Spongy bone
advertisement

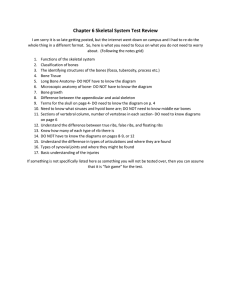
Ch. 7 The Skeletal System Composition • It is a solid network of active tissues surrounded by deposits of minerals. • Components: – – – – Bone Joints Cartilage Ligaments Function of Bones 1. Protection- of soft tissues and organs. 2. Movement – muscles attached to bones= function as levers. 3. Storage – of minerals (Calcium and Phosphorous) and lipids ( yellow marrow) 4. Blood Cell Formation- hematopoiesis- occurs within the marrow of the bone. 5. Support- for the entire body; Individual bones provide a framework for attachment of soft tissues and organs. Bones of the Human Body • The adult skeleton has 206 bones • Two basic types of bone tissue – Compact bone • Homogeneous – Spongy bone • Small needle-like pieces of bone • Many open spaces Classification of Bones Classification of Bones • Long Bones- Relatively long and slender. (Ex: Humerus, tibia, femur, ulna, metacarpals) • Short Bones- Short and cube-shaped: (Ex: carpal bones, tarsal bones) • Flat Bones-thin, flattened, usually curved. (Ex. Cranial bones, ribs, sternum, and bones of the hip and shoulder girdles) • Irregular Bones- vary in shapes, sizes, and surface feature. (Ex:the vertebrae, patella, and a few in the skull) Gross Anatomy of a Long Bone • Diaphysis – Shaft – Composed of compact bone • Epiphysis – Ends of the bone – Composed mostly of spongy bone • Epiphyseal plate (growth plate) – a thin layer of cartilage between the epiphysis – a secondary bone-forming center Gross Anatomy of a Long Bone • Articular cartilage – Covers the ends of bones where they articulate(join) with other bones • Periosteum – Covers bone – Tendons and ligaments attachment • Endosteum – is a thin layer of connective tissue that lines the surface of the bony tissue that forms the medullary cavity of long bones • Medullary cavity – The marrow cavity in the shaft of a long bone Gross Anatomy of a Long Bone • Spongy bone – Inside layer of bone that contains red marrow • Compact bone – Strong, dense layer of bone – Composed of cylinders of mineral crystals (calcium & phosphorus) and protein fibers Types of Bone Cells • Osteocytes – Mature bone cells • Osteoblasts – Bone-forming cells • Osteoclasts – Bone-destroying cells – Break down bone matrix for remodeling and release of calcium • Bone remodeling is a process by both osteoblasts and osteoclasts Bone Tissue Microscopic Anatomy of Bone • Osteon (Haversian System) – A unit of bone • Central (Haversian) canal – Opening in the center of an osteon – Carries blood vessels and nerves • Perforating (Volkman’s) canal – Canal perpendicular to the central canal – Carries blood vessels and nerves Microscopic Anatomy of Bone Microscopic Anatomy of Bone • Canaliculi – Tiny canals that radiate from the central canal to lacunae – Form a transport system Microscopic Anatomy of Bone • Lacunae – Cavities containing bone cells (osteocytes) – Arranged in concentric rings • Lamellae – Rings around the central canal – Sites of lacunae Bone Development and Growth QuickTime™ and a decompressor are needed to see this picture. Bone Development and Growth • Ossification – The process of producing bone from cartilage. Bone Development and Growth • Intramembranous bones originate between sheetlike layers of connective tissue. • Osteoblasts boneforming cells. • Endochondral bones-Long Bones they develop from masses of cartilage shaped like future bony structures. • Epiphyseal plate is the portion of bone where growth happens. Bones continue to grow until the plate closes. • If an Epiphyseal plate is damaged before it ossifies, elongation of the long bone may cease prematurely, or growth maybe uneven. • Babies are born with over 300 bones; many are composed almost entirely of cartilage. • The fontanels of a baby’s skull will fuse around age 2, but growth of the skull continues until adulthood. • Sutures develop and grow throughout childhood at the centers of ossification (growth plates) • Between the ages 18 – 21, all of the cartilage of the epiphyseal plate is replaced by bone. • This is called ossification and the bone lengthening process ends. Bone Homeostasis • Parathyroids regulate the homeostasis of blood calcium • When blood calcium is low Osteoclasts tap into reserves and Bone is “demineralized” Calcium ions is released into blood • Too much calcium in the blood? This hormone causes the deposition of Calcium into the bone matrix by osteoblasts Low Blood Calcium Parathyroid gland releases parathyroid hormone Stimulates osteoclasts to resorb Ca++ Blood calcium rises Feedback Inhibition High Blood Calcium Inhibits parathyroid gland Factors Affecting Bone Development, Growth, and Repair • Deficiency of Vitamin A – retards bone development • Deficiency of Vitamin C – results in fragile bones • Deficiency of Vitamin D – rickets, osteomalacia • Insufficient Growth Hormone – dwarfism • Excessive Growth Hormone – gigantism, acromegaly • Insufficient Thyroid Hormone – delays bone growth • Sex Hormones – promote bone formation; stimulate ossification of epiphyseal plates •Insufficient Sex hormone – Osteoporosis 28 • Physical Stress – stimulates bone growth The Skeletal System • Divided into two divisions – Axial skeleton – Appendicular skeleton Skeletal Organization • Axial Skeleton • 80 bones • head, neck , trunk • lie along longitudinal axis • Appendicular Skeleton • 126 bones • upper & lower limbs • pectoral & pelvic girdle 30 The Skull • 8 Cranial bones – protect brain & house the ear ossicles – muscle attachment for jaw, neck & facial muscles • 14 Facial bones – protect delicate sense organs -- smell, taste, vision – support entrances to digestive and respiratory systems 31 Basic Cranial Bones • Frontal, parietal, occipital, and temporal. – These make up the basic brain case. • Nasal, zygomatic, maxilla, and mandible. – The make up the front of your face, and your jaw. – The ears consist of 6 auditory ossicles – Floating in the throat is the Hyoid bone. Thoracic (Rib) cage • Thoracic is composed of: – 12 pairs of ribs • True ribs—rib pairs 1 through 7 • False ribs—rib pairs 8 through 10 • Floating ribs—rib pairs 11 and 12 – Sternum or breastbone The vertebral column • The vertebral column consists of • Cervical vertebrae (7) – Your neck. • Thoracic vertebrae (12) – Attaches to your ribs. • Lumbar vertebrae (5) – Your lower back. • Sacrum and coccyx – Part of your hip and tail bone. Appendicular skeleton • Appendicular skeleton consists of the – Shoulder girdle (pectoral girdle) – Arms (upper limbs) – Hip girdle (pelvic girdle) – Legs (lower limbs) Pectoral Girdle Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. • Also known as the shoulder girdle • Supports upper limbs •Clavicle (2) • Scapulae (2) Acromial end Sternal end Acromion process Clavicle Head of humerus Coracoid process Sternum Scapula Rib Costal cartilage Humerus Ulna Radius (a) 38 Upper Limbs Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. •Consist of: •Humerus (2) • Radius (2) • Ulna (2) •Carpals • Metacarpals • Phalanges Humerus Humerus Olecranon process Olecranon fossa Head of radius Neck of radius Ulna (c) (54) Radius Ulna Ulna Carpals Metacarpals Phalanges (a) Hand (palm anterior) (b) Hand (palm posterior) (d) d: © Martin Rotker 39 Pelvic Girdle Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. • Coxal Bones (2) • Supports trunk of body • Protects viscera • Forms pelvic cavity Sacral canal Ilium Sacrum Sacral hiatus Coccyx Ischium (b) Pubis Obturator foramen Sacroiliac joint Ilium Sacral promontory Sacrum Acetabulum Pubis Symphysis pubis Pubic tubercle Ischium 40 Pubic arch (a) c: © Martin Rotker (c) Differences Between Male Female Pelves Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. • Female pelvis Flared ilium • Iliac bones more flared Sacral promontory • Broader hips • Pubic arch angle greater •Lighter bones Pelvic brim Symphysis pubis (a) Female pelvis Pubic arch Sacral promontory Sacral curvature 41 (b) Male pelvis Pubic arch Lower Limb Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. • Femur (2) • Patella (2) • Tibia (2) • Fibula (2) • Tarsals • Metatarsals • Phalanges Femur Patella Femur Fibula Tibia (c) Lateral view Patella (52) Fibula Femur Tibia Lateral condyle Medial condyle Fibula Tibia Tarsals Metatarsals (d) Posterior view 42 Phalanges (b) Joint (Articulations) A. Every bone except hyoid (which anchors the tongue) connects to at least one other bone B. Joint types classified by degree of movement 1. Synarthrosis (no movement)—fibrous connective tissue grows between articulating bones (e.g., sutures of skull) 2. Amphiarthrosis (slight movement)—cartilage connects articulating bones (e.g., symphysis pubis) 43 44 Joint (Articulations) B. Joint types 3. Diarthrosis (free movement)—most joints belong this class a. b. c. d. to Structures of freely movable joints—joint capsule and ligaments hold adjoining bones together but permit movement at joint Articular cartilage—covers joint ends of bones and absorbs jolts Synovial membrane—lines joint capsule and secretes lubricating fluid Joint cavity—space between joint ends of bones 45 Joint (Articulations) C. Freely movable joints – – – – – – Ball-and-socket Hinge Pivot Saddle Gliding Condyloid 46 47 48 Skeletal Disorders A. Bone fractures 1. Open (compound) fractures pierce the skin and closed (simple) fractures do not 2. Fracture types include complete and incomplete, linear, transverse and oblique 49 50 How does a broken bone heal? 1. Blood flow increases to the area of the break. This allows nutrients and oxygen to help the healing process. 2. As bone becomes deposited, it grows stronger, and eventually remodels itself. 1. Conversion of blood clot (hematoma) to a soft tissue procallus. Takes 48 hours Loose network of fibers is laid down Inflammatory reaction = swelling = edema Increased blood flow and infiltration by white blood cells Macrophages phagocytize debris Fibroblasts begin repair process by laying down connective tissue Skeletal Disorders B. Joint disorders 1. Noninflammatory joint disorders—do not usually involve inflammation of the synovial membrane; symptoms tend to be local and not systemic a. Osteoarthritis, or degenerative joint disease (DJD) 1) Most common noninflammatory disorder of movable joints— often called “wear and tear” arthritis 2) Symptoms: joint pain, morning stiffness, Bouchard nodes (at proximal interphalangeal joints), Heberden nodes (at distal interphalangeal joints) of the fingers 3) Most common cause for partial and total hip and knee replacements 53 54 Skeletal Disorders • Joint disorders 1. Noninflammatory joint disorders b. Traumatic injury 1) Dislocation or subluxation—articular surfaces of bones in joint are no longer in proper contact 2) Sprain—acute injury to ligaments around joints (e.g., whiplash type injuries) 3) Strain—acute injury to any part of the “musculotendinous unit” (muscle, tendon, junction between the two, and attachments to bone) 55 Skeletal Disorders • Joint disorders 2. Inflammatory joint disorders • Arthritis: general name for several inflammatory joint diseases that may be caused by infection, injury, genetic factors, and autoimmunity • Inflammation of the synovial membrane occurs, often with systemic signs and symptoms 56 Skeletal Disorders – Inflammatory joint disorders: Arthritis a. Rheumatoid arthritis Systemic autoimmune disease—chronic inflammation of synovial membrane with involvement of other tissues such as blood vessels, eyes, heart, and lungs b. Gouty arthritis synovial inflammation caused by gout, a condition in which sodium urate crystals (URIC ACID) form in joints and other tissues c. Infectious arthritis arthritis resulting from infection by a pathogen, as in Lyme arthritis and ehrlichiosis, caused by two different bacteria that are transmitted to humans by tick bites 57 58 Skeletal Disorders C. Tumors of bone and cartilage 1. Osteosarcoma a. b. Most common and serious malignant bone neoplasm Frequent sites include distal femur and proximal tibia and humerus 2. Chondrosarcoma a. b. c. Cancer of skeletal hyaline cartilage Second most common cancer of skeletal tissues Frequent sites include medullary cavity of humerus, femur, ribs, and pelvic bones 59 60 Skeletal Disorders D. Metabolic bone diseases 1. Osteoporosis a. Characterized by loss of calcified bone matrix and reduction in number of trabeculae in spongy bone b. Bones fracture easily, especially in wrists, hips, and vertebrae c. Treatment includes drug therapy, exercise, and dietary supplements of calcium and vitamin D 61 62 Skeletal Disorders • Metabolic bone diseases 2. Rickets and osteomalacia—both diseases characterized by loss of bone minerals related to vitamins a. Rickets – Loss of bone minerals occurs in infants and young children before skeletal maturity – Lack of bone rigidity causes gross skeletal changes (bowing of legs) – Treated with vitamin D 63 64 Skeletal Disorders • Metabolic bone diseases 2. Rickets and osteomalacia b. Osteomalacia – Mineral content is lost from bones that have already matured – Increases susceptibility to fractures – Treated with vitamin D 65 Skeletal Disorders • Metabolic bone diseases 3. Paget disease (osteitis deformans) • Faulty remodeling results in deformed bones that fracture easily • Cause may be genetic or triggered by viral infections 66 67 Skeletal Disorders • Metabolic bone diseases 4. Osteogenesis imperfecta (also called brittle bone disease) • Bones are brittle because of lack of organic matrix • Treatment may include splinting to reduce fracture and drugs that decrease cell activity 68 69 Skeletal Disorders E. Bone infection 1. Osteomyelitis • General term for bacterial (usually staphylococcal) infection of bone • Treatment may involve surgery, drainage of pus, and IV antibiotic treatment—often over prolonged periods 70 71 About Spinal Curvature • At birth your spinal Column is shaped like a C • When baby is about to crawl the cervical region curves towards posterior. • As toddler begins to walk, another curve sets in the lumber area in the same direction…resulting in its characteristic S shape. Spinal Maladies • Kyphosis or Hunchback- When too much thoracic curvature (usually a result of osteoporosis) • Lordosis- Exaggerated Lumbar curvature ( may result from too much weight in pregnancy or obesity) • Scolliosis- A developmental abnormality in thoracic region (abnormal lateral curvature): can be corrected w/ a back brace. • Herniated Disk What do you think happens if you have a “blown disc”? • Your cartilage is located between your vertebrae. • When the tissue surrounding your disc ruptures, it allows your cartilage to move. – “Herniated disc” • This movement can pinch surrounding nerves, causing back pain. Rickets: Vitamin D deficiency in growing children Unable to absorb calcium and phosphate from gut Inorganic bone matrix (mineral salts) lacks calcium Bones deform Gouty Arthritis (GOUT) – Inflammation of joints is caused by a deposition of urate (URIC ACID) crystals from the blood – Can usually be controlled with diet – Hereditary as it runs in families. – This is very painful!! Cartilaginous Joints • Bones connected by cartilage • Examples – Pubic symphysis – Intervertebral joints Figure 5.27d–e Synovial Joints • Articulating bones are separated by a joint cavity • Synovial fluid is found in the joint cavity Figure 5.24f–h The Synovial Joint Figure 5.28 Joseph Merrick • Lived 1862 – 1890 in England • Known as the “Elephant Man” due to his deformities • Thought to be either Proteus Syndrome or Neurofibromatosis • Caused great enlargement of bone and surrounding tissue • Died due to a dislocation of the neck (strain from head weight)