Right Hand Panel
advertisement
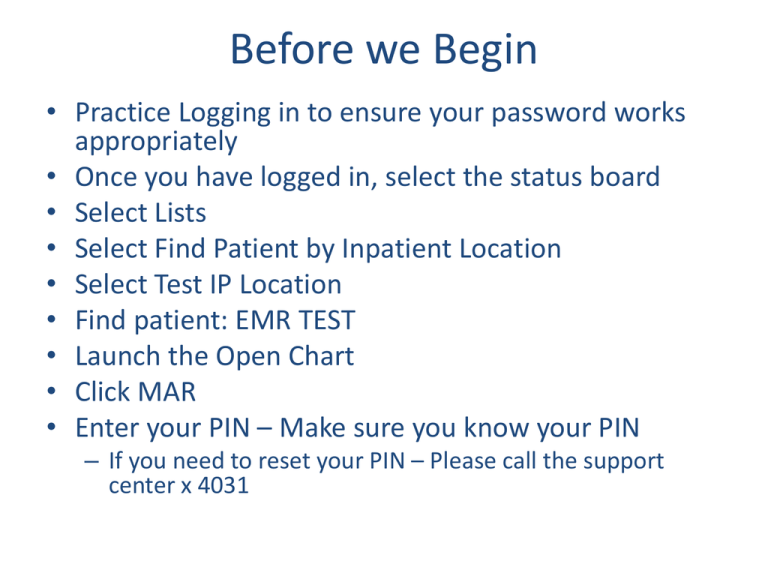
Before we Begin • Practice Logging in to ensure your password works appropriately • Once you have logged in, select the status board • Select Lists • Select Find Patient by Inpatient Location • Select Test IP Location • Find patient: EMR TEST • Launch the Open Chart • Click MAR • Enter your PIN – Make sure you know your PIN – If you need to reset your PIN – Please call the support center x 4031 Meditech 6.0 Upgrade RN OB/NB Session I Acronyms • PCS: Patient Care System – – – – Care Planning Intervention and Outcome Documentation Medication Documentation Notes • MAR: Medication Administration Record – Medication Administration Documentation • BMV: Bedside Medication Verification – Scanning Medication Barcodes to verify 5 Rights • EMR: Electronic Medical Record – Review clinical documentation • OM: Order Management – Enter Orders Agenda • PCS: Patient Care Systems – Overview – Status Board – Worklist – Care Planning – Documentation Functions • OM: Order Management – How to Enter Orders – Clinical Data Screen • EMR: Electronic Medical Record – Reviewing patient information Video Demonstration I New Admission and Care Plan Process New Admission and Care Plan Process Nursing Main Menu • List of Routines and Reports • PCS Status Board will provide most nursing care routines • Additional routines will be covered in more detail in Session II Status Board PCS Status Board Patient Assignment List Status Board Function Buttons • Patient Assignment List/Home Page • Displays Pertinent Patient Information – Relevant to the particular patient location Patient Care Routines & Function Buttons • ie: Psych, MedSurg, Rehab, etc • Continuously Refreshes with new information (every 5 minutes) • Launching pad to various patient care routines My List • Manually Add Patients to your list – Pts are Retained From One Log-on to the Next • Discharged Patients Remain on your Status Board until manually removed – Enables Care Provider to Complete Documentation even after the patient has left the facility • Manually Remove Patient from your List – Once you have Completed your Documentation and the patient has been discharged (or you are leaving for the day) • The more patients on your List the longer the status board will take to load Adding Patients to your List • [Lists] Button provides options to search for and add patients to your List – Find Account • Search for single patient by patient name – Find Patient by Inpatient Location • Provides a list of patients admitted to each location • Provides the ability to add multiple patients to your list at one time • Preferred method – My List • Launches your patient assignment list Video Demonstration II PCS Status Board PCS Status Board Exercise A: Find Patient by Location 1. 2. 3. 4. 5. Click [Lists] Click [Find Patient by Inpatient Location] Select [Test MVH IP Location] Click [Assignments] - Right hand panel Place a checkmark to the left of the following patient’s names • EMR, TESTPATIENTA • EMR, TESTPATIENTB 6. 7. 8. 9. Click [Add to My List] -Footer Button Click [Lists] - Right hand panel Select [My List] Confirm that both patients have been added to your assignment list Exercise B: Find Patient by Account 1. Click [Lists] 2. Click [Find Account] 3. Type Patient’s Name (Last Name, First Name) – Use the first Patient on the card taped to your PC. 4. Click to the select the patient account – Select the Account Number with the Admin In Registration Type – The status Board will Appear • • • • Click [Add to My List] – Footer Button Click [Lists] Select [My List] Confirm this new patient has been added to your List Open Chart Open Chart • All Inclusive Nursing Care Routine – – – – Review Patient Data Complete Assessment, Outcome, and Medication Documentation Enter Orders Enter Allergies and Home Medications Open Chart • EMR Electronic Medical Record – Review Patient Data • OM Order Entry – Enter Orders • PCS Patient Care System EMR – MAR Medication Administration Record • Document Medications – Care Planning • Add the Care Plan – Worklist • Intervention & Outcome Documentation – Write Note • Clinical Data • Enter Allergies • Enter Home Medications • Enter/Review Patient information OM PCS Open Chart: Patient Header Location, Room, Bed Age, Sex DOB Code Status Allergies Height/Weight/BSA Admit Status Medical Record Number Account Number Worklist OB Worklist Worklist Open Chart Routines Worklist Functions • Open Chart defaults to the worklist tab • Documentation Routine – Interventions, Assessments, & Outcomes Worklist: OB Standard of Care – Upon registration a Standard of Care Automatically defaults – Location Specific List of Interventions Care Plan Adding the Plan of Care • In Meditech, the first step for a new admission is to add the Care Plan • Select a location specific Care Plan – Includes Problems, Outcomes, Interventions common to any patient admitted to the particular location – Once the patient has been fully assessed the Care Plan will be individualized OB Delivery Care Plan Admission, Physical, and Daily Assessments Pain • Location specific Care Plan includes documentation common to any patient admitted to the particular Location • Care Plan Components – Admission, Daily, and Physical Assessments – Pain After Delivery… The specific focus of care selection for delivery (Vaginal, C/S, Perinatal Loss) will add: • Appropriate Recovery Documentation • Appropriate PP Shift Documentation • Appropriate Teaching Records • Discharge Documentation Newborn Care Plan Admission, Physical, and Daily Assessments Pain Feeding & Elimination Discharge • • Location specific Care Plan includes documentation common to any patient admitted to the particular Location Care Plan Components – – – – Admission, Daily, and Physical Assessments Pain Feeding & Elimination Discharge Worklist • Interventions and Outcomes will display on the worklist as added with the Plan of Care • Clicking the Frequency header will sort the list by frequencies – This will help to clarify which interventions are to be documented upon Admission Video Demonstration III Open Chart/Worklist/Add Care Plan Open Chart Worklist Add Care Plan Exercise C: Open Chart/Worklist/Care Plan 1. 2. 3. 4. Use the first TEST Patient on your PC paper Click [Lists] Select [My List] From your Assignment list, click to the left of the patient’s name to Launch the Open Chart 5. Confirm the Standard of Care list automatically defaults to the worklist 6. Click [Plan of Care] – Right Hand Panel 7. Click [Add] – Footer Button 8. Select Care Plan: OB DELIVERY Plan 9. Click [Save] – Footer Button 10. Review the Care Plan Components 11. Click [Worklist] – Confirm the Interventions and Outcomes from the plan of care appear on your worklist 12. Click the frequency header to sort the worklist by frequencies – This will highlight which interventions should be documented on admission Admission Documentation • The next step in the care planning process is to complete all admission documentation and physical assessments • Admission Assessments display separately on the worklist – Provides clarity as to which assessments have been documented vs. those that have not – Provides the ability to document one assessment or multiple assessments at one time – Same assessments are documented on admission as throughout the patients stay • Provides the ability to view documentation over time • Provides the ability to compare the current state to the state of the patient upon admission Documentation Overview Documentation Overview • Documentation mode defaults to flowsheet – Provides a view of prior documentation – Mode Button will toggle to Questionnaire mode • Similar to a paper assessment Documentation - Flowsheet Current Date/Time Defaults Gray Background = View Mode White Column = Documentation Mode Recall is Enabled for PMH Documentation - Questionnaire • Clicking Mode will toggle to Questionnaire Style • You may toggle between Questionnaire and Flowsheet mode at any time within documentation Video Demonstration IV Documentation Documentation Exercise D: Documenting PMH 1. 2. 3. 4. Use the first TEST Patient on your PC paper Start from the worklist Place a checkmark in the now column Click [Document] – Confirm the time column displays the current date/time in the header – Review the documentation • Displaying from the last admission 5. Click [Mode] to toggle to Questionnaire Mode 6. Document PMH: Asthma, Diabetes- Insulin Dependant, Tuberculosis, Eczema, Epilepsy, Patient is not at risk for aspiration 7. Any Body Systems with a Negative Response should be documented as None Reported 8. Click [Save] 9. Confirm the last done column updates with the last time the intervention was documented EMR Patient Care Panel • Displays PCS Documentation – – – – Assessments Interventions Outcome Care Plan Exercise E: Reviewing Documentation - EMR • • • • • • • • • • Use the first TEST Patient on your PC Click [Patient Care Panel] Confirm that the [Assessment] Tab Defaults Select to view the Past Medical History Documentation Place a Checkmark to the left of the Assessment Name Click [View History] Confirm that all documentation displays Click [Back] Click [Plan of Care] Tab – Header Click the [+] Symbol (in the description header) to Expand the Components of the Care Plan • Review the Care Plan Components Break 1 Hour 30 Minutes (15 Minute Break) Individualizing the Plan of Care OB Individualized Focus of Care • The Joint Commission Requires that each Care Plan be Individualized • Individualized Focus of Care Intervention – Tool to assist with care plan customization – Documentation occurs • After delivery to choose the appropriate selection • After the admission and physical assessments have been completed, as appropriate • When additional problems are indentified, PRN • Based upon the selections, problems and associated interventions will be suggested NB Individualized Focus of Care – Documentation on the focus of care occurs as problems are identified, PRN Individualized Focus of Care • Upon saving the focus of care selections, a list of problems is presented – Here, Vaginal Delivery and Diabetes (GDM/IDM) was selected Adding Problems • Place a checkmark to the left of every Problem presented • Click [Ok] OB Individualized Care Plan • The newly added problems will be viewable within Care Plan Routine Documentation Frequencies • Outcomes, Assessments and Interventions from the care plan display on the Worklist • Outcomes: required to be documented daily and upon discharge • Interventions/Assessments: vary based upon protocol and physician orders • Frequency column indicates how often to document • Last done column indicates the last time the assessment was documented • Frequencies can be edited as needed based upon a particular Order or Protocol Video Demonstration V Individualizing the Plan of Care Individualizing the Plan of Care Exercise F: Individualized Focus of Care • Use the first TEST Patient on your PC • Start from the worklist • Find the *Individualized Focus of Care –OB Intervention • Click in the now column • Click [Document] • Select: Vaginal Delivery, Diabetes (GDM/IDM) • Click [Save] • A List of Suggested Problems should display • Place a checkmark next to all and Save. • Click [Plan of Care] – Right Hand Panel • Confirm four new problems have been added Individualizing the Problem and Outcome • The next step in the care plan process will be to further individualize the problem and outcome • Problem – Indicate the specifics to which the problem relates • Outcome – Indicate specific goals that are being set to achieve the outcome Individualizing the Problem • Once the problems have been added • Select the Problem tab • Click to edit the item detail field to indicate the disease process for which the problem is related Exercise G: Customizing the Problem • • • • • • • • • • Use the first TEST Patient on your PC From the Care Plan Routine – Click the [Problem] Tab Click in the item detail column for the Problem: Pain Click [Edit] to enter text for the Problem Indicate that this problem is “Related to vaginal delivery, gr 3 with a peri-urethral laceration” Click [Save] Notice an “I” Displays in the Item detail column Click the I to view the Item Detail Confirm the newly documented info displays Click [Back] to return to the plan of care Individualize the Outcome • Next, click the outcome tab to list the goals that will be set to achieve the outcome • For each outcome, click in the item detail to indicate the specific goals will be set to achieve the outcome Outcome Customization • The documented goals will be viewable/editable from the worklist Exercise G: Customizing the Outcome • Use the first TEST Patient on your PC • Click the Outcome Tab to review the outcomes • Click in the item detail column for the Outcome: Reports pain at tolerable level • Click [Edit] to enter text for the Outcome • Indicate for the outcome that “Patient will demonstrate utilization of effective comfort measures” • Click [Save] • Notice an “I” Displays in the Item detail column • Click the I to view the Item Detail • Confirm the newly documented info displays • Click [Back] to return to the plan of care • Click Worklist and view the item detail text to view the outcome goals Care Plan Process: New Admission 1. Add a Location Specific Plan of Care 2. Complete All Admission Documentation – – – – – – – – – 3. OB Delivery or Antepartum Plan Newborn Plan of Care or NB Outside Adm If a GYN use M/S/ICU Plan of Care OB Arrival to Unit Admit/Transfer OB Admission Assessment Past Medical History OB Adm Physical Assessment Ht/Wt OB Vaccine Assessment Age 18+ Opt Out Vaccine Assessment Braden/Skin Risk Assessment Fall Risk/Safety/Precautions Assessment Customize the Care Plan – Adding Problems/Outcomes/Assessment based upon patient’s delivery status and/or condition Documentation Functions Documentation Functions • Temperature, Height and Weight Queries – Enable you to toggle between English and Metric Units within documentation • Instance Type Queries – Enable multiple instances of documentation for various body locations or situations • IV Insertions, Orthostatic Vital Signs, etc Documentation - Calculator • Enables you to toggle between English and Metric Units • Regardless of the units of documentation, the display will default to English Documentation – Instance Type – Enables multiple instances of documentation for various body locations, positions or situations • IV Insertions, Orthostatic Vital Signs – Click the drop down arrow to invoke the group response – Select the body location/situation – Click Ok Documentation – Instance Type • Document the fields for the situation/instance • Repeat the instance type documentation for the new body location • In this case, BP and Pulse will be documented for Lying, Sitting, and Standing Positions Documentation – Back Time • To back date/time your documentation, click the drop down arrow in the header • Adjust the date/time to reflect when the data was collected Documentation – Expand/Collapse • Clicking the [-] symbol will collapse the field within the section Documentation – Collapse • Notice the temperature section is now collapsed • You may now click the [+] symbol to expand • Some sections will default as collapsed – Notice the Thermal Management Documentation defaults this way and can be expanded as needed • Documentation that is infrequently utilized will default as collapsed and must be manually expanded as needed • The Manual Expand/Collapse will stick for the current assessment only Exercise F Part A: Documentation Functions - Back Documenting • • • • • • Use the first TEST Patient on your PC Select the [worklist] routine Select Vital Signs Click in the now column for the Vital Signs Click [Document] Back Document 1 Hour in the Past – In the Header, click the drop down to the right of the Date/Time Field – Change the time to 1 hour in the past • Next Step – Next Slide Exercise G Part B Documentation Functions – Calculator & Instance Type • Document – Temperature: 98.6 Oral – Pulse: 62 – Orthostatic Vital Signs (Instance Type) • Click “New Orthostatic Vital Signs” to start a new instance – Lying Left Arm 120/80 Pulse 62 • Click “New Orthostatic Vital Signs” to start a new instance – Sitting 118/78 Pulse 63 • Click “New Orthostatic Vital Signs” to start a new instance – Standing 115/70 Pulse 65 • Click [Save] Exercise H: Review Documentation in EMR • Click [Refresh EMR] • Select [Patient Care Panel] in the EMR • Place a checkmark to the left of the Vital Signs Assessment • Click View History • Confirm that the Vital Sign Assessment displays under the adjusted time (1 hour in the past) • Click [Back] • Click the [Vital Signs] Panel of the EMR and review the documentation Recall Values Recall Values • Recall Values provides the ability to pull prior documentation to the current assessment • This function is enabled for a select number of assessments • To invoke the recall values function, click the [Recall] Button Recall Values Recalls the entire assessment Recalls the section Recalls the individual query • Assessment displays in green • A column of diamonds appear to the right • Select the diamonds to recall individual queries, entire sections, or the whole assessment • It is critical that you review the recalled information to ensure accuracy before saving • Recalling & saving = Signing your name to the documentation Exercise I: Recall Values • Use the first TEST Patient on your PC • Document Past Medical History – – – – Click in the now column to select the intervention Click Document Click Recall Notice the screen turns green and diamonds appear in the right hand column – Click to recall one query: select to the right of the cardiovascular history – Click to recall the section: select to the right of the cardiovascular past medical history – Click to recall the entire assessment: select to the right of the Past Medical history • Confirm the entire assessment has recalled – Review all documentation to ensure accuracy – Update the GI Past Medical History Query – Click Save Worklist Management Worklist – Additional Functions Item Detail: Protocol, Associated Data, Item Detail Info Care Item: Intervention, Assessment, Outcome • • Frequency Last Done Worklist displays active and discharge statuses by default All other statuses are suppressed from view Status Adding a New Intervention • Most Interventions are added to the worklist through the plan of care • Additional Interventions may be added as needed • To add new interventions use the [Add] button Add Intervention Routine • The Quickest Method of searching for an Intervention is by [Any Word] – Searches the entire intervention name • Click [Any Word] and type the intervention name you wish to add Add Intervention Routine • Type the name of the intervention and click enter • Select the Intervention from the List and click save Exercise L: Adding a New Intervention • Patient’s primary language is Spanish and she prefers to discuss health related issues in this language. You will need to utilize the Telephonic/Video Interpretation device to communicate with your patient and her family. – Add the telephonic/video interpretation device intervention. – From the Intervention worklist, click [Add] – Type “Interpret” and hit [Enter] – Notice the intervention does not appear – Click [Any word] – Notice the Telephonic/Video Interpretation Assessment appears – Click the Intervention to select – Click [Save] – Confirm the Telephonic/Video Interpretation Assessment has been added to the worklist Item Detail Item Detail Column • Item Detail Column – P: Protocol – A: Associated Data – I: Item Detail Item Detail • Clicking the Icons will launch the item detail screen • Within Item Detail there are multiple tabs – Detail, History, Flowsheet, and Associated Data Item Detail Tabs • Detail – Info about Intervention – Intervention text (Post it note) • History – Audit trail of changes made to the intervention • Flowsheet – Documentation View in Flowsheet mode • Associated data – View of Data Fields related to the particular intervention Item Detail History Tab • Audit Trail of Changes Made to the Intervention – Activity: Document, Edit, Undo – User that documented, Care Provider Type, and Detail related to the change • Footer buttons: Edit/Undo documentation • Allows you to edit or undo your own documentation only – You may not edit or undo another users documentation Item Detail: Info • Item detail may be utilized as a communication tool • In the text field enter a note related to the intervention • In this case, the patient’s blood pressure must be taken on the left arm Item Detail: Edit Text • Enter the text that you wish to display with the intervention • Click save Item Detail Text The item detail will be viewable by clicking the “I” from the worklist or within the assessment Video Demonstration VII Item Detail/Editing & Undoing Documentation Item Detail Edit and Undo Exercise I: Item Detail/Editing • • • • • • • • • • • • • • Use the first TEST Patient on your PC Locate the Pain Intervention Click the “P” to invoke the Pain Protocol Review the Protocol Click [Close] to return to the worklist Find the Vital Signs Intervention Click in the [Item Detail] Column Select the [History] Tab Select the last instance of documentation Click [Edit] Document that the patient is on room air and O2 Sat is 98% Click [Save] Confirm a new Edit Line Item displays Click in the detail column (assessment icon) for the edit line item to review the old and new results Exercise J: Item Detail Text • Use the first TEST Patient on your PC • For the vital signs intervention, indicate that the blood pressure must be taken on the left arm – – – – – – – – – – Click in the item detail screen for the Vital Signs Intervention Click the [Detail] Tab In the text field, click [edit] Type: Patient’s blood pressure must be taken on the left arm Click [Save] Click [Back] to return to the worklist Click the “I” in the item details screen to view the information Click [Back] to return to the worklist This is comparable to a post it note or Edit Text in MT Magic Please note: The last documented text will print with the medical record Editing Worklist Frequencies • To edit a frequency, click on the frequency field • This will invoke a drop down menu • In the free text field type a “period” and enter a free text frequency (ie: .Q4H) Change Status • If an intervention is added in error, you may change the status to remove or suppress the intervention from view • Click in the status/due column and select to delete or complete the intervention Change View • The worklist displays active and discharge status items (only) by default • To bring inactive entries to view click Change View Change View • This routine provides the ability to update the worklist display • In this case, inactive interventions are selected to be added to the display. • Click Ok Change View – Worklist Display • Note the Inactive Intervention now appears • This intervention can be brought back to active status by selecting to edit the frequency Exercise K: Frequency and Worklist Status • Use the first TEST Patient on your PC • Find the Vital Signs Intervention • Edit the frequency of the intervention to .Q4H – – – – Click in the frequency field Type “.Q4H” Hit Enter Confirm the frequency is updated • Change the status of the Telephonic Interpretation Assessment to Complete – Click in the Status/Due column – Select Complete – Confirm the Intervention no longer displays • Bring the Telephonic Interpretation Assessment back to active status – – – – – Click Change View Select Complete from the Intervention status list Click Ok Find the Telephonic Interpretation Assessment and click Complete Change the status to Active Break 3 Hours 15 Minute Break OM/EMR Training Agenda • • • • • • • Introduction to the EMR Allergies, Code Status Order and Order Set Entry Consults and Uncollected Specimens Acknowledgment and Incomplete Orders Post-Filing Edits to Orders Entering Requisitions Intro to EMR • Electronic Medical Record • Integrated system so same information is viewable regardless of point of entry or desktop • Central access point for all results, patient demographic information, reports, clinical documentation, and clinical data. Intro to EMR •Selected tabs represent the EMR, viewable from all desktops with shared information •Patient header includes name, age, DOB, ht, wt, MRN, Acct number, Reg status, location/room/bed, and allergies •Items that have information “new to you” will be highlighted in red. “i”: More Information •Small “i” next to patient name provides additional information such as allergies, height, weight, admit date and time, BMI, and Code Status. Select Visits Panel •This panel allows you to select the visits for which you wish to view patient data. Choose a time period and visit type, or manually check off the visits you wish to view. Current visit is the default. Summary Panel •The summary panel holds clinical, demographic, and legal information regarding the patient. Allergies, home medications and problems (diagnoses) can be edited via the blue edit button. Allergies and home medications are usually edited on the Clinical Data screen which will be covered later. Summary Panel (cont) •The legal indicators page of the summary panel includes important patient information such as patient rights information, language, immunization, readmission data, blood type, precautions, fall risk, and Braden score. This information is also viewable for all visits by selecting the “all visits” tab. Review Visit •Review visit contains pertinent admission information including reason for visit and physicians associated to this patient visit. •The “More detail” footer button provides additional demographic and administrative information. •The patient abstract can be viewed and printed using the “Abstract” footer. Notices •The notices panel displays those notifications that have been sent to the physician desktop for acknowledgement. These include critical lab results, consultations, and certain nursing events such as patient falls. •The Send Notice button will allow users to manually queue this notice to another physicians desktop that may need to be aware of the result/event. New Results •The New Results panel shows new labs and reports that are new to you. They can be sorted to include data from the last 24 or 48 hours. Tests with multiple results will be listed in a separate date/time column. •All critical results in Meditech are shown highlighted in red/pink and abnormal results will always show in yellow. Clicking on the result will show additional information including the reference range for the test. Clinical Panels •Clinical panels are constructed to provide a comprehensive view of the patient by pulling various types of patient data onto one panel. Additional clinical panels can be found by selecting the “Panels” footer button. Displayed is the M/S Handoff panel. •Information is trended by date/time, but different time increments can be selected using the footer buttons. •You can also choose to pull in data from previous visits by selecting the Visits footer button. Vital Signs •Documented Vital Signs from the nursing assessment appear here. Additional documentations will be trended in an adjacent column by date/time. For patients with large amounts of documentation, the arrows at the top of the screen allow for scrolling through older documentation. I&O Documented intake and output will be listed here. Again data will be trended by date and time and can be adjusted to display increments of 1, 4, 8, 12, and 24 hours. Medications The default on the Medications tab, is the medication list which is a simple list of all medications during this patient’s visit, but can be expanded to include medications from all visits. Clicking the header of each column allows the list to be sorted accordingly. Additional filters can be applied using the footer buttons at the button. Medications cont The second tab on the Medications panel provides a view only display of the MAR. All information on the MAR can be viewed, but no documentation can take place here. You must visit the true MAR for this. The detail footer button allows for viewing of additional medication information, such as the flowsheet, monograph, medication detail, protocol/taper schedules, and any associated data. Laboratory The Laboratory Panel displays all lab data separated out by category. This defaults to the visits selected, but all visit data can be displayed by choosing that tab. Clicking the name of the test will launch you to a list of all results for that test. Clicking the result itself will launch you to a screen to view additional test data, such as the reference range. Laboratory cont Lab reports can be printed by clicking on the date and time header of the lab panel. The user will be launched to a collection data screen, where he/she can select lab report and print the data. Microbiology The Microbiology panel displays all microbiology tests that have been received into the lab. The status and results will be displayed with the procedure. Clicking on the notepad will launch the user out to the final report. Blood Bank The Blood Bank Panel allows for Blood related information to be tracked on the patients. The LAB/BBK department will update information in this panel along with the Blood Product Infusion Record/Reaction documentation done in nursing. Reports The reports panel shows all reports that have been entered on the patient, including radiology report, cardiology reports, dictated physician reports, physician documentation reports, as well as Allscripts reports once they are live in the system. *Initially Allscripts reports will be housed in the patient paper chart. Clicking the notepad will launch you to the report for viewing and printing. Patient Care The Patient Care tab provides a view only overview of all assessments and interventions documented on the patient. The plan of care is also viewable from here. The information can be sorted out by date, name, recorded by, and provider type. Patient Care cont Clicking onto the name of an assessment or intervention will launch you into a view only display of the documentation. No edits can be made from this panel. Notes The notes panel displays all notes entered on the patient by nursing, physicians, and other staff. Dictations and Physician Documentation reports (such as Progress Notes, H&P, Discharge Summary, etc) are not found here. They are on the reports panel. To view, either check off the box next to the desired note and click “View Selected” or clicking directly on the note. Orders Orders will be discussed in detail later in the training. For purposes of the EMR, however, the orders panel is accessible to all users on any desktop. All active orders will be displayed on the current orders table and the history panel contains these as well as cancelled, completed, and discontinued orders. EMR • Electronic Medical Record (EMR) Lunch Break 4 Hours 30 Minute Break Exercise M: EMR • Use: MTPatient,TEST • Where are two places in the EMR that I can find documented allergies on a patient (Hint: Clinical data is NOT part of the EMR)? • Where can I view the last medication administration in the EMR (Hint: your nursing MAR is not part of the EMR) • How can I easily tell whether a lab is of abnormal or critical value? • If I want to see a trend in a patients vital signs, how would I accomplish this? EMR Hands-On • Use MTPatient,Test • What is the easiest and most succinct way to locate a patients standard of care and individualized plan of care? • It is the end of your shift and you are preparing to hand off your patient, where would be the best place to find a comprehensive overview of that patient for that shift? Allergies In addition to the summary panel, allergies can be entered on the Clinical Data screen. Allergies can be entered and edited by clicking the blue edit button. Allergies cont To add a new allergy, click the “New” tab, and free text in your entry. A list of allergies should appear for you to select from. If your selection does not appear, the option to add the allergy as uncoded is available, but it is important to note this selection will NOT be included in interaction checking. Allergies cont Clicking on the allergy that is appropriate will launch you to the edit screen where you will be required to enter the type allergy (or adverse reaction), status, and the reaction associated. Allergies that are new will be highlighted on the list in green for editing. The Audit button gives a beginning to end view of the life of an allergy including edits made and by whom. Allergies • Entering and Editing Allergies Exercise N: Allergies • Enter a Penicillin Allergy – Reaction: Anaphylaxis – Severity: Severe • Enter “Little Blue Pill” – Uncoded Allergy – Reaction: Nausea – Severity: Mild • Save • Make an edit to the little blue pill – Change to an Adverse Reaction • Observe the audit trail. • Observe the status in the EMR. Code Status • Code status is entered as an order – Prior Advanced Directives Documented – Code Status – Code Status Limits (if applicable) – Advanced Directives Discussed and confirmed with Code Status Order/Display • Once the code status is entered – Code Status displays in Patient Header – Code Status and Limits displays in Summary Panel of the EMR – Code Status, Limits, Advanced Directives, and Health Care Proxy display in Clinical Panel – Code Status/Advanced Directives EMR Summary Panel Display - Code Status and Limits • Patient header displays Code Status • EMR Summary Panel displays Code Status and Limits EMR Clinical Panel Display • Code Status/Advanced Directive Clinical Panel displays – Code Status – Code Status Limits – Advanced Directives – Health Care Proxy Exercise: Code Status • Use Test Patient A from your PC • Enter a code status order – Full Code with Limits – Limits: No Dialysis – Save the Order • Confirm the Code Status Displays in the patient header • Review the EMR Summary Panel – Legal Indicator Tab • Review the Code Status Clinical Panel Order Management • Physicians will Go LIVE with Computerized Physician Order Entry on July 1st • Most Orders will be entered directly into Meditech • In the (rare) event that the MD is not able to enter the order into Meditech, orders may be entered for the MD by a Unit Secretary (Non Med Orders), or Nurse • The next training segment will review the steps for Entering Orders, Order Sets and Medication Orders Order Entry- Procedures Full orders functionality will be shown in the CBT coming up. To provide an overview, all non ordering providers will select an ordering provider and source upon selecting “New Orders”. This will launch you to your selection screen where you can order off of favorites, by category group, or by typing ahead in the name tab. With the type ahead, select the desired order. Multiple orders can be queued up by clearing the search field after selection and typing ahead again. Orders continued Clicking next will launch into the Edit Order list where all new orders and any potential duplicate orders will display. Any orders that have fields requiring edits will have an asterisk. Clicking that order will display the edit screen and fields with asterisks must be completed. Editing Order Frequency In the edit screen of an order, the frequency field can be free texted in. For series orders, the system recognizes DAILY and QXH. Simply enter the count in the count field and the stop time will automatically calculate. For DAILY orders the start time automatically defaults to the morning draw. Once all requirements are satisfied clicking next will take you to the Manage Orders screen where additional edits can be made if necessary. Orders cont Once you have reviewed on Manage Orders and click next you will be taken to the Current Orders table where new orders will be displayed with a green “New” status until filed. Clicking submit files the orders. Physicians require pin entry before filing. Order Sets Order sets are available for use by nursing should it be appropriate. They are especially useful in the ED where the Med Approved Protocols are available for use. The sets group orders together to support evidence based medicine and can be ordered by category or by searching by name. Multiple sets can be selected at one time. Order Sets cont Once the sets are selected, the manage orders list allows you to select the orders that are needed. Edits can be made by clicking the blue edit button on an individual order or by selecting edit all which will queue up orders for editing. The functionality here is identical to orders and they will be filed in the same way. Orders • Order Management for Non-Ordering Providers Order Sets • Order Sets for Non-Ordering Providers Exercise O: Orders •Enter orders from different categories •Imaging, Card, US, Lab, Mic, Bloodbank, Nursing, Consults •Make edits both individually and using “edit all”. Make one of the orders a DAILY order by free texting in the frequency field of a routine order. •Make note of the different screens on different types of orders. •Enter the Admit to General Medicine Order set •Select any orders relevant to your patient •File all orders together. Entering Medication Orders • First Select Ordering Provider and Order Source and Click [Next] • Select [New Meds] • Type the name of the medication and select the name from the search ahead lookup Entering Medication Orders • • • • Place a checkmark next to the appropriate schedule Click Edit to enter required information Update the Medication Order Click Submit and Save (or continue to enter additional medication orders Medication Ordering Process • One the medication orders have been entered, pharmacy will be required to verify the orders before they will be available on the MAR • Once Pharmacy has verified the orders, you will Acknowledge the Orders and document the administrations • MAR Documentation will be covered in session II Exercise: Entering Medication Orders • Enter the following Medication Orders into Meditech: – Enoxaparin 30 mg SC Daily – Lisinopril 10 mg PO Daily – Furosemide 20 mg PO Daily • • • • • • • • • • • • • Click [Orders] Select the Ordering Provider and Source Click [Ok] Click [New Meds] Use the type ahead lookup Select the appropriate order string Click [Next] Edit the order information Click [Next] Click [Next] Click New Med Enter the last 2 medications and click submit at the end Navigate to the Status Board and Select the Orders queue to confirm that the 3 new medication orders have been entered Consult Orders The edit screen of a consult order differs for ordering versus non-ordering providers. Physicians are not require to enter consulting provider, so their consults file as incomplete to be completed by the nurse or secretary. Once the consulting provider information is entered additional information regarding communication to the consulting provider should be entered. A notification is sent to the physicians desktop when this information is entered. Incomplete orders will display on the statusboard as such and on the current orders table. Uncollected Specimens When a lab or micro specimen is ordered and set to be collected by the nurse, it will flow to his/her worklist for collection. To document that it has been collected, check in the now column and click document. If a source has not been entered, it must be entered at this time. Filing the documentation automatically updated the order to collected and it is filed in lab. Consults and Specimen Collection • Consults and Specimen Collection Exercise P: Uncollected Specimen • Use the first TEST Patient on your PC • Practice entering various consult orders and note the required fields. • Place multiple lab and micro order set for the Nurse to collect. Note the status of the order on the current orders table. Collect specimen off of worklist. Acknowledgement of Orders All orders and order edits must be acknowledged by nursing. The Ack column on the status board allows for this to be done efficiently. Stat orders will be flagged as Stat and highlighted in pink. Routine orders will display with “Ack” in the column. Click into the column to acknowledge. Acknowledgement cont Each order must be selected and reviewed individually to acknowledge. Once you have reviewed each order, click the Acknowledge button. To restore them to unacknowledged before filing hit Undo. Otherwise click save to file the acknowledgment. You will then be brought to the manage orders screen. Acknowledging Orders • Acknowledgement of Orders Exercise Q: Acknowledging Orders • Use the first TEST Patient on your PC • Click into the Ack queue on the status board for your patient. • Check off each order individually. • Review Order Detail. • File. Editing after Filing To edit an existing order, click on the order in current orders, and make any edits on the edit order list page that you are brought to. Editing a connecting order (lab, pha, mic, rad, card) will place a stop request on the original order and file your edits as a new order. Editing after Filing cont Orders can also be edited from the Edit Multiple Button located on the Current Orders table. Multiple orders can be checked off here and edited using the available footer buttons. Again for connecting orders, edits made to the connecting orders (outside of the specimen collection field) will place a stop request on the order and file the edits as a new order. Exercise R: Editing Orders • Use the first TEST Patient on your PC • Make edits to both connecting (labs, mic, rad) and non-connecting (nursing, consults, diets) orders to observe the change in statuses. Make note of those orders that stop request when edited. Requisitions • Requisitions are a means of communication for information that is not patient specific • Requisitions can serve as requests for supplies or communications to other departments Requisitions On the edit screen simply enter in your message/communication. Once filed the order will print to the receiving party. Requisitions • Entering Requisitions Exercise S: Requisitions • Use the first TEST Patient on your PC • Enter the Requisition desktop and observe the different requisitions for the Morton facility • Practice entering requisitions. Suggested Orders – Nursing Documentation • Some Nursing Documentation is set to trigger suggested orders/consults • ie: OB Admission Assessment may trigger – Social Services Consult, Nutrition Consult, etc • In this case, answering yes to the nutrition consult query will trigger a suggested order for a nutrition consult Suggested Order • The suggested orders screen displays • Select the order and select Order Now or Undecided Remind again (if not appropriate) • To proceed to Order Management, Click Ok Suggested Order – Order Management • The ordering provide and source will be selected • Manager Order fields will be documented • And, once the order is ready to be transmitted, click Submit Exercise T: Suggested Orders • Use the first TEST Patient on your PC • Document the OB Admission Assessment – Typically, you would document all fields. For this example, document only the information indicated below under the OB General Information section: – Information Provided by: Patient – Patient Smoking Status: Never Smoked – Nutritional Consult indicated-YES – Patient has an Advanced Directive and it is on file from prior visit – Patient has a Health Care Proxy and it is on file from prior visit – Click Save – You are brought to the suggested orders screen Exercise: Suggested Orders cont’d • From the suggested orders screen, select Nutrition Consult and click Order Now • Click [Ok] • From Order Management, select the ordering provider and the order source • Click [Ok] • You are launched into Order Management • Enter the required fields (indicated by an *) and any additional information • Next, click Submit • The order has been entered • Navigate back to your status board – Click My List • Next, Click the ACK prompt for your patient • And, confirm the nutrition consult has been ordered • Acknowledge the Nutrition Consult Daily Documentation OB Daily Documentation • Vital Signs • OB Shift Assessment (which includes): – OB ADL Record – Postpartum Assessment – Physical Systems Assessments • • • • Fall Risk/Safety/Precautions Assessment Pain Assessment Patient Teaching Outcome Documentation NB Daily Documentation • • • • • Vital Signs Ht/Wt NB Physical Assessment NB Shift Care Record NB Feeding Record – NB Breast Milk check for dispensing EBM • NB Elimination Record • NB Pain Assessment • Outcome Documentation Physical Assessments Within Normal Limits • For admission, the OB Adm Physical Assessment will be used • For assessments after delivery, physical assessments will be found in the OB Shift Assessment – Document abnormal findings – If the patient is within normal limits, you may use the within normal limits statement to indicate this finding Clinical Update Panel Comments • Within each of the physical assessments, there is a Clinical Update Query • This is to document notable events related to the particular body system • This query pulls to several EMR panels & provides a snapshot of notable events • Supports communication between the care team members and can be viewed in the Clinical Update Panel OB Clinical Review Panel • Used for information snap shot and hand-off – Useful for nurses as well as OB’s • Includes: – – – – – – – VS Prenatal Hx Delivery Info PP Assessment PIH data Labs Medications NB Clinical Review Panel • Used for information snap shot and hand-off – Useful for nurses as well as Pedi’s • Includes: – VS – Delivery Info – Wgt/Length/I&O – Feeding Record – Labs – Medications OB Clinical Review Panel PP, NB and Breastfeeding Education • Each of these interventions uses the “Instance function” for documenting the individual topics – This will display all of the topics that have been “covered”, making education efforts more focused – This information can be seen in the EMR panel: Education Review Documentation Example: OB PP Education: Topics: OB and NB Outcome Documentation • All outcomes are documented daily • OB and NB outcomes have “criteria” which explain what is meant if the goal is “met” • Additional comments are always welcomed to make the documentation more individual for the patient and further explain why an outcome may not be met or only progressing toward goal, along with any changes in the “plan” • The education outcome states whether education was provided or not and there is a comment to describe anything pertinent about the efforts to education PRN Exercise U: Physical Assessments – Within Normal Limits • Use the first TEST Patient on your PC • Place a Checkmark next to the OB Adm Physical Assessment • Document the Cardiovascular Assessment is within normal limits • Document Crackles in the left upper lobe for the respiratory assessment • Document the patient had wheezing that was treated by RT at 1200 in the Clinical Updates Comment • Document Genitourinary Assessment is within normal limits • Save • Review the documentation in the M/S- Hand Off Panel (as an example) and in the Clinical Update Panel • Note: physical assessments do NOT go to the OB or NB Clinical Review panels • Vital Signs Exercise – Document a set of vital signs • Teaching – Document the OB/NB Infant Care Education • Document that you taught the mom about Infant cues and communication and that she verbalized an understanding of the information • Intake and Output Assessment – Document intake for the shift: 100 mls – Urine Output: 50 mls from indwelling catheter • Outcome Documentation – Place a checkmark next to outcomes of Maternal /Fetal risk and Stable PP recovery – Maternal/Fetal Risk->Document “Goal Met” – Stable PP recovery->Document “Progressing Toward Goal” with comment “Increased bleeding in immediate postpartum, requiring additional medication” – Change status of Maternal/Fetal Risk to Complete as it no longer needs to be documented Notes Routine • Write Note provides the ability to enter free text notes • Most Documentation is included within the Assessments • Additional Information should be entered within the Assessment comments • Notes should rarely be utilized – Reserved for unusual events that are not available within the assessments – Also utilized to generate Discharge Instructions and Page 2 Reports • Be careful not to double document within the notes routine • All Clinical Documentation is viewable from within the EMR Notes Routine • To begin documenting click write note • Next, select the note category (i.e. Nurse) Write Note • You may choose to document a free text note • Or, select Text to enter a canned text (pre populated note) Canned Text • Upon selecting canned text, a list of available notes will display • Once the canned text is selected, the pre populated information will display within the write note screen. Canned text may be edited before saving. Exercise V: Notes Routine • • • • • • • • • • Use the first TEST Patient on your PC Select Write Note Select Note Category: Nurse Select the Text Button From the list of Canned Text, Select Patient Off Unit Click F4 to navigate through and enter each of the free text fields Click Ok Click Refresh EMR Notice the Notes Button Turns Red Click to view the note within the EMR Comprehensive Exercise • • • • Use the SECOND TEST Patient on your PC Find Patient by Account Add Patient to your List Add a new OB Delivery Plan of Care (pt is being admitted for a scheduled C/S) • Enter Patient Allergies and Height and Weight • Document – – – – – • • • • OB Arrival to Unit/Admit or Transfer OB Admission Assessment Past Medical History OB Adm Physical Assessment Select the C/S Delivery from the OB Focus of Care and add the suggested problems Add a new intervention: Blood Product Infusion Record/Reaction Document Patient Teaching Document all outcomes Review all documentation in the Patient Care Panel of the EMR How to Discharge a Patient: Registration Management How to Discharge a Patient • The Discharge Process will be covered in session 2 – Documentation – Reports – Instructions • Next, you will learn to discharge a patient from registration management How to Discharge a Patient • From the main menu – select Registration Management Discharge Routine • Perform a lookup to select the registration status • Type Patient Information to identify the appropriate patient • Click Ok Discharge Routine • Select the patient account from the Account Lookup Screen Discharge Routine • Document the date and time of discharge and discharge disposition • Click Next to Navigate to the next screen and document the appropriate information • Save Exercise: Discharging a Patient • • • • • • • • • • • Navigate to your main manu Select Patient Registration Select the Discharge Tab Type: IN Name: Use your test patient (from your PC) Discharge Date: Today Discharge Time: Now Discharge Disposition: HOM Click [Next] and enter “N” at required field Click [Save] Repeat process for 2nd patient used during this class Thank you!



