TB Infection Control: Engineering Controls
advertisement
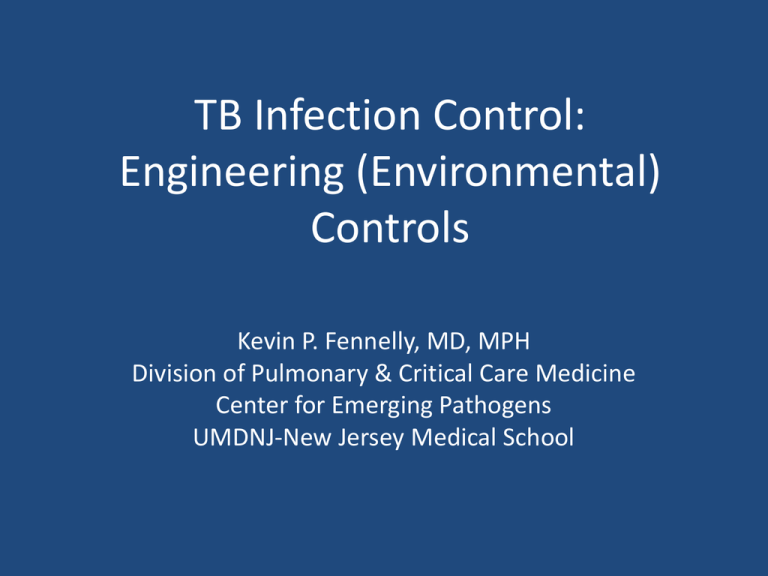
TB Infection Control:
Engineering (Environmental)
Controls
Kevin P. Fennelly, MD, MPH
Division of Pulmonary & Critical Care Medicine
Center for Emerging Pathogens
UMDNJ-New Jersey Medical School
Objectives
• To review fundamental principles and
practices of TB infection control related to
engineering controls
• To discuss advantages and limitations to
different engineering control measures.
• To discuss how engineering controls are used
in the total TB Infection Control Plan.
• To discuss issues and questions specific to
your experiences in Chiapas.
Key Points
• Engineering controls (EC) are the 2nd priority in
control measures AFTER administrative controls,
• But they are complementary
• Dilution ventilation is the most important EC
– Protects HCWs, other patients, visitors
– Has limits defined by technology, expense, comfort
• Negative pressure or directional airfllow keeps
contaminated air away from HCWs
• UVGI and filtration devices are adjuncts or backups for high-risk areas
– Require maintenance
– Need to consider cost-effectiveness
Fundamentals of Infection Control
• Administrative controls: reduce risk of
exposure
• Environmental controls: prevent spread
and reduce concentration of droplet nuclei
• Respiratory protection controls: further
reduce risk of exposure to wearer only
Hierarchy of Infection Control
Administrative Controls
Environmental Controls
Respiratory Protection
Hierarchy of Infection Controls
TB-Infection Controls: Simplified
• Administrative: WHO?
– Who is a TB suspect?
– Who is at risk from exposure?
– Who has infectious TB?
– Who has drug resistant TB?
• Environmental: WHERE?
– Where is optimal place to minimize risk?
• Personal Respiratory Protection: Special high
risk settings
Environmental Controls
• Control source of infection
• Dilute and remove contaminated air
• Control airflow
– Keep infectious air moving outside
– Keep HCWs ‘upwind’ , infectious patients
‘downwind’
Airborne Infection Isolation Room
Policies
• Environmental factors and entry of visitors and
HCWs should be controlled
• Air changes per hour (ACH) (volume /time)
– >6 ACH (existing)
– >12 ACH (new)
• Minimum of 2 ACH of outdoor air
• HCWs should wear at least N95 respirators
What is ventilation?
• Movement of air
• “Pushing” and/or “pulling” of particles and
vapors
• Preferably in a controlled manner
10
Ventilation control
• Types of ventilation
– Natural
– Local
– General
11
Local exhaust ventilation
• Source capture
– Exterior hoods
– Enclosing hoods
Uganda
Examples of General Ventilation
• Single pass
– First choice
•
Recirculating
– HEPA filtration
Room Air Mixing
and Air Flow
• Prevent air stagnation
• Prevent short
circuiting
• Air direction
• Air temperature
• Space configuration
• Movement
14
Facility Airflow Direction
• Clean to less clean
• Negative pressure
Facility Airflow Direction
• Clean to less clean
• Negative pressure
ronchoscopy
Brazil
17
18
- Escombe AR et al. Plos Med 2007 ; 4: e68
- Escombe AR et al. Plos Med 2007 ; 4: e68
Natural vs Mechanical Ventilation
• Good natural ventilation is better than bad
mechanical ventilation.
• Major limitation of natural ventilation is that it
depends upon outdoor weather conditions.
• Can control odor and improve comfort of
occupants , but not if very cold or very hot.
• Usually we do not have a choice and must
work with where we are!
Limitations of Ventilation
HEPA filtration
Must be used
– When discharging air from local exhaust
ventilation booths or enclosures directly into
the surrounding room, and
– When discharging air from an AII room into the
general ventilation system
24
Room Air Cleaners
25
TB Outpatient unit – Helio Fraga Institute, MoH, Rio de Janeiro
26
Evaluation of Room Air Cleaners
Colony Forming Units (CFUs)
1,000
Position 1
Position 2
Position 3
Position 4
Position 5
Position 6
Position 7
Position 8
Position 9
100
10
Off
Linear
On
1
0
2
4
6
8
10
Elapsed Time (hours)
27
Ultraviolet Germicidal
Irradition (UVGI)
• Used as supplement or back-up to dilution
ventilation
• Does NOT provide negative pressure
• Requires maintenance, esp. cleaning bulbs
• Not effective at high humidity (>70%)
• Occupational exposure limits: eye & skin
28
29
Xu P et al. Atmospheric Environment 2003; 37:405
31
- Escombe AR et al. Plos Med 2009 (March) ; 6
Escombe AR et al. Plos Med
2009 (March) ; 6
Environmental Controls:
Which one and When?
• Dilution ventilation, UVGI, and HEPA filter
units are all effective under IDEAL laboratory
conditions
• Best data in field support dilution ventilation
• Advantage of ventilation is usually ‘always on’,
minimizing human errors.
• Disadvantages of UVGI and HEPAs
– Maintenance (increased human errors)
– Large variability of effectiveness
– May cause false sense of reassurance
Control Measures are Synergistic & Complementary
Assumptions: Homogenous distribution of infectious
aerosol over 10 hours; uniform susceptibility.
- Fennelly KP & Nardell EA. Infect Control Hosp Epidemiol 1998; 19;754
Wells-Riley Equation:
Mathematical model of airborne infection
Pr{infection}=C/S=1-e(-Iqpt/Q)
Where
C=# S infected
S=# susceptibles exposed
I = # infectors (# active pulm TB cases)
q = # infectious units produced/hr/Infector
p = pulm ventilation rate/hr/S
t = hours of exposure
Q = room ventilation rate with fresh air
Admin
E.C.
x
x
x
x
x
x
Risk of Close Exposure?
Infectious
Case
HCW
Summary – TBIC Engineering Controls
• First priority is ADMINISTRATIVE controls, but EC
are complementary
• Dilution ventilation is most important for all
– Can add to comfort
– But limited by technology, comfort, expense
• Negative pressure or directional airflow can keep
infected air away (even if diluted) from HCWs
• UVGI and filtration devices are adjuncts for high
risk areas
– Back-up when not possible to ventilate well