17 - Pegasus @ UCF
advertisement

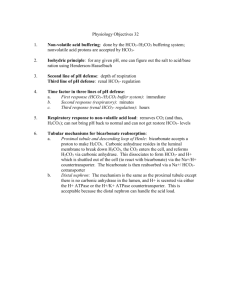
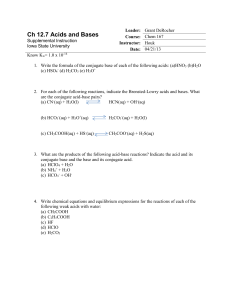
Chapter 17 Physiology of the Kidneys Dr. David Washington Glomerular Filtration A person with a cardiac output of 5,600 ml/min would have a flow rate through the kidneys of about 1,200 ml/min, or 21% of the C.O. 1,200 (renal fraction = = 21%) 5,600 o The glomeruli filter particles up to 80 A, therefore; proteins and blood cells are not filterable. Measurement of GFR (Glomerular Filtration Rate) GFR = Uv p U = concentration of substance in urine P = concentration of substance in plasma V = volume of urine example (inulin) U = 125 mg/ml P = 1 mg/ml V = 1ml/min therefore, Measurement of GFR (Glomerular Filtration Rate) U = 125 mg/ml P = 1 mg/ml V = 1ml/min therefore, GFR 125 mg/ml X 1 ml/min = 1 mg/ml GFR = 125 ml/min That is; 125 ml of plasma had to be filtered to get 125 mg of inulin in the urine. Counter-Current Mechanism Na+ K+ (Urine Formation) Na + H 2O H 2O Cortex Glucose Amino acid 320 400 Outer Medula H 2O Inner Medulla Diffusion passive active 300 400 600 200 400 Na+ 800 600 800 Na+ 1000 800 1000 + Na 600 1200 Highly permeable to Na Impermeable to H2O K+ Counter-Current Mechanism (Urine Formation) Cortex Outer Medula Inner Medulla Net action in loop of Henle - H2O reabsorption Net action at distal tubule: a. ADH - increases reabsorption b. Aldosterone - increases Na reabsorption Countercurrent Multiplier Mechanism Proximal Tubule Tubular lumen Peritubular fluid Na+ + K 70% H2O Glucose Amino acids Glucose Countercurrent Multiplier Mechanism 15% Loop of Henle (Descending limb) H2O Na+ 14% (Ascending limb) Na+ membrane x impermeable H2O Distal Tubule Na+ K+ H2O Diabetes insipidus Autoregulation of Glomerular Filtration Rate (J-G apparatus) Bowman’s capsule Glomerulus Juxtaglomerular cells Macula densa cells Afferent arteriole Efferent arteriole Distal tubule Renin-Angiotensin-Aldosterone Pathway Angiotensinogen Asp-Arg-Val-Tyr-Ile-His-Pro-Phe-His-Leu-Leu-Val-Tyr-Ser 14 Renin Angiotensin I Asp-Arg-Val-Tyr-Ile-His-Pro-Phe-His-Leu Ang.I 10 Converting enzyme (in lungs) Angiotensin II Asp-Arg-Val-Tyr-Ile-His-Pro-Phe 8 Vasoconstriction Aldosterone Compensation for Low Sodium Low Na+ Intake Na+ retention in blood Low plasma Na+ concentration Na+ reabsorption in distal tubules Hypothalamus Aldosterone Posterior pituitary Adrenal cortex ADH Angiotensin II Water reabsorption in collecting ducts Renin Urine Vol Blood Vol Juxtaglomerular apparratus Sympathetic nerve activity Acids, Bases and Buffers H H O OH- H+ + H H OH- H O H H O H-O-H H2O H+ + OHhydroxide Acids, Bases and Buffers HCL CL+ H H + O H H O CLH H H+ CL- O H H HCL Acid in H2O H+ + CL- Acids, Bases and Buffers NaOH + + H H H H H H O - O OH + Na H H OH- O NAOH Base in H2O Na+ + OH- Bicarbonate Buffer System Contains mixture for converting strong acids + bases to weak acids and bases. Example: (H2CO3 and NaHCO3) a) HCL + NaHCO3 H2Co3 + NaCL sodium bicarbonate carbonic acid b) NaOH + H2Co3 NaHCO3 + H20 pk - the ph at which the concentration of the two portions of the buffer are equal. Buffer power - ability to maintain a ph following the addition of acid or base Bicarbonate Buffer System Buffer Curve: 100 25 75 50 50 pk 6.1 75 25 4 5 6 ph 7 8 NaHCO3 Base added Acid added H2CO3 0 Extracellular Fluid pH Henderson-Hasselbalch Equarion (pH caused by the concentration of CO2 in blood) HA H + + A- 1) H2 CO3 H++ HCO3- carbonic acid bicarbonate ion Extracellular Fluid pH (H+)x(HCO3-) 2) KA = (H2CO3) (H+)x(HCO3-) 3) KA = (CO3) Since [H2CO3] in extra-cellular fluids is an express of [CO2], we write --- equation 3. (HCO3-) + 4) log KA = log (H ) + log (CO2) -) + (HCO 3 5) - log(H ) = -logKA + log (CO2) Extracellular Fluid pH 6) pH = pKA + (HCO3-) (CO2) 7) pH =p KA + log (HCO3-) 0.03 x Pco2 (solubility coefficient in mM/L) pKA= 6.1; [HCO3-] = 24mM/L in arterial blood pH = 6.1 + log 24 0.03 x 40 = 6.1 + log 20 = 6.1 + 1.3 = 7.4