Respiration & Gas Exchange
advertisement

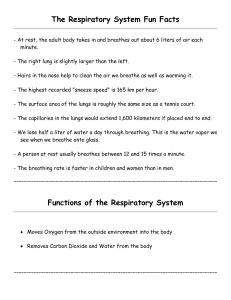
RESPIRATION & GAS EXCHANGE RESPIRATION & GAS EXCHANGE • Respiration - the exchange of oxygen and carbon dioxide between an organism and its external environment. • Respiration in humans can be divided into three steps: 1. Breathing 2. Gas Exchange 3. Cellular Respiration 1. Breathing • Process by which oxygen is taken from the external environment and carbon dioxide is expelled to the external environment. • Involves both inhalation and exhalation. These movements allow the body to take in the oxygen it requires and dispose of carbon dioxide. 2. Gas Exchange • Process of transferring oxygen from the air into the body and transferring carbon dioxide from the blood out of the body. • Takes place at a respiratory surface - a boundary between the external environment and the interior of the body. • Gases cross the respiratory surface by diffusion – the movement of a substance from an area of higher concentration to an area of lower concentration. • Single-celled organisms can exchange gases directly across their cell membrane. • Large animals cannot maintain gas exchange by diffusion across their outer surface. In humans, the respiratory surface is found in specialized structures called lungs. • A respiratory surface is covered with thin, moist epithelial cells that allow oxygen and carbon dioxide to exchange. Those gases can only cross cell membranes when they are dissolved in water or an aqueous solution. Gas Exchange During Respiration Conditions Necessary for Gas Exchange 1. Concentration gradient 2. Large surface area 3. Thin permeable surface 4. Moist exchange surface Gas exchange occurs both externally and internally in humans. • External respiration - the exchange of gases across the respiratory surface between the air sacs (alveoli) in the lungs and the blood. • Lungs to Body • Internal respiration - the exchange of gases between the blood and individual cells in the tissues. • Blood to Body 3. Cellular Respiration • Process in which food (glucose) and oxygen combine chemically to produce carbon dioxide and energy. • Results in the production of ATP, the "energy currency" of the cell. • Every cell in the human body must be able to carry out this necessary life process if that cell is to remain alive. C6H12O6 Glucose + 6O2 6H2O Oxygen Water + 6CO2 + Carbon Dioxide Energy (ATP) OTHER FUNCTIONS OF THE RESPIRATORY SYSTEM • The lungs are internal organs. However, they are constantly exposed to our external environment. With each breath, a host of foreign substances enter our bodies -- pollens, dust, viruses, bacteria, animal dander, tobacco smoke, and other chemicals spewed into our atmosphere by smokestacks and automobile tailpipes. • In addition to gas exchange, the lungs and the other parts of the respiratory system have important functions such as: • Warming or cooling air to proper body temperature • Moisturizing inhaled air for necessary humidity • Protecting the body from harmful substances by coughing, sneezing, filtering or swallowing them, or by alerting the body through the sense of smell • Defending the lungs with: 1.cilia - microscopic hairs along the air passages 2.phlegm (mucous) - a moving carpet of phlegm collects dirt and germs inhaled into the lungs and moves them out to be coughed up or swallowed 3.macrophages - scavenger cells in the lungs that literally eat up dirt and germs invading the lungs THE HUMAN RESPIRATORY SYSTEM Structure Nasal cavity (nose) Uvula Pharynx (throat) Epiglottis Function The preferred entrance for outside air into the respiratory system. The hairs that line the inside wall are part of the air-cleansing system. Piece of soft tissue that hangs down in your pharynx from its top surface and closes over the nasal openings when food is swallowed. Collects incoming air from the nose and passes it downward to the trachea. Flap of tissue that guards the entrance to the trachea, closing when anything is swallowed that should go into the esophagus and stomach. Larynx (voice box) Contains the vocal cords. It is the place where moving air being breathed in and out creates voice sounds. Trachea (windpipe) The passage leading from the pharynx to the lungs. Organ responsible for respiration and is divided into Lungs lobes Each bronchus carries air into the lungs, one to each Bronchi and side. The bronchi continue to branch into smaller bronchioles tubes called bronchioles. Very small air sacs that are the destination of air Alveoli breathed in. Pulmonary capillaries line the walls of the alveoli. As the alveoli inflate and fill with air, oxygen diffuses into Pulmonary capillaries the capillaries and carbon dioxide diffuses from the Pleura Two membranes that surround each lobe of the lungs and separate the lungs from the chest wall. Diaphragm Strong wall of muscle that separates the chest cavity from the abdominal cavity. By moving downward, it creates suction to draw in air and expand the lungs. Ribs Bones supporting and protecting the chest cavity. They move to a limited degree, helping the lungs to expand and contract. Intercostal muscles Muscles lie in between the ribs and control the movement of the ribs. MECHANICS OF BREATHING • Two major actions have to occur to move air into and out of the lungs: • Inhalation – air is pulled into the lungs (breathing in) • Exhalation – air is pushed out of the lungs (breathing out) • These two actions deliver oxygen to the alveoli and remove carbon dioxide. • Ordinary breathing movements are involuntary and occur 12 -16 times per minute. Is It Possible to Voluntarily Control Breathing? • A person can hold their breath, or change the amount of air inhaled, but soon the special sensory receptors begin to send messages to the breathing centre of the brain. • The messages become stronger and stronger due to rising carbon dioxide levels (and increased acidity of the blood). • Eventually a part of your brain (medulla oblongata) sends such severe sensations that you are forced to gasp for air. What Happens When We Breathe? • Two muscles, the diaphragm and intercostal muscles are responsible for breathing. • Diaphragm – large dome-shaped muscle that lies slightly above the waistline and separates the chest cavity from the abdominal cavity. • Intercostal Muscles – are attached to the 12 pairs of ribs. • Movements in the diaphragm and intercostal muscles account for inhalation and exhalation of air. Inspiration or Inhalation of Air • Several events must occur for inspiration to occur: 1. A nerve impulse is sent from the brain to the diaphragm and rib cage muscles. 2. Intercostal muscles move the ribs upward and forward; and the diaphragm contracts and moves down (flattens). 3. This action causes the chest volume to increase. 4. As a result there is a decrease in pressure inside the chest. 5. The pressure outside the body is greater than inside, and air is forced inward into the lungs. Expiration or Exhalation of Air • For air to leave the lungs, the volume of the lungs must decrease. • Breathing out requires only muscle relaxation: 1. Diaphragm relaxes and moves up (curved position) 2. Intercostal muscles move the ribs downward and inward. • These actions decrease the volume and increase the pressure. • The pressure inside the body is greater than outside and air is forced outward from the lungs. • Respiratory System 3D • 3D View of Diaphragm • Lung Expansion DEFENSE MECHANISMS & OTHER INTERESTING THINGS • Coughing is a reflex action in response to irritation of the throat, trachea, lungs or pleural membrane. It can also be caused by nervousness, or it can be voluntary. There is a rapid contraction of the chest and diaphragm muscles causing a sharp intake of air. The epiglottis closes as the chest and diaphragm muscles relax. This causes a build-up of air pressure inside. The epiglottis suddenly opens and the air blows out carrying the irritating particles with it. The main function is to protect the lungs from harmful particles that may be inhaled. • Sneezing is the sudden expulsion of air through the nose. Irritation of the lining of the nasal cavity usually stimulates the sneezing action. The air is taken in by normal breathing and then interrupted. The opening to the mouth is closed off by the soft palate and air is forced out through the nose carrying the irritating particles with it. During a sneeze, the heart stops momentarily. Slow Motion Sneeze Sneezing Panda • Hiccoughing is the result of stimulating the vagus nerve. The impulse is carried to a center in the spinal cord which relays it to the diaphragm. It causes an involuntary contraction of all or part of the diaphragm forcing air out of the lungs. The sudden closing of the epiglottis as air is drawn into the chest produces the sound. Hiccoughs can be caused by eating too fast, drinking too much alcohol, and by irritating diseases of the digestive system, heart, and lungs. • Yawning is a combination of psychological and physical reactions resulting in an involuntary stretching of the mouth accompanied by a large intake of air. The air is then exhaled as the mouth closes. It may be the result of a decrease in breathing rate due to tiredness, boredom, or drug action. Since the body requires more oxygen there is a sudden intake of air in the form of a yawn. Why We Yawn • Snoring is the result of vibrations of the soft palate in the mouth while sleeping. Snoring LUNG CAPACITY • Your body’s needs will determine the amount of air that must be taken in with each breath. • As your body’s needs increases, the volume of air taken in also increases. DIFFERENT AIR VOLUME MEASUREMENTS • Tidal Volume • The amount of air breathed in or breathed out by a person at rest. • About 0.6 L is exchanged during normal breathing. • Inspiratory Reserve Volume • The amount of air that can be forcefully inhaled after normal inhalation • Expiratory Reserve Volume • The amount of air that can be forcibly exhaled after normal exhalation. • Vital Capacity • The maximum amount of air the person can forcibly exhale after the largest possible inhalation of air. • About 4.5 L of air can be forcibly inhaled and exhaled with effort. • Also measured as the sum of three volumes of air vital capacity = tidal volume + inspiratory reserve + expiratory reserve • Residual Capacity • The air that remains in the lungs at all times • Not all air in the lungs is used at once, and no matter how hard one tries to expel the air from the lungs, there will always be some left in the tubes and lung spaces. • Spirometer – measures the volume of air inspired and expired by the lungs. CHEMISTRY OF RESPIRATION • Regulation of Breathing • The ability of the body to adjust and maintain the levels of oxygen and carbon dioxide is a good example of homeostasis (the maintenance of a constant internal environment). • As we studied in the last lesson, breathing movements are controlled by the diaphragm and intercostal muscles. These muscles are stimulated by nerve impulses from the brain. This system of brain, nerves, lungs, and muscles constitutes one of the many negative feedback mechanisms that maintain homeostasis in the human body. • The respiratory center is located in the medulla oblongata of the brain (located at the back of the brain). The medulla is connected to the respiratory muscles (diaphragm and intercostal muscles) by motor neurons. A set of sensory neurons conducts impulses from the lungs to the respiratory center. • During inspiration, the respiratory center sends a nervous impulse to the respiratory muscles that causes them to contract. This inflates the lungs. • The expansion of the lungs initiates impulses in the sensory neurons that extend from the lungs to the brain. • These impulses inhibit the breathing center, which then ceases to send impulses to the respiratory muscles. • No longer stimulated, these muscles relax, and the lungs deflate in an expiration. • The deflated lungs stop stimulating the sensory neurons which then stop sending impulses to the respiratory center of the brain. • No longer inhibited, the respiratory center once again sends out nerve impulses that stimulate the respiratory muscles, and the process repeats. Control of the Breathing Rate • Normal breathing usually supplies enough oxygen to meet the body’s needs and removes carbon dioxide as fast as it is formed. • Occasionally, however, carbon dioxide may begin to accumulate in the blood or oxygen concentration may fall -- two changes that often occur simultaneously. • Either of these conditions increases the rate and/or the depth of breathing. • It should be noted that the body is more sensitive to the carbon dioxide concentration in the blood than to the oxygen concentration. • Breathing rate is mainly controlled by the respiratory center in the brain. • The respiratory centre monitors the carbon dioxide level in the blood. • Oxygen levels are monitored by chemoreceptors in the aorta and the carotid arteries. • When carbon dioxide is dissolved in the blood, it reacts with water to form carbonic acid, which then ionizes to form a bicarbonate ion and a hydrogen ion: CO2 + H2O H2CO3 ----> H2CO3 HCO3- + H+ • As more carbon dioxide enters the blood, the hydrogen ion concentration rises. • The high concentration of hydrogen ions rather than the dissolved carbon dioxide gas stimulates breathing. • The high hydrogen ion concentration in the blood stimulates the respiratory centre in the brain, which then sends impulses to the respiratory muscles and the breathing rate is increased. • Neurons with endings (chemoreceptors) in the aorta and the carotid arteries are sensitive to oxygen concentration. • These neurons monitor the blood continuously, and when the oxygen concentration begins to fall, they also stimulate the respiratory center in the brain. Effects of Environment on Breathing Rate • If you have ever hiked in the high mountains, you have probably noticed how much faster and deeper you breathe at higher elevations than at lower elevations. • That is because there is less oxygen in the air at higher elevations than at lower elevations. You need to take in more air to obtain the same amount of oxygen as at lower elevations • People native to high altitudes have adapted to their environment by having more alveoli and blood vessels in their lungs than people native to low altitudes. • They also have a higher red blood cell count (70% of the blood volume Breathing on Everest 1 instead of the normal 45 to 50%). Breathing on Everest 2 Gas Exchange & Transport • As discussed in the last lesson, the trachea forks into the right and left bronchi, one leading to each lung. • Each bronchus, in treelike manner, branches into smaller tubes, the bronchioles, which divide repeatedly into alveolar ducts. • These ducts end in numerous grapelike clusters, the alveolar sacs, each of which contains several pockets, the alveoli. • Although the alveoli of the lungs are small, they are so numerous (three hundred million per lung) that if they were to be opened up, their total surface area in an adult would be 100 square meters. • This area is approximately the size of a tennis court or 40 times the external body surface area (2 square meters). It is across these 100 square meters of delicate alveolar surface that all our oxygen is absorbed. • A network of capillaries surrounds each alveolus. Their thin walls, like the alveolar walls, are only one cell thick. Thus, the blood passing through the capillaries is separated from the air in the alveolus by only two cells. • At this point, the partnership between the respiratory system and the circulatory system comes into effect. • The respiratory system has brought oxygen molecules to the exchange site in the alveoli. Oxygen will diffuse across the membranes, enter the bloodstream and be transported to the cells and tissues, which require oxygen for their activities. • Carbon dioxide, a waste product of cellular respiration, will diffuse from the body cells into the capillaries and be transported back to alveoli and be exhaled from the body. External Respiration • Gas exchange in an alveolus takes place by diffusion across the moist membrane of the alveolus and the capillary walls. • About 18% to 20% of the air is oxygen, which is a much higher concentration of oxygen than that found in the blood. • Due to these differences in concentration, the oxygen diffuses from the alveoli to the blood in the capillaries. • At the same time, waste carbon dioxide diffuses from the blood into the alveoli due to a higher concentration of carbon dioxide in the blood than in the air in the alveoli. Oxygen Transport • Neither external respiration nor internal respiration could take place without the blood that flows in the circulatory system. • It is the blood that carries the oxygen to the cells of the body and accepts the carbon dioxide from the cells and delivers it to the lungs for exhalation. • Most of the oxygen diffusing into the bloodstream becomes bound to iron-containing hemoglobin molecules within the red blood cells. • Each molecule of hemoglobin is capable of carrying four molecules of oxygen. • An average human red blood cell contains 280 million molecules of hemoglobin. Accordingly, a single red blood cell, with fully saturated hemoglobin molecules, can transport about one billion oxygen molecules. • Only a small fraction (less than 3 percent) of the total oxygen remains freely dissolved in the plasma. The combination of oxygen with hemoglobin allows for the transportation of as much as sixty times the amount oxygen as could be carried if the oxygen were solely in solution in the plasma. • The chemical combination of hemoglobin and oxygen is reversible. • Hemoglobin associates with oxygen in the capillaries of the lungs to form the bright red oxyhemoglobin and dissociates from the union with oxygen in the capillaries of the body tissues to form the dark purplish deoxyhemoglobin. • The amount of oxygen carried by hemoglobin depends upon the concentration (partial pressure) of oxygen. • At the normal concentration of oxygen in the arteries, 97% of the hemoglobin is combined with oxygen. Lungs O2 + Oxygen Hb -------> Hemoglobin HbO2 Oxyhemoglobin Tissues HbO2 Oxyhemoglobin -------> O2 Oxygen + Hb Deoxyhemoglobin CARBON MONOXIDE • Carbon monoxide poisoning is directly related to oxygen transport in the blood. • Carbon monoxide (CO) competes with oxygen for the active sites on the hemoglobin molecules. • Unfortunately, CO combines more readily than oxygen. • As more and more CO molecules combine with hemoglobin, less and less oxygen is carried to the tissues, eventually leading to oxygen starvation and cell death. CO2 Poisoning Carbon Dioxide Transport • Carbon dioxide is carried in the bloodstream in several forms. • About 9% remains in solution in the plasma. A further 27% attaches to vacant carrier sites on hemoglobin molecules that have just emptied their oxygen into the tissues. • About 67% of the carbon dioxide combines with the water in the plasma to form carbonic acid. • As discussed earlier in the lesson, this acid dissociates into bicarbonate ions (HCO3 -) and hydrogen ions (H+). Tissues CO2 + H2O ---------> H2CO3 -------> Carbon Dioxide Water Carbonic Acid HCO3- + Bicarbonate Ion H+ Hydrogen Ion • As you learned in module 1, hydrogen ion concentration lowers the pH of solutions, creating an acidic environment. • This acidic environment can create problems for enzyme function. This is where hemoglobin performs its second function. • The hemoglobin combines with the excess hydrogen ions in the blood, controlling the pH and acting as a buffer to maintain homeostasis. Tissues Lungs Hb + H+ ---------> Deoxy Hydrogen hemoglobin Ion HHb ---------> Hb Buffer + Deoxy hemoglobin H+ Hydrogen Ion The bicarbonate ions are carried back to the lungs in the blood plasma. Once the blood reaches the lungs, the hydrogen ions dislodge from the hemoglobin and join with the bicarbonate ions to form water and carbon dioxide. Lungs HCO3- + H+ Bicarbonate Hydrogen Ion --------> H2CO3 ------------> CO2 + H2O Carbonic Acid Ion Carbon Water Dioxide The carbon dioxide diffuses across the alveolar membranes and is then exhaled. CO2 TRANSPORT REVIEW Carbon dioxide is carried in the bloodstream in three ways. 1. 10% remains dissolved in the plasma. 2. 20% attaches to hemoglobin molecules that just emptied their oxygen into the tissues. 3. 70% of the carbon dioxide combines with the water in the plasma to form carbonic acid. The bicarbonate ions are carried back to the lungs in the blood plasma. Once the blood reaches the lungs, the hydrogen ions dislodge from the hemoglobin and join with the bicarbonate ions to form water and carbon dioxide. • The carbon dioxide diffuses across the alveolar membranes and is then exhaled. DISEASES & DISORDERS OF THE RESPIRATORY SYSTEM • Our lungs are amazing machines that can supply large amounts of oxygen to our blood. Sometimes the lungs don't work as well as they should. This can be because of a disease, allergies, or other inherited conditions. • Over 3 million Canadians must cope with serious respiratory diseases - asthma, emphysema, lung cancer, chronic obstructive pulmonary disease (COPD), influenza, pneumonia, bronchitis, tuberculosis (TB), cystic fibrosis, and respiratory distress syndrome (RDS). These diseases affect people of all ages. While in the past, lung cancer has affected primarily men, the increase in smoking among women in the past 50 years has resulted in the increased incidence and prevalence of this disease among women. LUNG CANCER • Respiratory diseases, including lung cancer, exert a great economic impact on the Canadian health care system. Costs include hospitalization, physician visits and drugs. They also include the less visible or indirect expenses associated with disability and mortality, which may be even more significant. WHAT IS CANCER? • Cancer is a disease in which abnormal cells in some organ or tissue go out of control, growing and increasing in number. Normal cells reproduce themselves throughout life, but in an orderly and controlled manner. Normal growth occurs, worn out tissues are replaced and wounds heal. • When cells grow out of control and form a mass, the mass is called a tumor. Some tumors grow and enlarge only at the site where they began and these are referred to as benign tumors. Other tumors not only enlarge locally but also have the potential to invade and destroy the normal tissue around them and to spread to distant parts of the body. Such tumors are called malignant tumors, or cancer. • Distant spread of a cancer occurs when malignant cells detach themselves from the original (primary) tumor, are carried to other parts of the body through the blood or lymphatic vessels and establish themselves in the new site as an independent (secondary) cancer. A tumor that has spread in this manner is said to have metastasized and the secondary tumor (or tumors) is called a metastasis. SMOKING & LUNG CANCER 1. Smoke inhalation damages the normal cleansing processes by which the lung protects itself from injury. Smoke causes the cilia to disappear so they can no longer do their job of "sweeping" out mucous. The lining then thickens in an attempt to protect the delicate underlying tissues from damage. 2. Cancer-producing agents in the cigarette smoke become trapped in the mucous on the surface lining of the airway long enough to pass into the cells before these substances can be removed by coughing. Coughing is now the only cleansing mechanism which remains. Once within the body, these chemicals, or their products, can alter the nature of the cells slowly and progressively until cancer develops. • The risk of lung cancer depends on how long you've smoked, how many cigarettes are smoked on average and how deep you inhale. • The person at greatest risk is one who has smoked for many years (e.g., over 20 years), who has averaged more than 20 cigarettes per day and who has inhaled freely. For this person the risk may be increased by as much as 15-30 times compared to that of a non-smoker. • Starting smoking early makes it possible for a person to have smoked heavily for at least 20 years by the age of 35. YOU DON’T HAVE TO BE A SMOKER TO GET LUNG CANCER 1. Second Hand Smoke • A series of studies have now shown that non-smoking spouses are at increased risk of lung cancer just from being exposed to the smoke being produced from their partner. Prolonged exposure to the smoke of others, in for example, the working environment, also increases risk, and this increase may apply not only to non-smokers, but to smokers as well. • Particularly at risk are young children, as it has already been demonstrated that children exposed to the smoke of their parents have increased risk of respiratory infection and it has even been suggested that mothers of unborn children exposed to the smoke of others, have a greater frequency of low birth weight infants than mothers not so exposed. Health Canada figures estimate that every year at least 330 non-smokers die from lung cancer due to exposure to second hand smoke. Second Hand Smoke 2. Pollutants • Other forms of inhaled pollutants, particularly repeated industrial exposures, may increase the risk for the smoker, although they can also affect the non-smoker. • Pollutants include the following agents: asbestos, chromium, nickel coal tar products and radon (a radioactive gas). • The risk of developing lung cancer has been increased 50 times for asbestos workers who also smoke in comparison with the risk in the nonsmoking general population. • In comparison the risk for a non-smoking asbestos worker is only 5 times greater than the risk in the non-smoking general population. Both nonsmokers and smokers must therefore avoid work where there is a risk from airborne asbestos. DETECTION & DIAGNOSIS • Regardless of the type of lung cancer, the complaints noted by the patient are very similar. Since the tumor is a foreign object in the airway, a repetitive cough develops in an attempt to dislodge it. • This chronic cough may damage the surface of the tumor so that blood appears in the sputum. In addition, glands are also stimulated by the irritation of the smoke inhalation and produce increased amounts of mucus which must be coughed up. • At a later stage, the growing tumor may also completely obstruct an airway so that infection develops behind this obstruction, resulting in the signs and symptoms of pneumonia. • Usually people with lung cancer complain of increased cough, fever, and sometimes chest pain. • Because the obstruction prevents the effective clearing of secretions from the involved lung, the symptoms persist even if antibiotics bring the infection itself under control. • The development of these complaints demands investigation in the attempt to detect the cancer at the earliest possible moment. DIAGNOSTIC TECHNIQUES • Once cancer is suspected, there are several techniques of investigation that can be pursued. • Sputum can be collected and examined microscopically for the presence of malignant cells which have sloughed from the surface of the tumor. Adequate and careful sampling is required. • Bronchoscopic examination of the airway is sometimes undertaken. In this examination the doctor passes a tube through the mouth or nose into the airways subdivision of each lung. When the obstructing tumor can be seen, a small piece of the tumor can be removed through the bronchoscope for examination under the microscope. Brushings and washings can also be taken from a suspect area for subsequent examination. • Needle biopsy - When the tumor cannot be reached by the bronchoscope and diagnosis has not already been established, a fine needle can be introduced through the chest wall directly into the tumor with xray guidance. A small sample is taken of the tissue and then examined microscopically. • Mediastinoscopy-Since it is essential that the specific nature of the tumor be clearly established before deciding how best to treat it, additional information can be obtained by making a short incision just above the breast bone down to the airway (trachea). A tube is passed through the incision downward alongside the airway to inspect the lymph nodes near the lungs. This procedure is called a mediastioscopy. If abnormalities are noted, biopsies can be obtained for examination. Mediastinoscopy • Computerized Axial Tomography (CAT) Scans are used to help a physician diagnose the presence and extent of any cancer in the lung. During this painless procedure, a narrow x- ray beam is directed by a computer to revolve around the chest area. Within seconds, thousands of bits of information are fed into the computer which converts the data into an image. • And finally, if all other measures have failed to establish a working diagnosis, a small opening can be made in the chest (minithoracotomy) through which the tumor can be directly examined and material obtained for diagnostic purposes. TREATMENT • Once the diagnosis has been established, the decision regarding appropriate treatment must be made. The doctor treats the whole person and not the disease alone. Therefore, the same treatment is not necessarily used for all people with cancer. • Lung cancers are not all alike and patients themselves differ widely in their resistance to the development and spread of the cancer. Some cancers grow and spread rapidly and aggressively whereas others grow slowly, not spreading until very late in the development of the tumor. Similarly, some patients can reject spreading tumor cells and also maintain effective control of the local growth while others cannot. • Therefore, the doctor decides whether the tumor is one which is best treated surgically, by radiation, by the use of drugs (chemotherapy), or by a combination of these measures. • If the tumor is localized so that surgery is advisable, about 30-35 per cent of the people who have lung cancer will be alive and well five years after a successful operation. Radiotherapy is considered a better method of controlling the primary tumor when it cannot be removed completely or when the patient's health indicates that surgery would be inadvisable. • The use of drugs, or chemotherapy, has in the past been used when there is evidence that the tumor has spread to other parts of the body. More recently, chemotherapy has been shown to be particularly helpful in the treatment of the small cell variant of lung cancer and an increase in long term survivals is now being reported following this form of treatment. However, overall, when all people with cancer of the lung are considered, it is obvious that prevention through smoking cessation is the best solution. EMPHYSEMA • Emphysema is a slowly progressing (chronic) destruction of the lungs which makes breathing very hard to do. • Persons with emphysema are, for the most part, males between 50 and 70 years old. Women get emphysema, too, but so far, not as often as men. However these statistics are changing as women are starting to smoke more, and at an earlier age. A very high percentage of the people who have emphysema smoke cigarettes and have been heavy smokers for many years. Frequently, they live in areas where air pollution is a constant problem. • Some people are born with a lack of a substance called alpha-1 antitrypsin. This makes them more likely than others to get emphysema and at an earlier age. HOW IT ATTACKS: • A person with emphysema doesn’t develop the disease suddenly. It comes on gradually. • He or she has probably had several very bad colds each winter for the past few years, each accompanied by a heavy cough, and often with chronic bronchitis. • The cough often persists between colds and becomes chronic. • The symptom that usually brings the patient to the doctor is that he or she has begun to feel short of breath on exertion in morning or evening or both. The patient may think he or she has asthma or heart disease. CAUSES OF EMPHYSEMA • It is believed that emphysema often is a late effect of chronic infection or irritation of the bronchial tubes. • When the bronchi become irritated, some of the airways may be obstructed, trapping air in the lung beyond them. Or the walls of the tiny air spaces may tear, for various reasons. The small blood vessels in the walls disappear. Less contact between blood and air results. • If infection or irritation continues or is repeated for a long time and the stretching and destruction of the walls of the air spaces goes on, the lungs as a whole may become enlarged, at the same time becoming less efficient in exchanging oxygen for carbon dioxide. Enlarged lungs are what give the disease its name, emphysema (which is a Greek word meaning "Inflation"). • Cigarette smoking contributes to the destructive processes that end up as emphysema. TREATMENT • The emphysematous patient must stop smoking to retard progression of the disease. Doctors may prescribe various bronchial dilating medications to treat an asthmatic component that often co-exists with emphysema. Antibiotics are helpful for acute chest infections. Some patients benefit from oxygen therapy, either when exercising or on a nearly continuous basis. • For the few patients suffering alpha-1 antitrypsin deficiency, weekly infusions of alpha-1 antitrypsin are available. These infusions are very expensive and it is not yet known if progress of this rare form of emphysema can be reduced by using this therapy. Physicians may emphasize the importance of regular exercise to maintain physical fitness and even refer a patient with emphysema to a respiratory rehabilitation program. PREVENTION • At this time, doctors do not know how to prevent emphysema. Continuing research is being conducted to find answers to many questions about this disease. But they do know that cigarette smoking is a definite cause, and that cutting out smoking can avoid damage for many who would otherwise develop the disease. Controlling air pollution can also help. • Modern medicine can usually slow down the progress of emphysema if patients are treated early. It is always the doctor’s immediate concern to clear up any infection or irritation of a patient’s respiratory system, because these things set up a possible starting place for emphysema. CHRONIC BRONCHITIS • The bronchi are air passages connecting the windpipe (trachea) with the sacs of the lung (alveoli) where oxygen is taken up by the blood. Bronchitis is an inflammation of the bronchi causing excessive mucous production and swelling of the bronchial walls. • Many people suffer a brief attack of acute bronchitis with fever, coughing and spitting when they have a severe cold. Chronic bronchitis, however, is the term applied when this coughing and spitting continue for months and return each year, generally lasting slightly longer each time. • Undue breathlessness on exertion is eventually noticed, due to obstruction to air flow in the air passages caused by swelling of the bronchial wall and the presence of mucous that cannot be cleared. WHAT CAUSES CHRONIC BRONCHITIS? • Cigarette smoking is the most important cause of chronic bronchitis which rarely occurs in the non-smoker. Environmental pollution may contribute to the development of chronic bronchitis. • Some smokers are resistant to the development of chronic bronchitis, but as yet there is no way of predicting which smokers will not develop chronic bronchitis. • The decreased incidence of chronic bronchitis among women probably reflects the difference in smoking habits between the sexes. As these differences have diminished we are seeing an increasing incidence of chronic bronchitis in women. • Chest infections seem to occur more frequently in patients with chronic bronchitis. • Inhaled tobacco products impair the ability of the lungs to combat infections. • The excessive mucus associated with chronic bronchitis is ideal for bacteria to breed. WHAT DOES CHRONIC BRONCHITIS FEEL LIKE? • Initially, it begins as a "smoker’s cough" - the expectoration of small amounts of phlegm each morning. It is usually worse in the winter time and when the person has a head cold. In these early phases of chronic bronchitis, the person may lead an entirely normal life, including vigorous sports. Sensitive breathing tests, however, can indicate the beginning of irreversible damage to the lung even at this stage. • The cough becomes more frequent during the day time and even at night, disturbing sleep. The patient then notices that activities previously tolerated well, cause shortness of breath and perhaps some wheezing. As the disease progresses, shortness of breath may be caused by very ordinary activities such as getting dressed in the morning or having a bath. • The patient with advanced bronchitis may be unable to walk or climb stairs without supplemental oxygen. He or she may be confined to a chair or bed because of shortness of breath and the type of heart failure which may develop in the late stages of this disease. Minor chest infections in patients with severe chronic bronchitis may require intensive treatment in hospital. As the disease is not rapidly fatal, it becomes an important cause of disability and the annual cost of this disease in terms of time lost from work, disability pensions and medical therapy may approach one hundred million dollars annually in Canada. TREATMENT • The best treatment for chronic bronchitis is prevention which means no smoking. • Once chronic bronchitis is established, smoking cessation does not cure the disease. The cough of chronic bronchitis will diminish within weeks of smoking cessation and usually disappears entirely within three months. • Obstruction to air flow caused by swelling of the walls of the bronchi persists, although medications to dilate the bronchi (bronchodilators) may diminish the breathlessness. • The important point to remember is that patients with chronic bronchitis who continue to smoke continue to deteriorate relatively rapidly. Smoking cessation will stop this rapid deterioration and there may actually be a slight improvement in the ability to lead a normal life. • Many physicians prescribe antibiotics for acute chest infections which may shorten their duration and help prevent pneumonia. Annual vaccinations against influenza and a once only vaccination against bacterial pneumococcal pneumonia may help prevent the pulmonary complication of infections in chronic bronchitis. • The sufferer from chronic bronchitis should avoid excessive dust and fumes although under normal circumstances, the contribution of atmospheric pollution to chronic bronchitis is extremely small. • Regular exercise is even more important for patients suffering from chronic bronchitis than for healthy people. Exercise does not improve the ability of the lungs to take up oxygen, but the effects of physical fitness on the cardiovascular system will compensate somewhat for the impaired lung function. • The result of physical fitness in the patient suffering from chronic bronchitis is a lessening in breathlessness on exercise. Chronic bronchitis is basically a preventable disease being rare in the nonsmoker. It is never too late to stop smoking. The patient with chronic bronchitis can be treated with better results in the early stages of the disease. ASTHMA • Asthma is a chronic lung condition. It is characterized by difficulty in breathing. People with asthma have extra sensitive or hyperresponsive airways. • The airways react by narrowing or obstructing when they become irritate. • This makes it difficult for the air to move in an out. This narrowing or obstruction can cause one or a combination of wheezing, coughing, shortness of breath, chest tightness. • This narrowing or obstruction is caused by airway inflammation (meaning that the airways in the lungs become red, swollen and narrow) and bronchoconstriction (meaning that the muscles that encircle the airways tighten or go into spasm). TRIGGERS • Triggers irritate the airways and result in bronchoconstriction although they do not cause inflammation and therefore do not cause asthma. The symptoms and bronchoconstriction caused by triggers tend to be immediate, short-lived, and rapidly reversible. The airways will react more quickly to triggers if inflammation is already present in the airways. • Common triggers of bronchoconstriction include everyday stimuli such as cold air, dust, strong fumes, exercise, inhaled irritants, emotional upsets, and smoke. • Smoke acts as a very strong trigger. Second-hand smoke has been shown to aggravate asthma symptoms, especially in children. The effects of one cigarette linger in the home for 7 days, and therefore it is very important to provide a smokefree home for all children. Stop Smoking CAUSES OR INDUCERS • In contrast to triggers, inducers cause both airway inflammation and airway hyper-responsiveness and are recognized as causes of asthma. Inducers result in symptoms which may last longer, are delayed and less easily reversible than those caused by triggers. The most common inducers are allergens and respiratory viral infections. ALLERGENS • Inhalant allergens are the most important inducer or cause of inflammation and airway hyper-responsiveness. Probably 75-80% of young asthmatics are allergic. The most common inhaled allergens include pollen (grasses, trees and weeds), animal secretions (cats and horses tend to be to the most allergen causing), molds, and house dust mites. • Exposure to an allergen (e.g. cat secretions) may cause immediate symptoms such as wheeze or cough. This occurs because airways are hyper-responsive and react by tightening. These symptoms can easily be relieved by a bronchodilator (such as Ventolin®). However, about 4 and 7-8 hours after exposure to the secretion, a late response occurs which is caused by the inflammation. This inflammation develops over time. Because of the late response, it is often difficult for the patient and physician to identify what is actually causing the asthma. RESPIRATORY VIRAL INFECTIONS • In children, respiratory viral infections may cause deterioration in his or her asthma. A respiratory viral infection is probably one of the most common causes of asthma. • In some cases, the influenza vaccine is indicated. This may help to prevent respiratory complications that can occur from developing influenza. This vaccine is contraindicated for those individuals who have an allergy to eggs.