HF presentation
advertisement
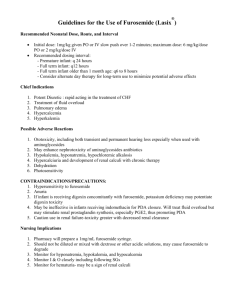
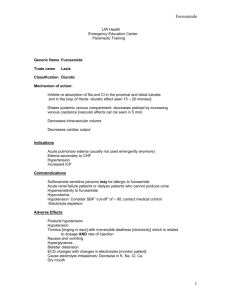
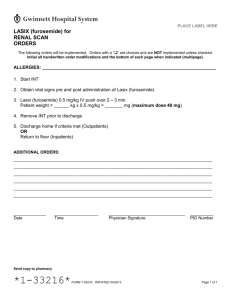
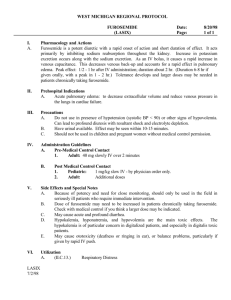
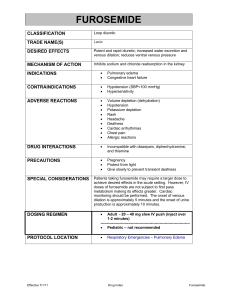
Heart Failure PHARMACIST CARE PLAN By: Dalya Abu Al-Sindyan Lina Darwish Msllam Chief Complaint I’ve been more short of breath lately, I can’t seem to walk as far as I used to, either my feet are growing or my shoes are shrinking. History Of Present Illness (HPI) ▪ Rosemary is a sixty eight years old African-American female, she report that her shortness of breath has been gradually increasing over the past four days and it is particularly worse when she is lying in bed at night and she also reports exertional duspnea that is usual for her and increased swilling in her lower extremities. PMH ▪ Hypertension X 20 years. ▪ CHD with history of MI in 2005. ▪ HF (NYHA FC III). ▪ DM type 2. ▪ Atrial Fibrillation ▪ COPD (Stage 3) Family History ▪ Father died of lung cancer at age 71. ▪ Mother died of MI at age 73. Social History ▪ Alcohol intake. ▪ Low cholesterol and sodium diet. ▪ Former smoker. Medications ▪ Valsartan 160 mg po BID. ▪ Furosemide 40 mg po BID. ▪ Carvedilol 3.125 mg po BID. ▪ Warfarin 2.5 mg po once daily. ▪ Glimepiride 2 mg po once daily. ▪ Potassium chloride 20 mEq po once daily. ▪ Atorvastatin 40 mg po once daily. ▪ Aspirin 81 mg po once daily. ▪ Albuterol MDI, 2 inhalations q 4-6 hours PRN shortness of breath. ▪ Tiotropium DPI 18 mcg /50 mcg, 1 inhalations BID ▪ Pioglitazone 30 mg po once daily. ROS ▪ Seven kg weight gain over the past week. ▪ Worsening shortness of breath. ▪ Orthopnea chronic, dry hacking cough. Physical Examination ▪ GEN: ▪ African-American female in moderate respiratory distress. ▪ VS: ▪ BP 134/76 (Sitting 138/80), HR 65, RR 24, T 37 ºC, O2 sat 90% RA, WT 79 kg. ▪ Skin: ▪ Color pale and diaphoretic. ▪ HEENT: ▪ PERRLA lips mildly cyanotic; dentures. ▪ Nick: ▪ JVD at 30º (7 cm). ▪ Lungs: ▪ Crackles bilaterally. ▪ Echocardiogram: ▪ LVH reduced global left ventricular systolic function, EF 20% ▪ Heart: ▪ Irregularly Irregularl (s3); displaced PMI. ▪ APD: ▪ Soft, myldlu tender, nondistended, (+) HJR. ▪ GENIT/RECT: ▪ Guaiac (-). ▪ MS/EXT: ▪ 3+ pitting pedal edema bilaterally. ▪ NEURO: ▪ A & O x 3, CNs intact. No motor deficts. ▪ ECG: ▪ Atrial fibrillation, LVH. ▪ Chest X-Ray: ▪ pleural effucion, evidence of pulmonary edema. Discussion ▪ Create a list of this patient drug related problems Drug-Drug Interactions Related issue solution Salmetrol with carvediolol B2 agonist with mixed b antagonist worsen dysponea Replace carvediolol with selective cardiotonic nebivolol Warfarin with Aspir May lead to bleeding Give small dose with monitor Pioglitazone Excerbate heart faliure Stop it Signs & Symptoms ▪ What signs symptoms & other information indicate the presence and type of heart failure in this patient? Signs ▪ Shortness of breath for the last 4 days . ▪ Increased swelling in lower extremities. ▪ Exertional dyspnea. ▪ Note: ▪ These are symptoms of Left sided-HF & listed as stage ii /iii HF (NYHA functional classification) or stage C (ACC/AHA(38) Symptoms ▪ HR 65 (irreg irreg), displaced PMI ▪ S3 sound present.(systolic HF) ▪ 3+ pitting pedal edema , Alveolar edema ▪ Decreased pleural effusion. ▪ Skin color pale & diaphoretic. Physical Examination ▪ Labs: BNP greater than 100 pg/mL (776pg/ml). ▪ ECG Atrial fibrillation ,and LV hypertrophy. ▪ Nick: JVD at 30 is a result of right side HF ▪ Lungs bilateral crackles result from CHF. Heart Failure Classification What is the classification of heart failure in this patient ? • stage ii /iii systolic HF (NYHA functional classification) or stage C (ACC/AHA(38)) • Stage I of diastolic HF. • She has acute exacerbation of heart failure with left systolic dysfunction. Patient Problems Causes Could any of this patient problems have been caused by drug therapy ? • Pioglitazone which is 1ST generation sulfonurea tend to exacerbate heart failure (BB C.I) in symptomatic patients & cause edema , weight gain,also glimperide increase CV mortality. • Intake of carvediolol with b2 agonist causes antagonism and worsening of COPD.. Goals For Pharmacologic Management Of HF What are the goals for pharmacologic management of HF in this patient? • Slowing progression of the disease, improving quality of life, and prolonging survival reducing long-term risk for hospitalizations • Alleviating fluid retention, minimizing disability. • Relief symptoms of dyspnea & orthopnea . • Decrease edema & swelling. • Manage acute exacerbation of her HF. Diuretic Therapy What diuretic therapy should be recommended for this patient initially for acute tx of HF exacerbation? • Use the same diuretic she takes furosemide as I.V.: 20-40 mg/dose, may be repeated in 1-2 hours as needed and increased by 20 mg/dose with each succeeding dose up to 1000 mg/day; usual dosing interval: 6-12 hours [ACC/AHA 2010 guidelines ] Pharmacotherapy How should this patient pharmacotherapy be adjusted for chronic management of her systolic heart failure ? • Change B blocker to metoprolol succinate to prevent interaction with b2 agonist • Titrate furosemide oral dose to 80 mg( max 600) • Warfarin dosage should be based on INR (2-3)or prothrombin level • Increase the dose of glimperide after stopping pioglitazone Non Pharmacologic Therapy What non pharmacologic therapy should be recommended for this patient with respect to her HF? • Cha dietary modifications such as sodium and fluid restriction & low cholesterol diet. • Risk factor reduction including stopping alcohol consumption, timely immunizations, and supervised regular physical activity. • Stop alcohol intake as it causes heart poisoning: bed rest & o2 therapy to enhance acute phase. Drug Plan What drugs, doses ,schedules & duration of action are best suited for the management of this patient ? Drug Initial Daily Dose(s) Maximum Dose(s) scaduals Duration of action Metoprolol succinate extended release 12.5 to 25 mg once 200 mg once 24 hr Furosemide 20 to 40 mg once 600 mg or twice valsartan 40 mg twice daily 80 to 160 mg once daily 6 to 8 h Drug Plan What non pharmacologic therapy should be recommended for this patient with respect to her HF? • Continue on Warfarin 2.5 mg PO 1ce/day. • Continue on aspirin 81 mg po once daily. • HTN management associated with heart faliure : • Continue on valsartan 160 mg po BID. • Continue on furosemide 40 mg po BID. • Atrial fibrillation: • Managed by warfarin 2.5 mg & carvedilol 3.125mg (replaced with metoprolol succinate) • Dyslipidemia: • Continue on atorvastatin 40 mg po 1ce daily. Drug Plan • DM Type ii management: • Use insulin glargine 36 U subQ daily • Use insulin lispro 12 U subQ TID with meals. • COPD management : • Continue on albuterol MDI 2 inhalation q 4-6 hr • Continue on tiotropium DPI 18 mcg, 1/day • Continue on fluticasone /salmetrol DPI 250 mcg/50 mcg, 1 inhalation BID. • Hypokalemia : • Continue on pottasium supplements with monitoring specially with furosemide IV. Alternative Plan • Add direct vasodilator as 1st line therapy for her HF b/c it has advantage in African American over ACE-I & ARB’s which c/I in this case due to presence allergy cough edema hyperkalemia & renal impairment : use Isosorbide Dinitrate and hydralazine in comb : BiDil®آ • No need to add digoxin for Afib as it’s managed. • Can’tAdd spirlonlactone as it’s adviced for stage iii HF because crcl Clinical & Laboratory Parameters What clinical & laboratory parameters are needed to evaluate the therapy for achievement of the desired therapeutic outcome and to detect and prevent adverse events? • Initially monitor patient for rapid relief of symptoms related to the chief complaint of orthopnea, dyspnea , oxygenation & fatique. • Monitor for adequate perfusion of vital signs: • asses mental status , Cr Cl , liver function test and a stable HR btw 50-100 HR/min,BP. • Monitor kidney& liver function. • monitor blood glucose • Fluid intake – body weight (daily)- Monitor Adverse Effect Of Drugs What clinical & laboratory parameters are needed to evaluate the therapy for achievement of the desired therapeutic outcome and to detect and prevent adverse events? • Metoprolol succinate: • BP, HR baseline and after Carvedilol 3.125 mg twice 25 mg twice each dose titration, ECG • Furosemide : • monitor electrolyte ,hyperuricemia , nephrotoxicity & autotoxicity. • Valsartan : • Monitor potassium and serum creatinine information should be provided What information should be provided to the patient about medication used to treat her HF ? • Furosemide taking on empty stomach • Digoxin: do not discontinue without consulting prescriber. • Grapefruit juice can increase the blood levels of Atorvastatin. This can increase the risk of side effects such as liver damage Information Should Be Provided What information should be provided to the patient about medication used to treat her HF ? • Furosemide taking on empty stomach • Digoxin: do not discontinue without consulting prescriber. • Grapefruit juice can increase the blood levels of Atorvastatin. This can increase the risk of side effects such as liver damage • Take Metoprolol at the same time each day, preferably with or immediately following meals • Avoid taking potassium rich food. • Glimepiride should be administered with breakfast or the first main meal. PCP Date 8/10 8/10 8/10 8/10 8/10 8/10 Medical proplem HF Tx issue Pharmacotherapy goals Acute exacerbation of Systolic HF Manage symptoms Inadequate drug increase survival & QOL. therapy HTN BP above goal BP<120/80 DM Blood glucose above goal Dyslipidemia Increased lipids Decrease glucose to 100mg/dl Decease LDL & increase HDL. COPD management Atrial fibrillation stable stable Decrease chronich cough & hacking cough,, enhance breathing. Continue to be managed recommendations Start on metoprolol succenate initial 12.5 mg BID Take furosemide Iv 40mg with gradual increment , when stable back to PO 80mg BID Continue on valsartan 160mg po BID Continue on Warfarin 2.5 mg PO 1ce/day. Continue on aspirin 81 mg po1ce Increase furosemide oral dose to 80mg. Continue on valsartan & metoprolol succenate as described above. Stop pioglitazone & increase glimpiride to 8mg Continue on atorvastatin 40 mg po 1ce daily Continue on albuterol MDI 2 inhalation q 4-6 hr Continue on tiotropium DPI 18 mcg, 1/day Continue on fluticasone /salmetrol DPI 250 mcg/50 mcg, 1 inhalation BID. Managed by warfarin 2.5 mg & carvedilol 3.125mg (replaced with metoprolol succinate) Physician action PCP Goals Monitoring parameters Freq HF Electrolytes : Na K Every visit till stidy BNP Every visit SCr Every visit HTN BP HR Every day DM Sugar level Every day Dyslipidemia Weight HDL, LDL,TG Daily Once a week Atrial Fib HR everyday COPD Breathing ,cough everyday Achievements of outcomes comments PCP Goals Monitoring parameters Freq Valsartan : Monitor potassium Every visit and serum creatinine Furosemide : monitor electrolyte(Na/K ,hyperuricemia , nephrotoxicity & autotoxicity Every visit Metoprolol succinate: BP, HR baseline ECG Daily 1ce amonth Achievements of outcomes comments Dalya & Lina Therapy Lab (Tuesday) 09-10-2013