Genital Anomalies
advertisement
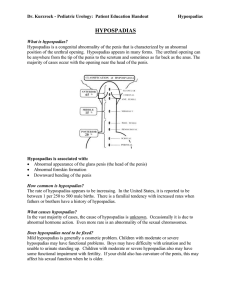
Genital Anomalies H. Salimi M.D. Hasheminejad Kidney Center Iran Medical University of Science Normal Anatomy Phimosis Paraphimosis Complication of Circumcision • • • • • • Bleeding Edema Infection Meatal stenosis Adhesions Penis loss Meatus stenosis Hypospadias • Ventral mallocation of meatus • Ventral chordee • No prepuce at ventral side Embryology • At the ninth week of gestation, the external genitalia begin to differentiate between the two sexes. • In the male fetus, genetic programming results in androgenic stimulation that induces posterior fusion of the genital folds and growth of the genital tubercle into a phallic structure . The penile urethra forms as a result of remolding and fusion of the medial edges of the endodermal urethral folds . • By 12 weeks gestation, the coronal sulcus separates the glans from the shaft of the penis. • By 16 to 18 weeks, urethral formation is complete, and the foreskin covers the glans. Pathogenesis • Disruption of the androgenic stimulation that is required for the development of the normal male external genitalia is the proposed mechanism resulting in hypospadias • Genetic factor • Exposure to estrogenic compounds (eg, maternal progestin or diethylstilbestrol) during pregnancy • In most cases of hypospadias, however, the cause is unknown. Both genetic and environmental factors are associated with hypospadias, suggesting that the etiology is multifactorial [These include the following: Advanced maternal age Pre-existing maternal diabetes mellitus Gestational age before 37 weeks History of paternal hypospadias Exposure to smoking and pesticides Epidemiology • Hypospadias is one of the most common congenital anomalies with an incidence that varies from 0.3 to 0.7 percent in live male births. • The risk of hypospadias appears to be increasing based upon population surveys throughout the world. Classifaication • mild – Urethral opening within the glans or subcorona : 50% • moderate– Urethral opening on the penile shaft : 30% • severe)– Urethral opening within the scrotum or perineum: 20% Evaluation • Initial evaluation — Once hypospadias has been identified, the initial evaluation includes: • a focused history • examination of the genitalia, and • identification of other congenital anomalies • Evalation for DSD Cryptorchidism and hypospadias Proximal hypospadias without cryptorchidism • Pelvic ultrasound to evaluate internal genitalia • Karyotype • Serum electrolytes as a screen for salt-wasting forms of congenital adrenal hyperplasia (CAH), one of the causes of DSD. Surgery • Timing • The American Academy of Pediatrics recommends that genital surgery be performed before 18 months of age based upon the premise that gender identity is not defined until 18 months of age • General consensus within the pediatric urology community is to perform surgery at six months of age in full term healthy infants Epispadias • Isolated • Associated with Bladder Extrophy Cryptorchidism Introduction • Cryptorchidism is the most common genital problem encountered in pediatrics • Untreated cryptorchidism clearly has deleterious effects on the testis over time – 89% of untreated males with bilateral cryptorchidism develop azospermia – Lifetime risk of neoplasia 2-3% • 4 fold higher than average risk • Despite more than 100 years of research, many aspects of cryptorchidism are not well defined and remain controversial Definitions • Cryptorchid: testis neither resides nor can be manipulated into the scrotum • Ectopic: aberrant course • Retractile: can be manipulated into scrotum where it remains without tension • Nonpalpable testes occur in approximately 20-30% of those who have cryptorchidism • Abdominal=10%; inguinal=68%; prescrotal= 24%; ectopic= 11.5%; • bilateral, 30%; and unilateral testis, 70%. Epidemiology & Risk Factors • Frequency 3.4 % in term boys , By 1 yo, incidence 0.8%. • Risk factors: • IUGR, prematurity – Incidence in premies 30% • • • • • • First-or second-born Perinatal asphyxia C-section Toxemia of pregnancy Congenital subluxation of hip Seasonal (especially winter) Radiology • Radiologic studies to localize the testis are currently of very little value. • To date, examination by a pediatric urologist has proven to be more valuable than ultrasound, CT scan, or MRA findings. • Ultrasound of abdomen and pelvis along with genitography should be used when the diagnosis of intersex is considered. • Laparoscopy if the testis is not palpable Treatment • Hormonal (HCG, GnRH) • Surgery Timing: 6 month in normal term boy Hernia , Hydrocele