3 Cardiovascular System
advertisement

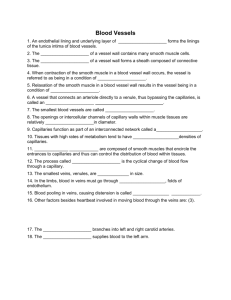
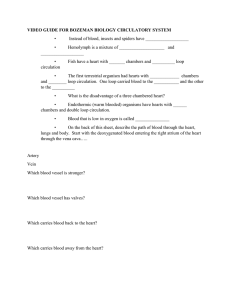
3 Cardiovascular System The Vascular System Categories and structures of blood vessels Arteries metarterioles arterioles capillaries venules veins Principles of fluid behavior #1: there is a universal law that relates force, friction and movement P P R F Flow rate F is proportional to the pressure gradient along the length of the tube (P – P) and inversely proportional to flow resistance R. Flow resistance is directly proportional to vessel length, but to the 4th power of vessel diameter. Translating this law to the vascular system as a whole… • The driving force for blood flow is the mean arterial pressure MAP (minus the venous pressure CVP, but this is so small we can almost neglect it) • The resistance is the total peripheral resistance TPR • The flow is the cardiac output CO, which is equal to the venous return VR • So, CO = (MAP- CVP)/TPR #2 In most vessels, blood flows fastest along the core of the vessel P P This is a laminar flow pattern. In turbulent flow, individual drops of blood swirl around rather than following a linear path. Turbulent flow can occur only within a few large vessels, or in special circumstances such as the vicinity of a cardiac valve. Where does pressure come from? • Gravity causes hydrostatic pressure when there is a difference in height. • Adding volume to an elastic vessel causes pressure to increase – this is how the heart generates arterial blood pressure. • So, blood pressure measured at any point in the body contains a combination of the two sources of pressure blood in a vessel above the level of the heart loses some pressure due to the gravity effect – below the heart, it gains some pressure. • However, the gravitational component cannot add to the driving force for blood flow because it applies equally to arterial and venous blood. #3 Blood flows from higher total energy to lower total energy • The total energy of flowing blood includes a potential form (seen as vessel wall pressure) and a kinetic form (the momentum of the flowing mass of blood). The partition of the total energy between the two forms is dependent on linear flow velocity. As blood flows along the length of a vessel, it spends kinetic energy as heat, while continuously converting its store of potential energy into kinetic energy. • When a vessel narrows, linear flow velocity goes up and wall pressure goes down. If a vessel is obstructed, linear flow velocity falls to zero and all of the energy reverts to wall pressure. Flow resistance and vessel branching • When a vessel branches, the flow resistance may increase or decrease, depending on the diameter of the branches. • So, when metarteries branch into arterioles, the effect of the branching is to greatly add to the resistance of the pathway, causing arterioles to be the resistance elements of the vascular system. • In contrast, when arterioles branch into capillaries, the effect is a decrease in resistance. Arteries • Wall is thick, tough, and relatively noncompliant (compliance is the change in volume of a vessel in response to a change in pressure) Smooth muscle • Three ‘coats’: – tunica externa – tunica media – tunica intima - endothelial cells + connective tissue Arterioles • Together with precapillary sphincters, individual arteries function to regulate blood flow through individual capillary beds. • Arterioles are the resistance elements of the circulation – so the sum of the resistances of all of the arterioles of the systemic loop largely determines the total peripheral resistance. Capillaries • Walls are thin, porous (usually), composed of endothelial cells without smooth muscle, except that the head of the capillary may have a precapillary sphincter. • Capillaries are the sites of all exchange of dissolved materials between tissues and bloodstream. Capillaries consist of endothelial cells lying on a basement membrane Veins • Walls are thinner and more compliant than those of arteries. • Diameters are larger. • As a result, about 60% of the blood is in veins at any instant, so they are the capacitance elements of the circulation. • Peripheral veins have valves that promote oneway flow The respiratory and skeletal muscle pumps Processes that apply a compressive force to veins (skeletal muscle contraction) or decrease central venous pressure (respiratory movements) favor the movement of blood from the venous reserve into the heart. These processes operate as pumps because of the presence of venous valves A trip through the systemic and pulmonary loops Pressure changes as blood passes through the systemic loop Thought question: how would arteriolar dilation or constriction affect this curve? Pressure changes in the pulmonary loop are smaller than in the systemic loop Compared to the systemic loop, the pulmonary loop is a lowresistance loop Control of the peripheral circulation The sympathetic n.s. exerts a major role in extrinsic control • Several regions in the medulla constitute the medullary cardiovascular center • Ordinarily, blood vessels (except capillaries) get only sympathetic input. • Both direct sympathetic innervation and circulating epinephrine are important in maintaining vascular tone. • For an individual vessel, whether an increase in sympathetic input will cause dilation or constriction depends on whether it is dominated by alpha receptors (constriction) or beta receptors (dilation). • For the systemic loop as a whole, alpha-dominated vessels are more influential than beta-dominated vessels. Extrinsic vascular regulation can… • Shift blood flow between body surface and body core in thermoregulation • Reduce blood flow to extrinsically dominated vascular beds in response to blood loss or hypotension • Shift blood flow from splanchnic beds to skeletal muscle in response to acute stress • Increase flow into splanchnic beds during sleep or after eating • Mediate genital sexual responses Intrinsic regulation (= autoregulation) allows individual tissues to match their blood flow to their metabolism This figure shows that tissues can control the flow resistance of their arterioles to keep flow constant in the face of pressure changes. Since pressure is usually well-regulated by central processes, the most important implication of this effect is that if tissue metabolism changes, intrinsic regulation will act to change flow rates while pressure remains constant. How does intrinsic regulation work? • Mediated by local factors and/or a direct response of arteriolar smooth muscle to stretch • Local factors include (depending on the tissue and the circumstances): oxygen, carbon dioxide, hydrogen ion, potassium ion, nitric oxide, prostaglandins, bradykinin, angiotensin, VIP, adenosine. Which vascular control system dominates depends on anatomy and function • Dominated by external control – Skin – Splanchnic beds – Resting skeletal muscle – genitalia • Dominated by autoregulation – Heart – Brain – Active skeletal muscle