Skeletal System
advertisement
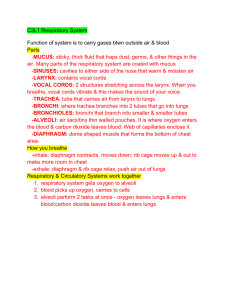
The Respiratory System Chapter 21 Introduction The trillions of cells making up the body require a continuous supply of oxygen to carry out vita functions We can survive only a few minutes without oxygen As cells use oxygen, they give off carbon dioxide a waste product of cellular respiration which the body must eliminate Introduction The major function of the respiratory system is to supply the body with oxygen and dispose of carbon dioxide To achieve this function four distinct processes, collectively called respiration occur – – – – Pulmonary ventilation External respiration Transport of respiratory gases Internal respiration (cellular respiration) Introduction Pulmonary ventilation – Air must be moved in and out of the lungs so that the gases in the air sacs (alveoli) of the lungs are continually changed and refreshed – This air movement is commonly called ventilation or breathing Introduction External respiration – Gas exchange (oxygen loading and carbon dioxide unloading) must occur between the blood and the air-filled alveoli of the lungs Introduction Transport of respiratory gases – Oxygen and carbon dioxide must be transported between the lungs and tissue cells of the body – This is accomplished by the cardiovascular system, which uses blood as the transporting fluid Introduction Internal respiration – At the systemic capillaries, gas exchanges (oxygen unloading and carbon dioxide loading) must be made between the blood and tissue cells Respiratory System The organs of the respiratory system include the nose, nasal cavity, paranasal sinuses pharynx, larynx, trachea, bronchi, and the lungs which contain the terminal air sacs or alveoli Respiratory System Functionally, the respiratory structures are divided into respiratory and conducting zones Visible structures represent the conducting zone Respiratory zone structures are small and lie deep within the lungs Respiratory System Functionally, the respiratory system consists of the respiratory and the conducting zones – The respiratory zone, the actual site of gas exchange, is composed of the respiratory bronchioles, alveolar ducts, and alveoli – The conducting zone includes all other respiratory passageways, which provide fairly rigid conduits for air to reach the sites of gas exchange Respiratory System Organs of the conducting zone clean, warm and humidify the incoming air Thus, the air reaching the lungs contain must less dust than what entered the nose and is warm and damp The Nose The nose is the only externally visible part of the respiratory system The external framework of the nose The Nose The functions of the nose include – Providing an airway for respiration – Moistening and warming entering air – Filtering inspired air and cleansing it of foreign matter – Serving as a resonating chamber for speech – Housing the olfactory (smell) receptors The Nose The structures of the nose are divided into the – External nose – Nasal cavity Surface features – – – – – – – Root (between eyes) Bridge Dorsum nasi Apex Philtrum External nares Alae The Nose - Nasal Cavity The nasal cavity lies in and posterior to the external nose During breathing air enters the external cavity by passing through the external nares or nostrils The nasal cavity is divided by a midline nasal septum The nasal cavity is continuous posteriorly with the nasal portion of the pharynx through the internal nares The Nose - Nasal Cavity The roof of the nasal cavity is formed by the ethmoid and sphenoid bones of the skull The floor is formed by the palate which separates it from the oral cavity below Anteriorly, where the palate is supported by the maxillary processes and the palatine bones is considered the hard palate The unsupported posterior portion is the muscular soft palate The Nose - Nasal Cavity The vestibule is lined with skin containing sebaceous and sweat glands and numerous hair follicles The hair, or vibrissae, filter coarse particles from inspired air The Nose - Nasal Cavity The nasal cavity is lined with two types of mucous membrane – The olfactory mucosa, lining the slitlike superior region of the nasal cavity, contain the receptors for the sense of smell – The balance of the nasal cavity is lined with respiratory mucosa The Nose - Respiratory Mucosa The respiratory mucosa is made up of pseudostratified columnar epithelium, containing scattered goblet cells, that rests on a lamina propria This lamina propria is richly supplied with compound tubuloalveolar glands that contain mucous and serous cells Mucous cells secrete mucus, whereas serous cells in glands secrete a watery fluid containing digestive enzymes The Nose - Respiratory Mucosa Each day the mucous glands secrete about a quart of sticky mucous containing lysozyme, an antibacterial enzyme The mucous traps inspired dust, bacteria and other debris, while lysozyme attacks and destroys bacteria chemically The epithelial cells of the respiratory mucosa also secrete defensins, natural antibotics that help to get rid of invading microbes The Nose - Respiratory Mucosa The ciliated cells of the respiratory mucosa create a gentle current that moves the sheet of contaminated mucus posteriorly toward the throat where it is swallowed and digested by stomach juices These ciliated cells become sluggish in cold weather allowing mucus to accumulate in the nasal cavity where it “runs” on a cold day when you come inside The Nose - Respiratory Mucosa The nasal mucosa is richly supplied with sensory nerve endings A sneeze reflex is stimulated when irritating particles (dust, pollen) contact this sensitive mucosa The sneezing propels air outward in a violent burst, expelling the irritant from the nose The Nose - Respiratory Mucosa A rich plexus of thin walled capillaries underlies the lamina propria of the nasal mucosa and warms the incoming air as it flows across the mucosal surface Blood flow increases when the temperature decreases Because of its superficial location and the extent of vessels, nosebleeds are common and often profuse The Nose - Nasal Conchae Protruding medially from each lateral wall of the nasal cavity are three mucosa-covered projections, the superior, middle of the ethmoid bone and inferior conchae which is a separate bone The Nose - Nasal Conchae The groove inferior to each concha is a meatus As inhaled air moves over the concha the turbulance created increases the amount of contact between the nasal mucosa and this inspired air This acts to trap particulates in mucus The Nose - Nasal Conchae The conchae and nasal mucosa not only function during inhalation to filter, heat, and moisten air, but also act during exhalation to reclaim this heat and moisture This reclamation mechanism minimizes the amount of moisture and heat lost from the body through breathing, helping us to survive in dry and cold climates The Nose - Paranasal Sinuses The nasal cavity is surround by sinuses located in the frontal, sphenoid, ethmoid and maxillary bones They function to – – – – Produce mucus Lighten the skull Warm the air Voice resonance The Pharynx The pharynx is the funnel shaped passage way than connects the nasal cavity and mouth superiorly to the larynx and the esophagus inferiorly Nasopharynx, oropharynx, laryngopharynx The Pharynx The pharynx serves as a common pathway for food and air The pharynx extends for about 5 inches from the base of the skull to the level of the sixth cervical vertebrae In the context of the digestive tract, the pharynx is commonly called the throat The Pharynx On the basis of location and function, the pharynx is divided into nasopharynx, oropharynx, laryngopharynx The muscular wall of the pharynx consists of skeletal muscle throughout its length, but the nature of the mucosal lining varies among the three pharyngeal regions The Nasopharynx The nasopharynx lies above the point of food entry, it serves only as an air passageway During swallowing the uvula reflects posteriorly to close off the nasopharynx and prevent food from entering the nasal cavity The Nasopharynx The nasopharynx is continuous with the nasal cavity through the internal nares It ciliated pseudostratified epithelium produces mucus Mucosa high on the posterior wall contains masses of lymphatic tissue, the pharyngeal tonsils or adenoids The Oropharynx The oropharynx lies posterior to the oral cavity and is continuous with it through an archway called the fauces Both swallowed food and air pass through Lined with stratified squamous epithelium for protection from food abrasion and chemical trauma The Oropharynx Two tonsils lie embedded in the oropharyngeal mucosa – Paired palatine tonsils – Lingual tonsil (posterior surface of the tongue) The Laryngopharynx The laryngopharynx serves as a common pathway for food and air and is lined with stratified squamous epithelium It lies directly posterior to the upright epiglottis and extends to the larynx where the digestive and respiratory pathways diverge The Laryngopharynx The esophagus conducts food to the stomach while air enters the larynx anteriorly During swallowing food has the “right of way” and air passage temporarily stops The Larynx The larynx attaches to the hyoid bone superiorly and opens into the laryngopharynx Inferiorly is is continuous with the trachea The Larynx The larynx has three important functions – It provides an airway for respiration – Act as a switching mechanism to route air and food into the proper channels – Vocal cords housed in larynx are used in voice production The Larynx The framework of the larynx is an arrangement of nine cartilages connected by membranes and ligaments Except for the epiglottis, all laryngeal cartilages are made of hyaline The Larynx The large, shield shaped thyroid cartilage is formed by the fusion of two cartilage plates The laryngeal prominence marks the midline fusion point The cricoid cartilage is anchored to the trachea inferiorly The Larynx Three pairs of small cartilages, the arytenoid, cuneiform and corniculate form part of the lateral and posterior walls of the larynx The arytenoid anchors the vocal cords The Larynx The ninth cartilage the flexible, spoon shaped epiglottis is composed of elastic cartilage It is almost entirely covered by mucosa The epiglottis extends from the posterior aspect of the tongue to its anchoring point on the thyroid cartilage The Larynx When only air is flowing into the larynx, the inlet to the larynx is open wide and the free edge of the epiglottis projects upward During swallowing the larynx is pulled superiorly and the epiglottis tips to cover the laryngeal inlet The Vocal Folds The vocal ligaments attach the arytenoid and thyroid cartilages These ligaments are composed of elastic fibers The vocal cords vibrate, producing sound as air rushes up from lungs The Vocal Folds The opening through which air passes is the glottis Superior to the vocal cords are the vestibular cords which play no part in voice production Vocal Folds Stratified squamous epithelium lines the superior portion of the larynx, an area subject to food contact Below the vocal folds the epithelium is pseudostratified ciliated columnar epithelium Cilia move the mucus away from our lungs Voice Production Speech involves the intermittent release of expired air and opening and closing of the glottis The length of the true vocal cords and the size of the glottis are altered by the action of the intrinsic laryngeal muscles most of which move the arytenoid cartilages As the length and tension of the vocal folds change, the pitch of the sound is altered Voice Production The glottis is wide when we produce deep tones and narrows to a slit for high pitched sounds Length and thickness of the vocal folds changes for males during puberty Loudness of the voice depends on the force with which the airstream rushes across the vocal cords The greater the force, the stronger the vibration and the louder the sound Sphincter Functions of Larynx The vestibular folds can perform a sphincter function under certain conditions In abdominal straining associated with defecation and urination, inhaled air is held temporarily in the lower respiratory tract by closing the epiglottis The abdominal muscle then contract and the interabdominal pressure rises The action know as the Valsalva manuever can also stabilize the trunk when one lifts a heavy load Innervation of the Larynx The larynx receives its sensory and motor innervation through the superior laryngeal branch of each vagus nerve and from the recurrent laryngeal nerves, which branch off the vagus in the superior thorax and loop superiorly to ascend through the neck The backtracking course these nerves is unusual The Trachea The trachea descends from the larynx through the neck and into the mediastinum It ends by dividing into the two primary bronchi at midthorax 10 cm long and 2.5 cm in diameter The trachea is very flexible and mobile The Tracheal Wall The tracheal wall consists of several layers that are common in many tubular organs of the body The Tracheal Wall From internal to external these layers are the mucosa, submucosa, and adventitia The Tracheal Wall The mucosa contains the same goblet cells containing pseudostratifed epithelium that occurs throughout most the of respiratory tract The Tracheal Wall Its cilia continually propel mucus, loaded with dust particles and other debris, toward the larynx The Tracheal Wall Smoking inhibits and ultimately destroys the cilia in the mucosa layer When their function is lost, coughing is the only means of preventing mucus from accumulating in the lungs Smokers with respiratory congestion should avoid medications that inhibit the cough reflex The Tracheal Wall The submucosa, a connective tissue layer, contains seromucous glands that help produce the mucus “sheets” within the trachea The Tracheal Wall The adventitia is a connective tissue layer that is reinforced by 16 to 20 C-shaped rings of hyaline cartilage The Tracheal Wall The cartilage rings prevent the trachea from collapsing and keep the airway open despite the changes in pressure that occur in breathing The Tracheal Wall The open posterior parts of the rings, which abut the esophagus are connected by smooth muscle fibers of the trachealis muscle and soft connective tissue The Tracheal Wall Since this portion of the tracheal wall is not rigid, the esophagus can expand anteriorly as swallowed food passes through it The Trachea The last tracheal cartilage is expanded and a spar of cartilage called the carina projects posteriorly from its inner surface, marking the point where the trachea splits Contacting this point results in violent coughing The Trachea Tracheal obstruction is life threatening The Heimlich maneuver was developed to expel an obstruction using the residual air in the victim’s lungs The maneuver creates interthoracic pressure that drives the obstruction from its lodging point The Conducting Zone The right and left main (primary) bronchi are the largest conduits in the bronchial tree The Conducting Zone The right and left primary bronchi are formed by the division of the trachea at the level of T4 (T7 living) The Conducting Zone Each bronchi runs obliquely in the mediastinum before plunging into the medial depression (hilus) of the lung on each side Conducting Zone: Bronchial Tree Once inside the lungs, each primary bronchus subdivides into secondary and then tertiary bronchi which then divide further (23 orders of branching) The Conducting Zone Air passages under 1mm in diameter are called bronchioles and the smallest of these are called terminal bronchioles and are less than 0.5mm The Conducting Zone The tissue composition of the walls of the primary bronchi mimics that of the trachea but as the conducting tubes become smaller, a number of structural changes occurs – The cartilage supports change • Rings are replaced by plates and then none at all – The epithelium type changes • Pseudostratified columnar, to columnar, to cuboidal • Debris removed by macrophages at bronchiole level – The amount of smooth muscle increases • A complete layer of circular smooth muscle allows for vasoconstriction and vasodilation The Respiratory Zone The respiratory zone begins as the terminal bronchioles feed into respiratory bronchioles within the lungs Protruding from these smallest bronchioles are scattered alveoli The Respiratory Zone The respiratory bronchioles lead into alveolar ducts The ducts lead into terminal clusters of alveoli called alveolar sacs Respiration takes place within the alveoli The Respiratory Zone About 300 million air-filled alveoli crowd together within the lungs, accounting for most of the lung volume All these cells provide for a tremendous surface area for gas exchange The total area of all alveoli in an average pair of lungs is 140 square meters, or 1500 square feet, which is 40 times greater than the surface of the skin The Respiratory Zone The wall of each alveolus consists of a single layer of squamous epithelial cells called Type I cells surrounded by a delicate lamina The Respiratory Membrane The cell walls are extremely thin to allow for ease of gas exchange The wall is 15 times thinner than a piece of paper The Respiratory Membrane The external surfaces of the alveoli are densely covered with a web of pulmonary capillaries Together the alveolar and capillary walls and their fused basal lamina form the respiratory membrane with gas on one side and blood on the other The Respiratory Membrane Gas exchange occurs by simple diffusion across the respiratory membrane Oxygen from the alveoli passes into the blood and carbon dioxide leaves the blood to enter the alveoli The Respiratory Membrane Scattered amid the type I squamous cells that form the alveoli walls are cuboidal type II cells Type II cells secrete a fluid containing a surfactant that coats the alveolar surfaces which prevents the walls from sticking during exhalation The Respiratory Membrane Lung alveoli have three other features – Surrounded by fine elastic fibers – Open pores connect adjacent alveoli • Allow for pressure equalization • Alternative air routes for blocked bronchi – Alveolar macrophages crawl freely along the internal alveolar surfaces The Respiratory Membrane Alveolar macrophages (dust cells) which actually live in the air space and remove the tiniest inhaled particles not trapped by the mucus Most dust filled macrophages migrate from the alveoli to the broncholes where ciliary action carries them into the pharynx to be swallowed By this mechanism over 2 million dust cells are cleared each hour! The Pleurae Around each lung is a flattened doulbe layered sac whose walls form a serous membrane called the pleurae There is an outer parietal pleura and an inner visceral pleura The Pleurae The parietal pleura covers the internal surface of the thoracic wall, the superior surface of the diaphragm and the lateral surfaces of the mediastinum It also enclosed the great vessels running to the lung root The Pleurae In the area of the lung root the membrane reflects inward forming the visceral pleura which covers the entire external lung surface The Pleurae The pleural cavity is the space between the parietal and visceral pleurae It is actually a slit like space filled with a layer of pleural fluid The Pleurae Secreted by the pleurae, this lubricating fluid allows the lungs to glide without friction over the thoracic wall during breathing movements The fluid also holds the parietal and visceral pleurae together, just as a film of oil or would hold two glass plates together The Pleurae The two pleurae can easily slide from side to side across each other, but their separation is strongly resisted by the surface tension of the fluid between the membranes Consequently, the lungs cling tightly to the thoracic wall and are forced to expand and recoil as the volume of the thoracic cavity increases and decreases during breathing The Pleurae The pleurae also help divide the thoracic cavity into three separate compartments – Central mediastinum with the heart – Two lateral pleurae each containing a lung The Pleurae The compartments prevent the moving lungs or heart from interfering with one another The compartments also limit the spread of local infections and the extent of traumatic injury The Lungs The lungs occupy all of the thoracic cavity except the mediastinum Each cone shaped lung is suspended in its own pleural cavity and connected to the mediastinum The Lungs The anterior, lateral and posterior lung surfaces lie in close contact with the ribs and forms a curving surface called the costal surface The apex is the superior tip of the lung The Lungs The concave inferior surface that rests on the diaphragm is called the base The hilus is the location where the pulmonary and systemic circulation and the primary bronchi enter The Lungs The left lung is divided into two lobes (upper and lower) while the right has three lobes (upper, middle, lower) Each of the lobes contains a number of bronchopulmonary segments separated by connective tissue Each lung has 10 similar segments The Lungs The bronchopulmonary segments have clinical significance in that they limit the spread of some diseases within the lung, because infections do not easily cross the connective tissue partitions between them The Lungs Furthermore, because only small veins span these partitions, surgeons can neatly remove segments without cutting any major blood vessel The Lungs The smallest sub division of the lung is the lobule Appearing on the lung surface as hexagons ranging in size from the size of a pencil eraser to the size of a penny each lobule is served by a large bronchiole In most city dwellers and in smokers the connective tissue that separates individual lobules is blackened with carbon The Lungs The lungs consist largely of air tubes and spaces The balance of the tissue, its stroma, is a framework of connective tissue containing many elastic fibers As a result the lungs are light, soft, spongy, elastic organs that weigh only 1.25 pounds The elasticity helps to reduce the effort required for breathing Blood Supply / Nerves of the Lungs The pulmonary arteries deliver oxygen poor blood to the lungs for oxygenation In the lung, these arteries branch along the bronchial tree Blood Supply / Nerves of the Lungs Generally, the arteries lie posterior to the corresponding bronchi The smallest arteries feed into the pulmonary capillary network around the alveoli Oxygenated blood is carried from the alveoli of the lungs back to the heart by the pulmonary veins, whose tributaries generally lie anterior to the corresponding bronchi within the lungs Blood Supply / Nerves of the Lungs The lungs are innervated by sympathetic, parasympathetic, and visceral sensory fibers that enter each lung through the pulmonary plexus on the lung root Parasympathetic fibers constrict the air tubules whereas the sympathetic fibers dilate them Ventilation Breathing or pulmonary ventilation consists of two phases – Inspiration is the period when air flows into the lungs – Expiration is the period when gases exit the lungs Inspiration During inspiration the lungs increase in volume by enlarging in all dimensions Inspiration lowers the air pressure within the lungs Air flows from areas of high pressure to areas of low pressure to equalize the pressure within the lung to that outside the lung Inspiration During normal quiet inspiration, the diaphragm and external intercostal muscles produce the muscle movement Inspiration When the dome shaped diaphragm contracts, it moves inferiorly and flattens As a result the vertical dimension of the thoracic cavity increases Inspiration The external intercostal muscles contract to raise the ribs Because the ribs normally extend anterioinferiorly from the vertebral column, lifting them enlarges both the lateral and anterior dimensions Inspiration Although these actions expand the thoracic dimensions by only a few millimeters along each plane, this movement is sufficient to increase thoracic cavity volume by almost a pint which is equal to normal resting inspiration Inspiration During deep or forced inspiration, additional muscles contract and further increase thoracic volume The rib cage is elevated by the scalenes and sternocleidomastoid in the neck and the pectoralis minor Expiration Quiet expiration in healthy people is a passive process As the respiratory muscles relax, the rib cage drops under the force of gravity and the relaxing diaphragm moves superiorly Expiration At the same time, the many elastic fibers with the lungs recoil The result is that the volume of the thorax and lungs decrease simultaneously, which pushes air from the lungs Expiration Forced expiration is an active process produced by the contraction of muscles in the abdominal wall, primarily the oblique and transverse abdominis muscles These contractions – Increase the interabdominal pressure which forces the diaphragm superiorly – Sharply depresses the rib cage and thus decreases thoracic volume Expiration The internal intercostal muscles, quadratus lumborum, and the latissimus dorsi also help to depress the rib cage End of Material Chapter 21