Urinary System, Day 2 (Professor Powerpoint)
advertisement

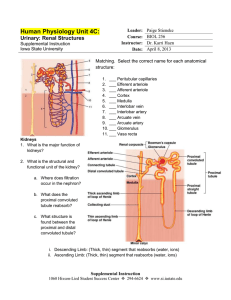
Urinary System Chapter 24 – Day 2 4/7/08 Review Nephron Structure Network with blood vessels Two types of nephrons ♦ Cortical Nephrons – loop of Henle does not extend below cortex ♦ Juxtamedullary nephrons – loop of Henle extends into medulla ♦ Vasa recta – feature of jextamedullary nephrons ♦ 85% are cortical nephrons • Majority of process is done here ♦ 15% are juxtamedullary • Important role in concentrating urine • Conserving water in the body 4/7/08 Renal corpuscle Renal arteries branch into afferent arterioles in the cortex One afferent arteriole enters the renal corpuscle Wall of the renal corpuscle is the Bowman’s capsule Afferent arteriole branches into capillary network ♦ Glomerulus, inside the corpuscle within the bowman’s capsule A second efferent arteriole connects to the glomerulus – brings blood out of the renal corpuscle ♦ (Efferent arteriole is thinner than afferent) Efferent arteriole branches around nephron as peritubular capillaries and vasa recta Eventually the efferent arteriole connects to venules – carries blood to renal veins and out of the kidney 4/7/08 Nephrons & blood supply 4/7/08 Fig. 24.7 Kidneys – Blood supply 4/7/08 Fig. 24.5 Glomerulus Surrounded by 2 layers ♦ Bowman’s capsule: • Visceral epithelium • Parietal epithelium ♦ Separated by capsular space Blood in the glomerulus is bounded by 2 walls ♦ Endothelial cells of the blood vessels ♦ Visceral layer of the bowman’s capsule 4/7/08 Fig. 24.8 Glomerulus Endothelial cells of blood vessels ♦ Have large diameter pores: • Fenestrations • Basement membrane Visceral Layer of the Bowman’s capsule ♦ Special basement membrane = lamina densa ♦ Special cells = podocytes • These have special feet like structures called pedicels • Spaces between pedicels = filtration slit/slit pore Special structures of the endothelial cells and visceral layer restrict the passage of particles according to size (analogous to the filter paper) Capsular space = place where filtrate is released 4/7/08 Glomerulus - barriers 4/7/08 Fig. 24.8 Glomerulus blood boundaries 4/7/08 Fig. 24.8c Filtration in the Glomerulus Blood rushes into glomerulus via the afferent arteriole Difference in diameter between afferent & efferent arterioles results in High Blood Pressure inside the Glomerulus ♦ = Effective Filtration Pressure (EFP) This pushes blood against the endothelial cells ♦ Filtration takes place ♦ Fenestrated capillaries – stops blood cells from passing through, but all other contents go through ♦ Basement membrane – stops large proteins ♦ Pedicels/filtration slits – stops medium-sized proteins from leaving blood 4/7/08 Glomerular Filtration 4/7/08 Fig. 24.10 Filtrate Remaining contents end up in the capsular space and are called filtrate Contents of filtrate: ♦ Water ♦ Small proteins ♦ Glucose ♦ Amino acids ♦ Vitamins ♦ Citric acid 4/7/08 ♦ Ions: Na+, Cl-, K+, HCO3 ♦ ammonia ♦ Urea ♦ Bilirubin ♦ Neurotransmitter ♦ Hormones Filtrate - PCT Filtrate passes to proximal convoluted tubule (PCT) ♦ PCT walls = simple cuboidal epithelium ♦ Outside fluid = peritubular fluid ♦ Then peritubular capillaries PCT – reabsorption begins ♦ 99% of the reabsorption is of organic materials • Glucose, amino acids, vitamins, citric acid ♦ Facilitated diffusion ♦ Transport of Ions = active transport & passive ♦ Water reabsorption = osmosis Enters peritubular fluid, then to capillaries 4/7/08 Filtrate – Loop of Henle Tubular fluid with remaining contents flows into Loop of Henle ♦ Descending & Ascending Limbs Juxtamedullary nephrons – in contact with the vasa recta Reabsorption of water & solutes ♦ (specifically Na+ & Cl-) Descending & Ascending limbs have different properties – very important in concentrating urine 4/7/08 Loop of Henle Descending limb = thin ♦ Permeable to H2O ♦ Mostly impermeable to salts (Na+,Cl-) Ascending limb = thick ♦ Impermeable to H2O and solutes ♦ Prevents diffusion by concentration gradient ♦ Allows selective permeability ♦ Only Na+& Cl- can leave via active transport while wastes stay in ♦ Salts (Na+,Cl-) are pumped out by active transport = reabsorption of Na+& Cl- into blood 4/7/08 Fig. 24.13 Loop of Henle As tubular fluid moves up, salts enter peritubular fluid via active transport into vasa recta Results in a high solute concentration of peritubular fluid Know: ♦ Direction of H2O? Direction of salts? ♦ From which limb? ♦ What is the significance/importance? ♦ How does the countercurrent work? 4/7/08 Fig. 24.13 Loop of Henle Countercurrent flow drives reabsorption ♦ Osmotic concentration is constantly maintained ♦ Allows reabsorption of H2O into blood b/c osmotic concentration is high in the peritubular fluid (due to high salts) ♦ = contercurrent multiplication (exchange increases) Loss of H2O from descending limb concentrates solutes in urine Tubular fluid containing mostly wastes & some ions enters distal convoluted tubule (DCT) 4/7/08 Filtrate – Distal Convoluted Tubule Further reabsorption of salts + (Na & Cl ) ♦ Active and Passive Presence of aldosterone alters rate of Na+ reabsorption Ca2+ may be reabsorbed depending on calcitriol Secretion also occurs in DCT Wastes are not reabsorbed – moves forward to collecting tube 4/7/08 Fig. 24.15 Filtrate – Distal Convoluted Tubule Further reabsorption of salts + (Na & Cl ) ♦ Active and Passive Presence of aldosterone alters rate of Na+ reabsorption Ca2+ may be reabsorbed depending on calcitriol Secretion also occurs in DCT Wastes are not reabsorbed – moves forward to collecting tube 4/7/08 Fig. 24.15 Nephron - Secretion Reabsorption & secretion take place in the DCT Secretion: ♦ Other wastes that did not enter the nephron during filtration ♦ Transported later by secretion ♦ Peritubular capillaries → nephron ♦ PCT & DCT are involved in secretion ♦ K+ and H+ ions – depends on blood levels/blood conditions • Example: H+ ions increase from CO2 conversion, they are secreted to maintain balance • Diabetes: ketones are released = acidic, so more H+ is secreted ♦ NH4+ ions (comes from removal of NH3 group from amino acids) ♦ Other secreted compounds = drugs, creatinine, neurotransmitters 4/7/08 Filtrate – Collecting Duct Urine moves into the collecting tubule (urine) ♦ Some reabsorption: • Na+ ions • HCO3 ions • Some urea reabsorption (helps to maintain high salt concentration in peritubular fluid) Concentration gradient is very important to keep the flow of things moving properly ♦ Ions & H2O enter peritubular fluid, then go to vasa recta • Keeps a constant concentration gradient of high salt levels in the peritubular fluid H2O reabsorption in kidney = very important process 4/7/08 ♦ Helps to keep H2O balanced in the body ♦ Depends on solute concentration Urine - hydration If the body is well hydrated H2O absorption occurs only in the descending limb of Loop of Henle Solute concentration gradient in Loop of Henle & Collecting Tubule 4/7/08 Fig. 24.13 Urine - hydration Dilute urine = large volume because high amounts of water are retained Only ions are reabsorbed heavily If the body is dehydrated – activates pituitary gland to produce antidiuretic hormone (ADH) ♦ ♦ ♦ ♦ ♦ Body conserves H2O in the kidney & thirst response for more H2O intake Special H2O channels open in collecting tubule H2O is reabsorbed from collecting tubule Driven by diffusion because salt concentration is already high outside Yields concentrated urine – small volume (conc. urea) Diuretics like caffeine: ♦ Prevent H2O reabsorption in collecting tubule, force H2O out of cells ♦ Leads to dilute urine but reduces blood volume ♦ Are also used to alter blood pressure 4/7/08 4/7/08 Fig. 24.6 Kidneys – Blood supply 4/7/08 Fig. 24.7 Kidneys – Blood supply 4/7/08 Fig. 24.8 Kidneys – Blood supply 4/7/08 Fig. 24.5 Kidneys – Blood supply 4/7/08 Fig. 24.5