Shigellosis
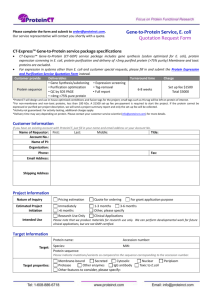
advertisement

ENVR 133 Bacterial Pathogens Overview
Mark D. Sobsey
Some Important Enteric Bacterial Pathogens and Their Sources
Bacterium/Group
Salmonella spp.
(except S. typhi)
Campylobacter spp.
Escherichia coli
Helicobacter pylori
Aeromonas hydrophila
Yersinia enterocolitica
Listeria monocytogenes
Vibrio cholerae
some other Vibrio sp.
Shigella spp.
Animal Feces
yes
no
yes
yes
unknown
yes
yes
yes
yes
no
Non-fecal sources
no
no
yes
no
unknown
yes
yes
yes
yes
no
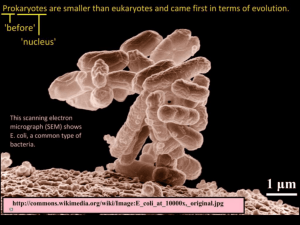
Typical Procaryotic Cell
Gram Negative Outer Cell Membrane and
Lipopolysaccharide Structure
Structure of a Gram-Negative Cell Wall
Porins
• Porins are structures in the outer
membranes of Gram-negative
bacteria
• They allow diffusion of low
molecular weight compounds into
the periplasmic space.
• Function as channels for small
hydrophilic molecules.
• Porins are beta-barrel proteins in
the outer membranes.
• Porins occur as trimers in the
membrane.
• In E. coli, porins with different
specificities exist, e.g.. maltoporin
and phosphoporin.
Shigellosis - Illness
• Persistent diarrhea with frequent and painful passage of
stools consisting mostly of blood, mucus and pus
– accompanied by fever and stomach cramps.
• Blood and mucus in stools are likely signs of shigellosis
• Shigella infect, invade cells lining the large intestine (colon)
• Cause breaks (ulcers) in mucous membrane lining of intestine
– Inflammation and tissue damage
– Causes painful straining to pass stools; can lead to rectal
prolapse
– Ulcers commonly in the rectum
– results in increased production of mucus
– loss of blood and serum proteins into intestinal cavity
• Causes the symptoms of dysentery, which include blood and
mucus in the stool (bloody diarrhea); fever is also common
Shigella and Shigellosis
• Fecal-oral transmission
– person-to-person, fomites, food, water, ect.
•
•
•
•
•
Waterborne and water-washed
Reservoirs: humans and primates
Infectious dose: low; as few as 10 cells to infect
Incubation period: 1 to 7 days; typically, 1-3 days
Duration of illness:
– untreated: severe symptoms for about two weeks
– Antibiotic treatment shortens illness and prevent spread
to others
Shigellosis - Epidemiology
• Four species of Shigella: flexneri, sonnei, dysenteriae, boydii
• Major public health problem in many developing countries
– causes about 5 to I0% of childhood diarrhoea
– up to 25% of all diarrhea-related deaths can be associated with Shigella
Developing countries:
• Sh. flexneri is endemic (always present) in most communities
• Sh. dysenteriae type 1 often occurs in an epidemic pattern
– organism can be absent for a number of years, then reappear and infect a
large proportion of the population.
• These two species of Shigella generally produce the most
severe illness.
Developed countries:
• Sh. sonnei is the most common and is the least virulent
• Sh. boydii causes disease of intermediate severity
– is least common, except in the Indian sub-continent.
Shigellosis - Epidemiology
•
•
•
•
•
Worldwide distribution; infections occur throughout year
Mostly in children aged under five
Rates of infection are highest where sanitation is poor
As few as 10 cell can initiate infection
Transmission influenced by:
– nutritional status
– environmental factors affecting transmission:
• rainfall and temperature
• Waterwashed as well as waterborne
• Incidence highest in dryer climates in hot and dry weather
– Scarcity of water may limits handwashing and other hygiene
measures that reduce transfer of the very small number of
bacteria needed to cause infection
• Incidence in wet climates is often highest in rainy season
Shigellosis - Complications
• severe anorexia (loss of appetite)
• hypoproteinaemia (a low concentration of blood
protein)
• hyponatraemia (a low concentration of blood sodium)
• dilation of the large intestine
• seizures
• anaemia
• kidney damage
• persistent diarrhoea
• weight loss and malnutrition
Shigellosis - Treatment, Control and Prevention
Treatment:
• Continue to eat (feed)
– to prevent weight loss and hypoglycemia
• include foods rich in potassium (bananas)
• Replace fluids
– Oral or IV rehydration with fluids and electrolytes
• Treat with antibiotics:
– trimethoprim/ sulfamethoxazole
– ampicillin
Prevention and Control:
• Handwashing, especially after defacation
• Improved sanitation and hygiene
– improve water, waste treatment/disposal and food sanitation
– reduce overcrowding, etc.
• No effective vaccine
Escherichia - Taxonomy and Biochemistry
Five accepted species:
• E. coli, E. blattae, E. fergusonii, E. hermanii and E. vuneris
Can be differentiated on the basis of the following reactions:
• Indole, citrate, lysine decarboxylase, growth in KCN and
malonate utilization
Biochemistry:
• frequently produce indole (except E. blattae and E.vulneris)
• ferment glucose by mixed acid fermentation
• do not produce H2S, phenylalaninedeaminase or urease, do not
utilize citrate as sole carbon source (except some strains of E.
blattae , and E. fergusonii. )
• Most are motile, ferment a variety of carbohydrates and
decarboxylae arginine, lysine and/or ornithine.
E. coli Genetics and Serology
Genetics:
• Single, circular DNA molecule, ~4 x 106 base pairs
• Molecular weight of 4 x 109
• Total length of about 1.4mm.
• Two strains completely sequenced and genomic
organization is now being characterized
– many of the genes have been mapped.
Serology:
• E. coli can be subdivided by somatic (cell-wall) or O
antigens and flagellar or H antigens.
– >160 recognized O types and 55 recognized H types
– over 8000 possible OH serotypes.
– also capsular (K) and fimbrial antigens.
Virulence Properties of E. coli
Enterotoxins:
• at least two types: Heat Stable (ST) and Heat Labile (LT)
• Verotoxins or Shiga-like toxins (interchangeable terms):
– Verotoxin term is based on the reactions of toxins on Vero cells
– at least two families of these toxins:
• VT1 (SLT I): similar to Siga-toxin (produced by some strains of
Shigella dysenteriae)
• VT2 (SLT II) which is only about 50% realted Shiga toxin.
• Other Toxins:
– Cytolethal distending toxin (CLDT), VirCytotoxin, Cytotoxic necrotising
factors (CNF), a possible Enteropathogenic E. coli EPEC) enterotoxin and
a possible E. coli Sudden Infant Death Syndrome (SIDS)-toxin.
• Haemolysins:
– extracellular haemolysin known as alpha-haemolysin (many strains)
– cell-associated haemolysin, beta-haemolysin, (some strains)
– enterohaemolysin: extracellular; Enterohaemorrhagic E. coli (EHEC)
Virulence Properties of E. coli
• Fimbriae: CFAI/CFAII, Type 1 fimbriae, P fimbriae, S fimbriae
– most important: K88, K99 and CFA fimbriae associated with
enterotoxigenic E. coli (ETEC). They have differing species
specificities.
– The p-fimbriae: associated with urinary tract pathogens.
– E. coli also produce common fimbriae not associated with
virulence.
• Adhesins:
– Intimin: non-fimbrial adhesin; causes the intimate association
with target cells in enteropathogenic and
enterohaemorrhagic E. coli .
• Associated with the 'attachment and effacement' phenomenon
• Causes destruction of the intestinal surface cells.
• Other outer membrane proteins can act as adhesins.
Iron and E. coli virulence
Enterobactin (Enterochelin)
• A siderophore: low-molecular weight, high-affinity iron-binding
compounds
• In vitro conditions are iron-limitated; E. coli produces the
phenolate iron chelator enterobactin, which is also known as
enterochelin.
• cyclic triester of 2,3-dihydroxy-N-benzoyl-L-serine and removes
iron from iron-binding proteins and transports it into the bacterial
cell..
• Seven chromosomal genes needed to synthesise enterobactin
• Used once, because the molecule is cleaved within the E. coli cell
and the remnants discarded for the iron to become available. It is
thus a very energy expensive process.
Iron and E. coli virulence
Aerobactin
• Another siderophore
• plasmid mediated
• associated with virulence in E. coli causing extraintestinal
infections.
• A conjugate of 6-(N-acetyl-N-hydroxylamine)-2-aminohexanoic
acid and citric acid.
• Forms an octahedral complex with ferric iron.
• Can be recycled (unlike enterobactin)
• Not bound by serum albumin.
Iron and E. coli virulence
Non-native Siderophore Use by E. coli:
• fungal siderophores such as ferrichrome
• coprogen rhodotorulic acid
• citrate (inefficient)
Outer Membrane Proteins (OMP)
• For iron-loaded siderophores to be adsorbed on the cell surface
• Also function as bacteriophage and/or colicin receptors.
• Other proteins needed by these receptors to move iron into cells.
– act as 'gated porins'
Iron from Heme Compounds
• E. coli takes up iron from haemoglobin preferentially to by
siderophores,
• E. coli hemolysins may help make heme and hemoglobin iron
available.
Pathogenic E. coli
Enteric Infections:
•
•
•
•
•
•
Enteroadherent E. coli (EAEC)
Enteroaggregative E. coli (EAggEC)
Enterohaemorrhagic E. coli (EHEC)
Enteroinvasive E.coli (EIEC)
Enteropathogenic E. coli (EPEC)
Enterotoxigenic E. coli (ETEC)
Extraintestinal Infections:
• Uropathogenic E. coli (UPEC): urinary tract infections
• Neonatal Menigitis E. coli (NMEC).
Enterohemorrhagic E. coli
Harbor genes for one or more of the virulence attributes known
to associated with the EHEC.
• shiga toxin(s)
• adherence factor(s)
• enterohaemolysin
• somatic antigens characteristic of many EHEC serogroups,
such as O111 or O157.
• An E. coli must cell carry a sufficient number of such genes
to cause disease.
• Magnitude of exposure or size of infectious dose is also
important.
– Dose is very small in comparison with those for most other
enteric pathogens; a few bacteria per dose may cause
infection and illness
Enteropathogenic E. coli
• Cause infantile gastroenteritis.
• Certain serotypes are associated with infantile diarrhea.
– Infantile gastroenteritis with dehydration is an important problem.
• Serogroups O26, O55, O111, O119, O125, O126, O127, and O128
are most commonly isolated.
• EPEC have declined in the developed world as major causes of
infantile diarrhea, but remaining very important in the developing
world.
• EPEC adhere to the intestinal mucosa to produce a characteristic
"attaching and effacing" lesion in the brush border microvillous
membrane.
• EPEC trains belonging to serogroups O26, O111 and O128 have
recently emerged as enterohaemorrhagic E. coli (EHEC).
Enterotoxigenic E. coli
• Major cause of travellers' diarrhea (Montezuma’s revenge,
Delhi belly, Aztec two-step, etc.) and of diarrhea in children
in the developing world
• Produce an enterotoxin similar to cholera toxin.
– They are involved with a condition known as "Non-Vibrio cholerae
cholera-like diarrhoea".
• Produce one or both of two enterotoxins:
–
–
–
–
heat stable enterotoxin (ST) : survives boiling for 30 minures
heat labile enterotoxin (LT): does not survive such boiling
LT response is sensitive to acid pH; ST was not.
LT is closely related to choleragen (CT) the enterotoxin of V.
cholerae.
• Most ETEC isolated from humans produce colonization
factor antigens which are human specific fimbrial antigens
– also a common cause of diarrhea in young animals.
Enteroinvasive E. coli (EIEC)
• Cause positive reaction in the Sereny test (ability to cause
keratoconjunctivitis in guinea pig eyes).
– a characteristic shared with strains of Shigella
• By DNA probes the invasiveness plasmids of both E. coli and
Shigella are identical.
– 120-140 mD invasiveness plasmids encode all the genes
necessary for the virulence of the EIEC.
• Many EHEC are non-motile and anaerogenic.
• Account for only a small proportion of diarrhea in non-tropical
countries
– but, cause high proportions of illness and death, mostly in
warmer seasons
• Also important causes of dysentery-like diarrhea in tropical
countries.
Enteroahherent E. coli (EAEC)
• Different patterns of adherence to cultured epithelial
cells.
• Localized adherent E. coli (LAEC) by some serotypes
– form adherent microcolonies on HEp-2 cells
– associated with acute, non-bloody diarrhoea in
children.
• Diffusely adhering E. coli (DAEC)
– a cause of diarrhea in some studies
Enteroaggregative E. coli (EAggEC)
• 3rd type of adherence: enteroaggregative adherence
• Bacteria align in parallel rows to cells or glass ('stacked
brick-like’).
• persistent childhood diarrhoea in South America and India
• Illness lasts >14 days.
• Produce a heat-labile toxin antigenically related hemolysin
but not hemolytic
• Produce plasmid encoded heat stable toxin (EAST1)
unrelated to the heat stable enterotoxin of ETEC.
• Form a distinct “scum” on the surface of Mueller-Hinton
broth
– possibly use as a rapid screening method for EAggEC.
Uropathogenic E. coli (UPEC)
•
•
•
•
Common cause of urinary tract infections (UTI).
Severity: from asymtomatic to bacteriuria, cystitis and pyelonephritis.
Women more frequently affected than men.
Same serotypes are found in feces and urine of patients, but, UPEC
have virulence factors which enhance their ability to cause infection.
• Only some O groups cause UTI: O1, O2, O4, O6, O7, O18 and O75.
• Only some K antigens (K1, K2, K3, K5, K12 and K13) cause UPEC.
• Certain pili (fimbrae), the p-pili, are an important virulence factor
– bind to the P-antigen, a blood grouping antigen
– bind more to uroepithelial cells of persons with the P or P2 phenotype
– other adhesins may also be involved.
• Production of alpha-haemolysin by UPEC
• Production of aerobactin
• Several virulence enhance an E. coli's ability to cause UTI
– an infecting strain may only express some of them to cause infection.
Neonatal Meningitis E. coli (NMEC)
• Neonatal menigitis in about 1/2500 live births.
• Up to 80% of cases of neonatal menigitis are due to E. coli.
• ~80% of the isolates possess the K1 capsular antigen.
– a 2.8 a-linked homopolymer of N-acetylneuraminic acid (sialic acid)
– chemically and immunologically identical to the group B acidic
polysaccharide of Neisseria menigitidis.
– masks the underlying structures of the bacterial cell surface, preventing
specific antibody responses and the activation of the alternate complement
system from being activated.\
– poor immunogen, maybe due to it resembling extracellular matrix proteins.
– may also reduce the serum sensitivity of E. coli.
– serotypes isolated from meningitis cases often found in maternal faeces;
source; infection occurs at birth.
• Reasons for susceptibility of neonates to NMEC is not known.
Salmonella and Salmonellosis
• Belong to Enterobacteriaceae family
• Gram-negative bacilli; facultative and flagellated (motile).
• 3 major antigens:
– "H" or flagellar antigen (phase 1 & 2)
– "O" or somatic antigen (part of the LPS moiety)
– "Vi" or capsular antigen (called "K" in other
Enterobacteriaceae).
• Posess LPS endotoxin characteristic of Gram-negative bacteria
– composed of an "O” polysaccharide ("O" antigen)
– "R" core
– endotoxic inner "Lipid A".
– Endotoxins evoke fever and can activate complement, kinin
and clotting factors.
Salmonella Illness
Gastroenteritis or salmonellosis
• contaminated food or water. Most commonly,
• often from contaminated poultry (turkeys and chickens).
• S. enteritidis or S. choleraesuis: most commonly isolated
species
Enteric fever:
• transmitted from person to person and involves
• S. typhi (no animal reservoirs)
• reservoirs:
– Contaminated food or water with human feces
– asymptomatic human carriers
Salmonella enteritidis
Salmonella typhi
Salmonella typhimurium DT 104
• A commonly reported phage type of S. typhimurium
• Resistant to many antibiotics: ampicillin, chloramphenicol,
streptomycin, sulphonamides, and tetracyclines.
– also some additionally resistant to trimethoprim and to
quinolone antibiotics such as ciprofloxacin
• Antibiotic resistance emerged as a result of widespread use
both prophylactically and therapeutically.
– effective antibiotics to control its spread is severely limited.
•
•
•
•
Associated with cattle, pigs and chickens and other animals.
May infect animals without showing any signs of illness.
Spreads from farm to farm by raw water and other sources
Once a farm becomes contaminated it is hard to eradicate;
– it survives in dry as well as in wet environments
• Illness from S. typhimurium DT 104 is more difficult to treat than
illness from other salmonellae; also has a higher mortality rate.
Campylobacters
•
•
•
•
Gram-negative
Curved rod
about 1.5-3 microns
motile via polar
flagella
• Microaerophilic
• Prefer high CO2
Campylobacters
• Due to Campylobacter jejuni or sometimes C. coli.
• Normal intestinal flora of many warm-blooded animals
– chickens and turkeys; also in raw water and raw milk.
– Illness in sheep (abortion), dogs and cats (gastroenteritis)
• Causes illness in humans
– Cause 5-11% of all diarrhea cases in the United States.
• Symptoms: from mild to severe:
– bloody diarrhoea is the most characteristic symptom)
– also fever, nausea, abdominal cramps and (seldom) vomiting
– duration of illness usually 2-10 days
• abdominal cramps, may recur for up to 3 months after infection
– Complications such as septicaemia, may arise.
• The infectious dose may be very low, i.e. 100s of cells
• Infants, young children and debilitated people at highest risk
Complications and Sequelae of
Campylobacteriosis; Guillain-Barre Syndrome
• Develop a rare disease of the nervous system beginning
several weeks after the diarrheal illness.
• Called Guillain-Barré syndrome
• Person's immune system is "triggered" to attack the body's
own nerves
• can lead to paralysis lasting several weeks; usually requires
intensive care
• About 1 per 1000 reported campylobacteriosis cases leads to
Guillain-Barré syndrome.
• Perhaps 40% of Guillain-Barré syndrome cases in this
country may be triggered by campylobacteriosis.