Anatomy of the Digestive System
advertisement

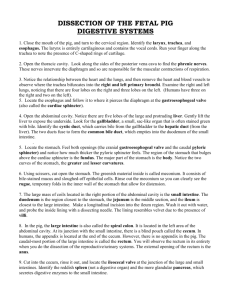
Anatomy of the Digestive System Chapter 25 Target Test Date (Chapters 25 & 26): Block Days 4/6-4/7 Gastrointestinal (GI) Tract Walls of the GI Tract 1. Mucosa – inner lining of tract – secretes mucous – Highly folded – increased surface area for absorption • Microvilli – Composed of 3 layers • Mucous epithelium, lamina propria, muscularis mucosae Walls of the GI Tract 2. Submucosa – Mainly connective tissue – Contains: • Exocrine glands – Secretes acids & enzymes • Parasympathetic nerves form the submucosal plexus Walls of the GI Tract 3. Muscularis – Smooth muscle • 2 layers – – – – Longitudinal (outer) Circular (inner) Move particles by peristalsis Myenteric plexus: found between 2 layers of smooth muscle Walls of the GI Tract 4. Serosa – – – Outermost layer Connective tissue and peritoneum (visceral layer) Mesentery connects the parietal & visceral portions of the peritoneum Walls of the GI Tract – Cell Modifications • Although the layers remain the same throughout the GI tract, the cell types may change – Ex: Mucosa layer of the esophagus is composed of stratified squamous cells to resist abrasion, but transitions to simple columnar cells for absorption and secretion Mouth • Also called the oral or buccal cavity • Composed of: – Lips, cheeks, tongue, hard palate, soft palate Tongue • Skeletal muscle covered by mucous membrane • Helps in chewing (mastication), swallowing (deglutition) and speech • Papillae cover upper portion of the tongue – Vallate: posterior portion of tongue; contain taste buds – Fungiform: sides and tip of tongue; contain taste buds – Filiform: anterior 2/3 of tongue; do not contain taste buds Tongue • Frenulum – anchors tongue to floor of the mouth – Ankyloglossia: frenulum is too short; results in speech problems; “tongue-tied” • Floor of mouth and underside of tongue are very vascular – Sublingual drugs (nitroglycerin, morphine) Salivary Glands • Parotid – Upper jaw; anterior & inferior to external ear – watery saliva containing enzymes • Sublingual – floor of the mouth – Mostly mucous saliva • Submandibular – Opens on either side of the frenulum – Mixture of watery (enzymes) and mucous secretions Teeth • Organs of mastication • Increase surface area that digestive enzymes can work on food • 3 main sections: – Crown: exposed portion; covered by enamel – Neck: surrounded by the gingivae (gums) – Root: fits into the alveolar process of the jaw (gomphosis) Teeth • Children - 20 teeth – deciduous or primary • 16 teeth per jaw - 32 total (adult) – Incisors (4) • blade shaped - used to tear food – Canines (Cuspids) (2) • Pointed teeth - used to tear food – Premolars (Bicuspids) (4) • 2 points - used to tear and grind food – Molars (6) • 4 points - used for grinding • Last set called wisdom teeth Esophagus • Collapsible, muscular, mucous-lined tube • 25cm; extends from pharynx to stomach • Posterior to trachea • Upper esophageal sphincter (UES) – prevents air from entering during respiration • Lower esophageal sphincter or cardiac sphincter Esophagus • Esophageal hiatus – hole in the diaphragm through which the esophagus enters the abdominal cavity – Enlargement results in lower portion of esophagus and stomach bulging upward into the chest hiatal hernia • Gastroesophageal reflux disease (GERD) – backward flow of stomach acid through the cardiac sphincter into the lower esophagus Warm Up 3/9-10/11 Announcements: 1. Make up test ASAP 2. No tutoring/make ups today after school 3. Progress Report grades due this Friday 4. Bring book & packet on Friday Warm Up: 1. Name the 4 layers of the GI tract (inner to outer). List one fact about each layer. 2. Name the 3 salivary glands. What type of saliva is produced from each? 3. What is a hiatal hernia? 4. On what areas of the tongue are taste buds found? Warm Up 3/11/11 Announcements: 1. You need your book and packet – go get it. Warm Up: 1. True/False: The layers of the GI tract and cell types are consistent from mouth to anus. 2. Name 3 functions of the tongue. 3. True/False: The tongue is poorly vascular. 4. How does the number of teeth differ between children and adults? 3/21/11 Announcements: 1. Welcome Back!! 2. No warm up today 3. Packet due block day 4. Quiz block day (covers chapter 25 notes through tomorrow) 5. Practical Friday (cat digestive organs and labeling) Stomach • Elongated, pouch-like structure • Mostly in LUQ • After eating the stomach walls distend; when empty size of large sausage • In adults holds 1-1.5 liters Stomach Landmarks (fig 25-10) • • • • Fundus – enlarged upper left portion Body – central portion Pylorus – lower portion Lower esophageal sphincter (also cardiac sphincter) • Pyloric sphincter • Lesser curvature • Greater curvature Modifications of the Stomach Wall • Gastric Muscosa – – – Arranged into folds which allow for distention (Rugae) Contains gastric glands which are surrounded by gastric pits Gastric glands secrete gastric juice • 3 major secretory cells: 1. Chief cells: secrete enzyme of gastric juice 2. Parietal cells: secrete hydrochloric acid (HCl) 3. Endocrine cells: secrete ghrelin (stimulate hypothalamus to increase appetite) and gastrin (influences digestive functions) Modifications of the Stomach Wall • Gastric Muscle – Muscularis layer is composed of 3 smooth muscle layers – Superficial to deep • Longitudinal • Circular • Oblique – Allows stomach to contract at many different angles Modifications of the Stomach Wall • Serosa Layer – Visceral layer forms the greater omentum (over intestines) and lesser omentum (connects stomach to liver) Small Intestine • 1 inch in diameter; 20 feet in length • 3 divisions: – Duodenum • 10 inches • C shaped – Jejunum • 8 feet • Begins where the sm. intestine turns forward and downward – Ileum • 12 feet Walls of the Small Intestine • Mucosa lining has circular folds plicae • Small projections called villi (singular – villus) cover plicae – 1 mm in height – Contain an arteriole, venule and lymph vessel – Epithelial cells on the surface of villi contain approx 1700 microvilli per cell • Villi and microvilli increase surface area for absorption Walls of the Small Intestine • Goblet cells are located on villi and in crypts – Secrete mucus • Secretory cells in each crypt produce an enzyme that prevents bacterial growth in the small intestine Large Intestine • 2.5 inches in diameter; 5-6 feet in length • Divisions – Cecum – Colon – rectum Divisions of the Large Intestine • Cecum – First 2-3 inches of the large intestine – Blind pouch in right quadrant Divisions of the Large Intestine • Colon (4 divisions) – Ascending • Vertical position in right quadrant • Ileum joins superior to cecum • Ileocecal valve allows material to pass into the large intestine – Transverse • Horizontal position below liver, stomach & spleen • Extends from the hepatic flexure to the splenic flexure Divisions of the Large Intestine – Descending • Vertical position in the left quadrant • Extends to the level of the iliac crest – Sigmoid colon • Below iliac crest • Means “s-shaped” • Bends from L to R Divisions of the Large Intestine • Rectum – Last 7-8 inches of the large intestine – Anal canal is the last inch • Mucous lined vertical folds anal columns – Opening = anus Walls of the Large Intestine • Intestinal mucous glands – Secrete mucous that coats feces • Longitudinal muscles are grouped into tape-like strips called taeniae coli • Circular muscles are grouped into rings which form pouches haustra • Circular muscles in the rectum form rectal valves 3/22/11 Announcements: 1. Packet due block day 2. Quiz block day 3. Practical (identification & labeling) Friday Warm Up: 1. The folds in the stomach which allow for distention are called: 2. Name 3 modifications of the stomach wall. 3. List the divisions of the small intestine from superior to inferior. 4. The transverse colon extends from the _________ to the ___________. 5. Name the 3 modifications in the small intestine which increase surface area (from largest to smallest). Vermiform Appendix • Attached to the cecum in the RLQ • 3-4 inches in length • “breeding ground” for intestinal or normal flora – Nonpathogenic bacteria – Aids in digestion and absorption Appendicitis • Mucous lining becomes inflamed • Fecal matter or food becomes trapped causing irritation and inflammation • Rupturing of the appendix results in infectious materials in the abdominal cavity – May cause infection of the peritoneum and/or other abdominal organs Appendicitis • S/S – Nausea/vomiting – RLQ pain (McBurney’s Point) – Rebound tenderness • An enlarged appendix can be removed through a laparoscopic surgical procedure Peritoneum • Continuous sheet of serous membrane – Lines walls of abdominal cavity (parietal layer) – Outer layer of abdominal organs (visceral layer) • Binds abdominal organs together – Mesentery: projection of the parietal layer • Attached to small intestine • Allows free movement without becoming tangled (volvulus) – Greater omentum: continuation of the stomach’s serosa layer • Covers small intestines – Lesser omentum • Attaches from the liver to the stomach Liver • Largest gland in the body • Weighs 3-4 pounds • RUQ Anatomy of the Liver • Two lobes connected by the falciform ligament – Left lobe 1/6 the size of the right lobe – 3 divisions of the right lobe • Right lobe proper, caudate lobe and quadrate lobe (seen inferiorly) (fig 25-22) Anatomy of the Liver Anatomy of the Liver • Hepatic lobules – anatomical units of the liver – Pentagon-shaped cylinders • Blood enters the lobules from the hepatic artery & hepatic portal vein – Arterial blood oxygenates – Venous blood passes for inspection • Kupffer cells remove bacteria, old RBCs, dissolved toxins • Venous blood continues to the inferior vena cava – Bile formed by hepatic cells passes though the canaliculi to the bile ducts Fig 25-23, page 758 Bile Ducts • Small bile ducts merge to form R and L hepatic ducts – R and L hepatic ducts form common hepatic duct – Cystic duct and common hepatic duct form common bile duct – Common bile duct opens into the duodenum – Fig 25-25 Bile Ducts Liver Functions • Detoxification • Bile secretion (aids in the absorption of fats) • Protein, fat and carbohydrate metabolism • Hematopoisesis (blood cell production) Gallbladder • • • • • • Pear-shaped sac 3-4 inches long Can hold 30-50mL of bile Located on inferior surface of the liver Rugae (similar to stomach) Functions: – Stores and concentrates bile – Contracts and ejects bile into duodenum during digestion Cholecystitis • Inflammation of the gallbladder • Often caused by gallstones (cholelithiasis) – Solid precipitants; mostly cholesterol – High incidence in obese individuals and those undergoing rapid weight loss • Treatment: – Laparoscopic cholecystectomy – Ultrasound lithotripsy – Oral medications (Actigall) Pancreas • 6-9 inches long • LUQ; behind stomach extending to the spleen • Endocrine & Exocrine tissue • Exocrine tissue arranged in a compound acinar formation (grapelike) – Release digestive enzymes into microscopic ducts which join to the main pancreatic duct – Pancreatic duct empties into the duodenum