by the DRG is about 1215 breaths per minute. Normal respiratory rhythm is called eupnea. B. Ventral respiratory group (VRG) role is not so clear, but it appears to be important during forced breathing. The basic rhythm set by the medulla can be influenced by the pons: A. Pneumotaxic center of the pons sends inhibitory signals to the DRG. This finetunes the duration of inspiration and helps to prevent over-inflation of the lungs. B. Apneustic center of the pons stimulates the DRG. This center works with the pneumotaxic center in fine-tuning the rate and depth of breathing. Factors influencing the rate and depth of breathing Medulla = basic respiratory rhythm, the rate and depth of breathing can be altered by: A. Irritants, such as smoke and dust, stimulate bronchoconstriction. ◦ also may stimulate coughing and/or sneezing B. Stretch receptors in the lungs are stimulated as the lungs expand. (Hering-Breuer reflex) ◦ Send inhibitory signals to the medullary respiratory centers that may end inspiration. ◦ Once the lungs recoil, the stretch receptors stop sending signals, and this inhibition of the medulla ends. ◦ May be important in protecting lungs from over-stretching ◦ Does not appear important to normal breathing. C. Hypothalamus - strong emotions and pain (consider a gasp of fear). ◦ Increase in respiratory rate in response to rising body temperature, and a decrease in rate in response to cold. D. The cortex - conscious control over breathing by directly stimulating motor neurons that excite the muscles involved in breathing. ◦ Has limits—you cannot hold your breath long enough to kill yourself! E. CO2 - Chemoreceptors in the brain stem monitor the level of CO2 in the CSF ◦ Hypercapnia (rising levels of CO2) = pH of the CSF, and decreasing pH stimulates the chemoreceptors. ◦ Chemoreceptors then send signals to the respiratory centers and stimulate increased rate and depth of breathing. ◦ A high level of stimulation may result in hyperventilation. Abnormally low levels of CO2 (hypocapnia) decrease respiratory rate and depth, possibly leading to hypoventilation and even brief periods of apnea (cessation of breathing). F. Concentration of oxygen in the blood is typically not very important in affecting breathing. However, if arterial PO2 drops below 60 mm Hg, then chemoreceptors in the aortic and carotid bodies stimulate the respiratory centers to increase ventilation. Chronic Obstructive Pulmonary Diseases (COPD) Smoking Dyspnea, coughing, infections and pulmonary failure 2 examples Obstructive Emphysema Enlarged alveoli, deteriated alveolar walls Chronic Bronchitis Excess fluid in lungs, inflammation, infection Asthma Active immune inflammation of airways Not simply irritant inflammation Corticosteriods Future antibodies against own antibodies Tuberculosis Mycobacterium tuberculois Hard, calcified tubercles Body can usually handle trough inflammatory and immune response Lung Cancer 1. Squamous cell carcinoma epithelium of bronchi get hollow holes which bleed out (cough up blood) 2. Adenocarcinoma starts on outer edges of lungs from alveolar cells 3. Small cell carcinoma grape cluster on mediastinum High pitch Low pitch Blood Vessels part of a venous plexus that provide heat-exchange to help condition the air. Epithelium Lamina propria Submucosa Adventitia Trachea Primary Bronchus Tertiary Bronchus Type II cell Type I cell Type II cell capillary RBC macrophage Rib cage ventilation