Smarter Healthcare - Community Care of North Carolina
advertisement

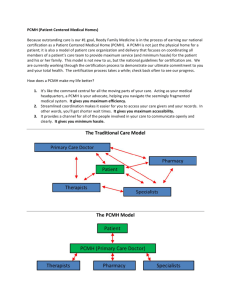
Extracting Value Patient Centered Medical Home Paul Grundy MD, MPH - IBM Director, Healthcare Transformation @Paul_PCPCC https://twitter.com/Paul_PCPCC Beyond Flexner --- Driven by Actionable - Personalized Data Course Objectives • participant will understand/be able to discuss the important trend of PCMH in health care • participant will understand/be able explore the rationale and supporting evidence for PCMH • - participant will understand/be able understand the impact on patients, providers and payers • Disclosure: • – I am a full time Employee of IBM I WILL NOT discuss any pharmaceuticals, medical procedures, or devices • I have gratefully had my expenses covered to do some of my talks about PCMH by Abbvie, Merck, and Pfizer. North Carolina Starts the movement • When Look at the Landscape CCNC was who was called CCNC now into year 18 !! – CCNC at the first roundtable pre-PCPCC. • Jan 2015 --Idaho Embraces Medical Home Model Statewide Programs Seek to Facilitate Innovative Care Transitions In much of the world, no one is in charge. And the result is the most wasteful and Unsustainable – BUT -where the delivery system works – a Patient in a trusting relation with a healer who is a comprehensivist with data is in charge” Away from Episode of Care to Management of Population WITH DATA Per Capita Cost Population Health System Integrator @Paul_PCPCC https://twitter.com/Paul_PCPCC The System Integrator Creates a partnership across the medical neighborhood Drives PCMH primary care redesign Offers a utility for population health and financial management Patient Experience Public Health Community Health Smarter Healthcare 36.3% 32.2% 12.8% -15.6% 10.5% 18.9% 15.0% Drop in hospital days Drop in ER use Increase Chronic Medication use Total cost Drop Inpatient specialty care costs Ancillary costs down Outpatient specialty down Outcomes of Implementing Patient Centered Medical Home Interventions: A Review of the Evidence from Prospective Evaluation Studies in the US - PCPCC Oct 2012 24 July 2014 Michigan Blues’ patient-centered medical home program shows statewide transformation of care YEAR 6 •9.9 percent lower rate of adult ER visits •27.5 percent lower rate of adult ambulatory care sensitive inpatient stays •11.8 percent lower rate of adult primary care sensitive ER visits •8.7 percent lower rate of adult high-tech radiology usage •14.9 percent lower rate of pediatric ER visits •21.3 percent lower rate of pediatric primary-care sensitive ER visits 4,022 primary care doctors at 1,422 practices around the state in its sixth year of operation. These practices care for more than 1.2 million BCBSM members. USA 2012 Ogden UT Wienke Boerma Nivel Institute Utrecht, Holland. Amb Wos Tabulating Systems Era Programmable Systems Era Cognitive Systems Era Watson is ushering in a new era of computing 2011 1900 1950 MobileFirst Patient Consumer Practice transformation away from episode of care Preventive Medicine Chronic Disease Monitoring Medication Refills Acute Care Test Results DOCTOR Master Builder Case Manager Source: Southcentral Foundation, Anchorage AK Behavioral Health Medical Assistants Nursing PCMH Parallel Team Flow Design: the glue is real data, not a doctor’s brain Chronic Disease Monitoring Medication Refills Healthcare Support Team Point of Care Testing Acute Care Test Results Case Manager Source: Southcentral Foundation, Anchorage AK Preventive Medicine Clinician Acute Mental Health Complaint Medical Assistants Chronic Disease Compliance Barriers Behavioral Health Healthcare Will Transform --- Family Medicine for America’s Health Data Driven Every person has a plan Team based Managing a population down to the person . Today’s Care My patients are those who make appointments to see me Care is determined by today’s problem and time available today Care varies by scheduled time and memory or skill of the doctor I know I deliver high quality care because I’m well trained Patients are responsible for coordinating their own care PCMH Care Our patients are the population community Care is determined by a proactive plan to meet patient needs with or without visits Care is standardized according to evidence-based guidelines We measure our quality and make rapid changes to improve it A prepared team of professionals coordinates all patients’ care It’s up to the patient to tell us what happened to them We track tests & consultations, and follow-up after ED & hospital Clinic operations center on meeting the doctor’s needs A multidisciplinary team works at the top of our licenses to serve patients Slide from Daniel Duffy MD School of Community Medicine Tulsa Oklahoma Defining the Care Centered on Patient Superb Access to Care Patient Engagement in Care Team Care Communication Patient Feedback Clinical Information Systems, Registry Care Coordination Mobile easy to use and Available Information Trajectory to Value Based Purchasing: Achieving Real Care Coordination and Outcome Measurement Operational Care Coordination: Embedded RN Primary Care Coordinator and Capacity: Health Plan Care Patient Coordination $ Centered Medical Home Value/ Outcome Measurement: Reporting of Quality, Utilization and Patient Satisfaction Measures HIT Infrastructure: EHRs and Connectivity Source: Hudson Valley Initiative Value-Based Purchasing: Reimbursement Tied to Performance on Value (quality, appropriate utilization and patient satisfaction) Achieve Supportive Base for ACOs and Bundled Payments with Outcome Measurement and Health Plan Involvement Payment reform requires more than one method, you have dials, adjust them!!! “fee for health” “fee for value” “fee for outcome” “fee for process” “fee for belonging “fee for service” “fee for satisfaction” Businesses are no longer accepting cost-shifting. 40% of commercial in-network payments are value-based up from 11% -- 2012 Government and private insurers increasingly are paying for value and outcomes, not volume; they are also employing new payment models for hospitals and clinicians. Half of these payments are “at risk” and half are upside only. Transformation is Here • • • • • HHS to spend $840 million on readying practices for value-based pay. -- Part of the 10 Billion The Transforming Clinical Practice Initiative will invest $840 million over four years to support 150,000 clinicians. It will provide a combination of incentives, tools and information to encourage doctors to team with peers and others to transition to value-based services. Momentum building toward value-based payment methods, this initiative hopes to leverage the success of leading practices, health systems and professional orgs to coach others in how to best move to value-based reimbursement. It fits well into the broader federal strategy. Transforming Clinical Practice Group practices health systems and Medical Societies Impact 150,000 clinicians • AND You ARE READY!!!!!!! • • Benefit Redesign - Patient Engagement Different Strategies for Different Healthcare Spend Segments Those with severe, acute illness or injuries % Total Healthcare Spend Those with chronic illness % of Members Those who are well or think they are well PCMH 2.0 in Action A Coordinated Health System Hospitals Community Care Team PCMH Specialists PCMH Public Health Prevention Nurse Coordinator Social Workers Dieticians Community Health Workers Care Coordinators Public Health Prevention HEALTH WELLNESS Health IT Framework Global Information Framework Evaluation Framework Operations need to move from traditional care provider to health partner if your do not choose innovation (play a better game) you will be forced into disruption ( game Changed for you). Honest you can see it coming and some places is already there Millennials are already finding the convenience, economics and technology in powerful virtual engagement compelling so you can chose innovation or disruption. Virtual access become a required defensive strategy Primary Care team engaged in virtual augmented relationship – or your history loss the relationship. Thank you A comprehensive approach helps reduce costs while improving care KNOWLEDGE INTERVENTION Identify and influence individuals and populations, and recognize intervention opportunities Drive evidence-based and standardized care planning LEARNING Apply new insights from interactions and outcomes to enable continuous transformation COLLABORATION WELLNESS COORDINATION Deliver care and monitor progress across clinical and social requirements Assess and engage individuals and stakeholders to drive individualized care plans Asking New Questions From To How many patients can you see? How many patients’ problems can you solve? From To How can we encourage and convince patients to get required prevention? From To How often should a physician see a patient to optimally monitor a condition? How can we create systems that significantly increase that patients get required prevention? What is the best way to optimally monitor a condition? *Source: 2014 Kaiser Permanente Jack Cochran What new skills are required for the future family physician and what old skills might no longer be necessary? How can we know if the changes underway in our practices are good for patients? What are the implications for how we teach and study family medicine? What new payment models will be required for this model of care to succeed?