File
advertisement

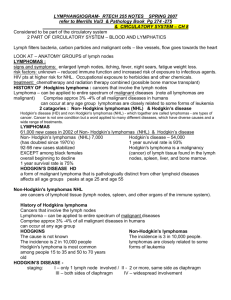
Lecture 8 and 9 Lymphomas; Multiple Myeloma, Plasma cell disorders; Lipid storage disease and Histiocytosis Abdulkarim Aldosari Objectives List distinguishing features for nodular lymphocyte predominant, mixed cellularity, lymphocyte rich, lymphocyte depletion and nodular sclerosis Hodgkin lymphoma List distinguishing features for the four stages of Hodgkin lymphoma Describe classification criteria, differential diagnosis, prognosis and treatment for Hodgkin and non Hodgkin lymphomas Describe and compare multiple myeloma and monoclonal gammopathy Describe the workup of patients with plasma cell dyscrasia Define and describe amyloidosis Name and describe enzyme deficiencies seen in Gaucher’s disease, Niemann-Pick, and Tay-Sachs disease Describe clinical features and laboratory findings of Mucopolysaccharidoses and seablue histiocyte syndrome Lymphomas • http://blausen.com/?Topic=9562 Lymphomas - Introduction Malignant lymphomas are a heterogeneous group of diseases From cells of the lymphoid tissue • Lymphocytes • Histiocytes • Reticulum cells Two categories • Hodgkin disease/ Hodgkin lymphoma • Lymphocytic lymphoma/non-Hodgkin lymphomas (NHLs) Introduction to the lymphomas Difficulties involved in lymphoma diagnosis due to the many subcategories Need to make distinction between: • Benign and malignant lymphoid proliferations • Hodgkin versus non-Hodgkin lymphoma • Subcategories of each type of lymphoma Definitive diagnosis may not be possible Introduction to Hodgkin Lymphoma First described by Thomas Hodgkin in 1832 Samuel Wilks in 1865 applied the term Hodgkin disease In 1898 Sternberg and in 1902 Reed described the histological features of Hodgkin disease, the unusual cell that is characteristic of Hodgkin disease = Reed-Sternberg cell Two distinct clinical and pathological disease • Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) • Classical Hodgkin lymphoma (CHL) Etiology and pathogenesis Possible viral etiology • Epstein-Barr virus (EBV) EBV nucleic acids demonstrated in 80% of all cases of Hodgkin lymphoma (HL) EBV antigens detected in 50% of the cases • CMV, Herpesvirus 6 also implicated • Mechanism is unclear • Possibly a preceding immunosuppression causing an abnormal immune response to the infections HL – malignant clonal proliferation • A small percentage of Reed-Sternberg cells and its variants • A larger percent of B cells Pathology Reed-Sternberg cell – cytological hallmark of HL Large cell ( up to 45 µm ) with abundant acidophilic cytoplasm Multinucleated or polylobed nucleus Gigantic, inclusion like nucleoli Halo effect around the nucleoli Not necessarily diagnostic because seen in a variety of other conditions Helpful in suggesting the possibility of HL or a subclassification of HL Reed-Sternberg cells in the proper cellular, stromal and clinical setting in conjunction with immunophenotyping → diagnosis of HL Nodular lymphocyte predominant HL • 5% of cases • Pathologically and clinically distinct from HL • Characterized by a nodular, and/or a diffuse proliferation of scattered large neoplastic cells known as L&H , popcorn cell, or lymphocyte predominant cells (LP cells) L&H = lymphocyte histiocyte RS variant Popcorn cells are Reed Sternberg variants • Most of the lymphocytes found in the lymph nodes are normal (not cancerous) Nodular lymphocyte predominant HL • Occurs at any age with a peak incidence at 40yrs • Cervical and axillary lymph nodes are most frequently involved • Presents as an early stage disease; has slow progression and excellent outcome with standard therapy • Recurrence is common and occurs in 21% of cases • The immunophenotype of the L&H cells is distinct from the cells of the classic Hodgkin's lymphoma • Unlike classical Hodgkin Lymphoma, the LP cells show immunoreactivity with CD45 and CD20 and no staining with CD30 or CD15 • There is consistent staining with CD20, CD22, and CD79a • http://www.universitypathologists.com/education/case-of-the-month/february-2011 Nodular lymphocyte predominant HL • Slightly higher incidence in the U.S. among blacks than whites, and a lower incidence among Asians • 3:1 male predominance • Shows a propensity toward peripheral (neck and/or axilla) • Nodal spread is dis-contiguous, compared with the contiguous nodal spread of classical HL. • In 50%–60% of NLPHL cases, the time between the initial presentation of lymphadenopathy and the diagnosis of NLPHL is 6–12 months or longer http://theoncologist.alphamedpress.org/content/14/7/739.long Nodular lymphocyte predominant HL • Prognosis is good - 90-100% remission rate with primary therapy • Relapse seen in 10-15% of patients and occurs on average 3-6 years after diagnosis • Overall 10 year survival rates are >90% in limited stage disease Classic Hodgkin Lymphoma Defined by the observation of classic Reed-Sternberg cells in the appropriate cellular and stromal background Background of the lesion determines the subclassification of CHL: Nodular sclerosis HL • Most common subtype of HL; 60-80% of all cases of HL • The involved lymph nodes contain R-S cells Normal WBCs Lacunar cells (grouped lacunars)- type of RS cells Scar tissue (birefringent collagenous sclerosis) • The disease is more common in women than men • Usually affects adolescents and adults under 50 • Most patients are cured with current treatments Classic Hodgkin Lymphoma Mixed-cellularity HL • Accounts for about 15-30% of all cases of HL • Found more commonly in men than women • Lymph nodes contain heterogeneous mix of cells; R-S cells in addition to several other cell types • Primarily affects older adults • More advanced disease is usually present by the time this subtype is diagnosed Classic Hodgkin Lymphoma Lymphocyte-rich HL • < 5% of HL cases • The disease may be diffuse (spread out) or nodular (knot-like) in form • Characterized by the presence of numerous normal-appearing lymphocytes and classical R-S cells. • Usually diagnosed at an early stage in adults and has a low relapse (returns after treatment) rate Lymphocyte depletion HL • Rarely diagnosed • Abundant R-S cells and few normal lymphocytes are present in the lymph nodes of patients with this subtype • Aggressive and usually not diagnosed until it is widespread through the body Classic Hodgkin Lymphoma Hodgkin Lymphoma - Classification Type Histologic Features Frequency Prognosis Nodular sclerosis Bands of fibrosis, lacunar cells Most frequent type (60-80%), more common in women Good, most are stage I or II Mixed cellularity Composed of many different cells Most frequent in older Fair, most are stage persons, second most frequent III overall (15-30%) Lymphocyte rich Mostly reactive lymphocytes Uncommon (5%). Older adults and many Reed-Sternberg cells Good to excellent Lymphocyte depletion Many Reed-Sternberg cells and Rare (<1%) variants Poor, most are stage III or IV Lymphocyte predominance Mostly B-cells and few ReedSternberg variant cells Good, most are stage I or II Uncommon (5%) Classic Hodgkin Lymphoma Histologic progression HL progresses from: Lymphocyte rich → mixed cellularity → lymphocyte depletion lymphoma Clinical features: • ~9,000 new cases of HL are projected each year • Most commonly diagnosed in young adults 15-35yrs and in adults over 50 • Most patients with HL present with swelling of the lymph nodes (which is often but not always painless) • Fever, night sweats, unexplained weight loss, and lack of energy Diagnosis and staging of HL Clinical staging for patients with Hodgkin lymphoma (HL) includes • Careful history • Detailed physical examination • Laboratory studies (CBC, sedimentation rate, chemistry panel; liver, kidney, bone profile) • Thoracic and abdominal/pelvic computerized tomographic (CT) scans • Positron emission tomography (PET) scans, gallium scans • Bone marrow biopsy if symptomatic, Cytopenia or advanced stage Diagnosis and staging of HL Most widely used staging scheme - Cotswold’s revision of the Ann Harbor classification Stage I - Involvement of a single lymph node region (cervical, axillary, inguinal, mediastinal) or lymphoid structure (spleen, thymus, or Waldeyer's ring) Stage II - Involvement of two or more lymph node regions or structures on the same side of the diaphragm. Hilar nodes should be considered to be "lateralized“. All nodal disease within the mediastinum is considered to be a single lymph node region. The number of anatomic regions should be indicated by a subscript (II-3). Stage III – Involvement of lymph node regions or lymphoid structures on both sides of the diaphragm. III-1 with or without the involvement of the spleen, hilar, celiac or portal nodes; and stage III-2 with involvement of the paraaortic, iliac, inguinal, or mesenteric nodes Stage IV - Involvement of one or more extranodal organs or tissue beyond that designated E, with or without associated lymph node involvement Diagnosis and staging of HL Subclassification of stage Stages I, II, III, and IV adult HL can be sub classified into A and B categories: B for those with defined general symptoms A for those without B symptoms The B designation is given to patients with any of the following symptoms: • Unexplained loss of more than 10% of body weight in the 6 months before diagnosis • Unexplained fever with temperatures above 38°C • Drenching night sweats http://www.cancer.gov/cancertopics/pdq/treatment/adulthodgkins/HealthProfessional/p age3 Stage1 of HL Stage I adult nonHodgkin lymphoma. Cancer is found in one lymphatic area (lymph nodes, tonsils, thymus, or spleen). In stage IE (not shown), cancer is found in one organ or area outside the lymph nodes. E: is used if the disease is "extranodal" (not in the lymph nodes) or has spread from lymph nodes to adjacent tissue Stage 11 of HL Stage II: Cancer in two or more lymph node groups, and both are either above (a) or below (b) the diaphragm Stage IIE Cancer in one or more lymph node groups either above or below the diaphragm and outside the lymph nodes in an organ or area on the same side of the diaphragm as the lymph nodes with cancer (a). Stage 111 of HL Stage III - in one or more lymph node groups above and below the diaphragm (a). Stage IIIE - in lymph node groups above and below the diaphragm and outside the lymph nodes in a nearby organ or area (b). Stage IIIS - in lymph node groups above and below the diaphragm (a) and in the spleen (c). Stage IIIE plus S,- in lymph node groups above and below the diaphragm, outside the lymph nodes in a nearby organ or area (b), and in the spleen (c). Stage 1V of HL Stage IV: Cancer found throughout one or more organs that are not part of a lymphatic area (lymph nodes, tonsils, thymus, or spleen) (a); or in one organ that is not part of a lymphatic area and has spread to lymph nodes far away from that organ (b); or cerebrospinal fluid (not shown), the liver, bone marrow, or lungs. Treatment and prognosis • Based on staging evaluation • Multiagent chemotherapy • 10 year survival for stage 1 and 11 > 80% • 10 year survival for stages 111 and 1V improved with aggressive chemotherapy ~70% Non-Hodgkin Lymphoma • Any of a large group of cancers of lymphocytes • Can occur at any age • Marked by lymph nodes that are larger than normal, fever, and weight loss • Many different types divided into aggressive (fast-growing) and indolent (slowgrowing) types • Can be formed from either B-cells or T-cells • Estimated new cases and deaths from non-Hodgkin lymphoma in the United States in 2013: New cases: 69,740 Deaths: 19,020 http://www.cancer.gov/cancertopics/types/non-hodgkin Non-Hodgkin Lymphoma B-cell non-Hodgkin lymphomas • Burkitt lymphoma • Chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) • Diffuse large B-cell lymphoma • Follicular lymphoma • Immunoblastic large cell lymphoma • Precursor B-lymphoblastic lymphoma • Mantle cell lymphoma Non-Hodgkin Lymphoma T-cell non-Hodgkin lymphomas • Mycosis fungoides • Anaplastic large cell lymphoma • Precursor T-lymphoblastic lymphoma Lymphomas that occur after bone marrow or stem cell transplantation are usually Bcell non-Hodgkin lymphomas Prognosis and treatment depend on the stage and type of disease. Etiology and pathogenesis • Damage to region of the genetic code that regulate growth and reproduction of immune cells • May be due to chemicals, ionizing radiation, viruses (EBV) • Genetic damage associated with numeric and/or structural alterations in chromosomes • Chromosomal abnormalities demonstrated in 60% of NHL cases • Mainly translocations in chromosomes 2,8,14,22 • Chromosomal regions relates to function of the genetic material t(11;14) = BCL1-IgH; t(14;18) = IgH- BCL2; t(3;14) = BCL6-IgH Etiology and pathogenesis Best example Burkitt’s lymphoma – in 90% of cases – c-myc proto-oncogene located at region q24 of chr 8 translocated to IgH chain 14q32 Also in 40% of large-cell lymphomas Pathology of NHL Classification schemes based on: • Growth pattern: nodular or diffuse • Cytological features of malignant cells Historically the most widely used in USA: Working formulation for clinical usage Working Formulation has become outdated and less useful to clinicians and pathologists European and American pathologists proposed a new classification • The Revised European American Lymphoma (REAL) classification Pathology of NHL Since 1995, members of the European and American Hematopathology societies have been collaborating on a new World Health Organization (WHO) classification • Represents an updated version of the REAL system • Utilizes clinical, morphological, immunophenotypic and genotypic features • Requires an understanding of the morphology of the lymph nodes and the maturation of normal lymphocytes Pathology of NHL The WHO modification of the REAL classification identifies three major categories of lymphoid malignancies based on morphology and cell lineage: • B-cell neoplasms • T-cell/natural killer (NK)-cell neoplasms • Hodgkin lymphoma Both lymphomas and lymphoid leukemias are included in this classification because both solid and circulating phases are present in many lymphoid neoplasms and distinction between them is artificial. • B-cell chronic lymphocytic leukemia and B-cell small lymphocytic lymphoma are different manifestations of the same neoplasm • Also lymphoblastic lymphomas and acute lymphocytic leukemias Within B-cell and T-cell categories, two subdivisions: • Precursor neoplasms = earliest stages of differentiation • Mature neoplasms Lymph nodes Three major anatomical regions Cortex – populated by B cells, plasma cells, reticular cells B cell organized into nodules - 1o or 2o follicles 1o follicles → 2o follicles containing a germinal center Germinal center surrounded by mantle zone (crescent of B cells) Germinal center contains – centrocytes, centroblasts, dendritic cells, histiocytes/macrophages Lymph nodes Paracortex – occupied by Tcells Medulla – contains T cells, B cells, macrophages, plasma cells NHL arise from any of these normal cellular counterparts B cell – most common 85-90% T/NK – 10-15% Histiocytes and dendritic cells - < 1% Follicular B-cell lymphoma • The most common of the indolent non-Hodgkin's lymphomas = 40% of adult NHL • The second-most-common form of non-Hodgkin's lymphomas overall • It is a lymphoma of follicle center B-cells (centrocytes and centroblasts) with at least partial follicular growth pattern Follicular growth should be included in the pathologic assessment • Positive for the B-cell markers CD10, CD19, CD20, and CD22 but almost always negative for CD5 • A translocation between chromosome 14 and 18 results in the overexpression of the bcl-2 gene Follicular B-cell lymphoma According to the WHO criteria, the disease is morphologically graded into • grade 1 (<5 centroblasts per high-power field (hpf)) • grade 2 (6–15 centroblasts/hpf) • grade 3 (>15 centroblasts/hpf) grade 3A (centrocytes still present) grade 3B (the follicles consist almost entirely of centroblasts More aggressive than grades 1 and 2 Progression from follicular to more aggressive diffuse large cell lymphoma – 40% of cases Male: female – 1:1 Survival rate at 5yrs >60% Mantle cell lymphoma Characterized by • small-to-medium sized lymphocytes with pale staining cytoplasm • Irregular nucleus • Inconspicuous nucleoli • Cells express CD5, Cd34 • t(11;l4) • A disease of older adults • Male: female – 3:1 • Disease widespread at diagnosis • Lymph nodes and spleen as most common sites of involvement • One of the rarest of the NHL Mucosal-associated lymphoid tissue • Marginal zone- poorly defined anatomical compartment of the lymph nodes • Small cleaved cell (centrocytes-like) • Lymphomas related to marginal zone cells – referred to as lymphomas of the mucosa-associated lymphoid tissue (MALT) • Frequently of the stomach, but virtually any mucosal site can be afflicted. • Originate from B cells in the marginal zone of the MALT • Also called extranodal marginal zone B cell lymphoma Non-Hodgkin's Lymphomas Type Histologic Features Immunogenetics Small Lymphocytic Lymphoma Small and well-differentiated B lymphocytes, with diffuse effacement of nodal architecture and no follicles CD19, 5; Bcl-2 and Bcl-6 expression Follicular Lymphoma Nodal architecture is effaced CD19, 20, 79a; t(14:18); Bcl-2 (predominantly small cell) by monotonous, crowded expression follicles composed of monomorphous small cleaved B-lymphocytes Clinical Features Seen in older adults, it is essentially the solid tissue (lymph nodal) component of chronic lymphocytic leukemia; disease tends to be generalized but with indolent course and prolonged survival; some may transform to more aggressive lymphomas Most common type, seen in adults, often involves multiple lymph nodes, course is indolent, with prolonged survival, though some may transform to a large cell lymphoma Diffuse Large B-cell Lymphoma Cells are large, with prominent nucleoli and abundant cytoplasm and many mitoses. Most are Bcell, but 20% are T-cell phenotype CD19, 20, 79a; some have t(14;18); some have Bcl-2 and Bcl-6 expression; linked to EBV infection; negative TdT Though often localized, they tend to be aggressive extranodal masses; seen in adults and children, can be seen in HIV infection Burkitt Lymphoma Intermediate sized Blymphocytes (smallnoncleaved cells) CD10, 19, 20, 79a; t(8:14) is characteristic; African form linked to EBV infection; negative TdT, Bcl-2, CD5, CD23; surface IgM+ Endemic in Africa with mandibular and abdominal involvement; sporadic elsewhere with abdominal involvement; affects mainly children and young adults High-grade B-cell Lymphoma (small noncleaved) Burkitt-like Lymphoma Intermediate sized BCD19, 20 lymphocytes (small non-cleaved cells) Sporadic; may be seen with HIV infection Precursor T or B-cell Lymphoblastic Lymphoma/Leukemia (Lymphoblastic Lymphoma) Intermediate sized lymphocytes B-cells are CD19, 20, Seen in children and in a diffuse pattern sometimes CD10; T-cells are adolescents; T-cell type often in CD3 and 8; all are TdT positive mediastinum; very aggressive and can progress to acute lymphocytic leukemia Mantle Cell Lymphoma Small to medium sized B cells CD 19, 20, 43; t(11;14); Bcl-1 (Cyclin D1) expression Seen in adults in middle age; often advanced at diagnosis and may be extranodal, including multifocal submucosal nodules in bowel Marginal Zone Lymphoma CD19, 20, 79a; negative CD5 and 10 Seen in middle aged adults; typically arises in areas of immune activation (Hashimoto thyroiditis, Sjogren syndrome, Helicobacter pylori gastritis); similar lesions associated with mucosal lymphoid tissue are called MALTomas (mucosa-associated lymphoid tissue tumors); may transform to diffuse large B-cell lymphoma Small to medium sized B cells T-cell and NK cell lymphomas • T-cell lymphomas account for ~15% of all NHLs in the USA • NK cell shares many features with T-cells • When NK cells become cancerous, the cancer is called NK or NK/T-cell lymphoma • Many different forms of T-cell lymphomas, some of which are extremely rare • T-cell lymphomas can be aggressive (fast-growing) or indolent (slow-growing) T-cell and NK cell lymphomas • Peripheral T-cell lymphoma (PTCL) - entire group of mature or "post-thymic" T-cell lymphomas (arise from mature T-cells) distinguishes them from the immature T-cell lymphomas such as acute lymphocytic leukemia (ALL) or lymphoblastic lymphoma. • Under this broad meaning, almost all types of T-cell lymphoma fall under the category of PTCL • Cells characteristically express CD3, the T-cell receptor (TCR) αβ or γδ chains, and either CD4 or CD8 • Natural killer (NK) cells share the same ontogeny with T cells + NK-cell markers CD56 T-cell and NK cell lymphomas Because of morphological phenotypic and genotypic complexity of T/NK cells clinical features are necessary in classification of the lymphomas Three patterns of clinical presentation of mature T/NK cell lymphoma 1. Nodal 2. Extranodal 3. Leukemic/disseminated T-cell and NK cell lymphomas Nodal group most common in western countries Peripheral T-cell lymphoma, unspecified Anaplastic large cell lymphoma Angioimmunoblastic T-cell lymphoma Peripheral T-cell lymphoma, unspecified (PTCL) • Most common of all the T-cell lymphomas • Involves the lymph nodes, other sites such as the liver, bone marrow, gastrointestinal tract, and skin, may also be involved. • PTCLs is aggressive and requires combination chemotherapy upon diagnosis • Usually Tdt-, CD3+, CD4+, CD8- T-cell and NK cell lymphomas Anaplastic large cell lymphoma • Accounts for ~12-15% of all T-cell lymphomas in adults and 10-30% of all lymphomas in children. • Can be divided into three types: 2 systemic (presents in lymph nodes or organs) subtypes 1 non-systemic subtype – appears only on the skin - not to be confused with primary cutaneous anaplastic large cell lymphoma The systemic types are usually fast-growing, while the skin-only type is usually more slow-growing • Characterized by large cell with kidney-shaped nuclei and eosinophilic inclusion-like region adjacent to the nucleus Unusual in that it responds to therapy Overall survival – 80% at 5yrs T-cell and NK cell lymphomas Angioimmunoblastic T-cell lymphoma • Fast-growing; accounting for 1-2% of all T-cell lymphomas in the United States • Initial symptoms often include swollen lymph nodes and systemic symptoms such as fever and rash. • It is generally treated like other fast-growing T-cell lymphomas, but can be managed with milder therapies in certain circumstances • Affected lymph nodes contain mixture of atypical lymphoid cells, follicular dendritic cells, thick-walled high endothelial venules • CD4+, CD21+ • Usually follows an aggressive clinical course T-cell and NK cell lymphomas Primary Cutaneous T-cell Lymphoma (PCTL) • Extranodal presentation • Accounts for 2-3% of all NHL cases and usually affects adults. • A group of typically slow-growing cancers that appear on and are most often confined to the skin Mycosis fungoides, which appears as skin patches or plaques, is the most common type of cutaneous T-cell lymphoma Less common forms include: Sézary syndrome Primary cutaneous anaplastic large cell lymphoma Lymphomatoid papulosis T-cell and NK cell lymphomas Require thin sections of fixed paraffin-embedded material to observe the peculiar cerebriform nucleus of malignant T-cells 90% exhibit pan-T+, CD4+, CD810% exhibit pan-T+, CD4-, CD8+ Different from systemic anaplastic large-cell lymphoma Both CD30+, but PCTLs are epithelial membrane antigen (EMA)- negative; T(2;5) translocation (+) for systemic anaplastic large-cell lymphoma (-) for PCTL PCTL is indolent, incurable versus the aggressive curable systemic anaplastic lymphoma T-cell and NK cell lymphomas Staging is similar to that of HD Treatment and prognosis Based on two categories 1. Indolent relatively long median survival without therapy (7-9 yrs) Can be treated with radiotherapy 90% present at stage 111 or 1V- sensitive to radiation and chemo, but incurable with standard Multiagent chemo 2. Aggressive Rapidly fatal if untreated Potentially curable with aggressive treatment strategies • Adults > 45yrs have longer survival than younger patients • Median survival more favorable for B-cell than for T-cell lymphoblastic lymphoma Multiple myeloma and related plasma cell disorders Multiple myeloma is a disorder characterized by: • Proliferation of abnormal plasma cells in the BM • Tumor of plasma cells – plasmacytoma • Monoclonal gammopathy – over production of an antibody in the serum • Secretion of Bence-Jones proteins in the urine • Symptoms of bone destruction, hypercalcemia, kidney failure, hyperviscosity, pancytopenia, anemia, bleeding episodes, increased susceptibility to infections Plasma cell development B cells develop from multipotential stem cells present in BM. Following encounter with Ag, naïve B cells can differentiate into short-lived plasmablasts, secreting predominantly IgM- first line of defense against infection. Alternatively, activated naïve B cells can seed a GC, where affinity maturation and differentiation into long-lived memory and plasma cells occur. Following their generation, memory cells and PCs can then migrate into niches in distinct sites (MALT, BM, splenic red pulp) where they receive survival cues from neighboring cells. Immunoglobulin • Igs have two identical light chains (25kD), two identical heavy chains (50kD) • Held together by disulfide bonds • Antibody produced by each plasma cell has only one type of light chain and one type of heavy chain • 5 types of heavy chains;γ, α, μ,δ, ε IgG1-4, IgA1,2 • 2 types of light chains; κ, λ Immunoglobulins • IgG, IgA, IgM, IgD, IgE • IgM does not cross the placenta Transient antibody produced in response to infection Unmeasurable within 2wks after initiation • IgG next to respond Remains until antigenic stimulus is removed • IgG and IgA form dimers IgA provides protection of epithelial surfaces in GI tract and airways • IgE – allergic/hypersensitivity reactions • IgD – role unclear • Overproduction of Igs is the hallmark of plasma cell disorders Laboratory recognition and measurement Electrophoresis (SPEP) • Total protein in serum measured in routine chemistry • Includes albumin, Igs, α1-antitrypsin, α2-macroglobulin, transferrin, β-lipoprotein • Total albumin also measured • Total protein – albumin = ~Ig fraction • Need to differentiate between polyclonal and monoclonal Polyclonal – in infections Monoclonal – plasma cell disorders • Then perform Immunofixation to investigate abnormal spike on SPEP Electrophoresis Normal pattern Monoclonal spike Polyclonal production IgM M spike Hypogammaglobulinemia Immunofixation (IFE) Proteins separated by electrophoresis Mono-specific antibody added Precipitation of proteins occur → washing → staining of remaining immunoprecipitate Example of identification of a monoclonal serum protein by immunofixation electrophoresis The first track is serum protein electrophoresis (ELP). The next tracks are IgG, IgA, IgM, κ light chains and λ light chains (L) The arrow indicates the position of the monoclonal protein. The second track identifies the protein as IgG after reaction with IgG antibody and protein staining. The sixth track identifies the light chain as λ. Laboratory recognition and measurement Quantitative Igs • By measuring decree of turbidity by light scatter caused by Ag-Ab complexes • Mix patient sample with specific Ab reagent • Use nephelometer • Clonality to be determined by SPEP and IFE Free serum light chains (FLC) • Detect monoclonal FLC not detected by SPEP or IFE • Automated immunoassay • For diagnosis of and monitoring of myelomas and Amyloid light chain amyloidosis Laboratory recognition and measurement Bence-Jones proteinuria • Imbalanced Ig production yields an excess of free light chains (κ/λ) • Rapidly metabolized by blood → increased production of FLC being filtered into urine • Proteins precipitate at 40-60oC, dissolve at 100oC, re-precipitate on cooling • Need 24-hr urine collection • FLC can be deposited in kidneys → leakage of protein into urine and kidney failure Clinical consequences of increased monoclonal Ig Hyperviscosity syndrome • Viscous blood → decreased blood flow to vital organs → increased workload on the heart → headaches, dementia, stroke, coma, congestive heart failure • Most cases seen with IgM, IgA, IgG3 – higher molecular weights • Plasmapheresis – plasma exchange in symptomatic patients Decreased production of normal Igs • Abnormal Ig suppresses plasma cell production of other Igs → increased susceptibility to infections (main cause of death of multiple myeloma patients) • May require intravenous infusion of Ig Clinical consequences of increased monoclonal Ig Cryoglobulinemic syndrome • Due to the presence of abnormal Igs called cryoglobulins in the blood • Cryoglobulins become thick or gel-like in cold temperatures → block blood vessels throughout the body • On exposure to cold, patients experience painful extremities, palpable purpura • Can lead to complications ranging from skin rashes to kidney failure Clinical consequences of increased monoclonal Ig Cryoglobulinemic syndrome Three main types, depending on the type of antibody that is produced: • Cryoglobulinemia type I Monoclonal Ig (IgG or IgM) Waldenstrom’s macroglobulinemia and/or multiple myeloma • Cryoglobulinemia type II Mixed polyclonal Ig Patients with viral infections; HCV, HIV • Cryoglobulinemia type III Mixed Igs Secondary to connective tissue disease Monoclonal gammopathy of undetermined significance (MGUS) – benign monoclonal gammopathy Evident when patient has small M spike Urine light chain of < 1g/24hrs No lytic bone lesions < 10% plasma cells in BM No end organ damage from monoclonal Ig overproduction 20% develop multiple myeloma, NHL, CLL Multiple myeloma • Most common plasma cell dyscrasia • Affects terminally differentiated B cells • Multi step process • Incurable but responsive to various therapies • Survival ranges from <1yr – 15yrs • Characterized by triad: Abnormal proliferation of plasma cells in BM Over production of monoclonal Ig Lytic/destructive bone disease • Disease manifestations of triad: Life threatening end-organ damage Renal insufficiency Anemia, immunosuppression, infections Multiple myeloma Most devastating feature Osteolytic lesions → bone pain, pathologic fractures, spinal cord compression, hypercalcemia • Accounts for 10% of all hematological malignancies; 1% of all cancers • Median age of presentation – 67yrs • Higher in men than women • Only hematological malignancy that is higher among Blacks, lowest in Asians • Unknown cause – but associated with chronic stimulation of immune system Diagnostic work up of Multiple myeloma If clinical symptoms (anemia, renal insufficiency, bone pain, neuropathy, high protein levels) suggests MM then perform confirmatory testing to establish stage and prognosis Diagnostic criteria 1. Biopsy proven plasmacytoma 11. BM Plasmacytosis 111. Monoclonal protein- M spike CRAB: Calcium; >11mg/dL Renal insufficiency; creatinine >2 mg/dL Anemia; Hgb <10g/dL Bony lesions; lytic lesions, osteoporosis Diagnostic work up of Multiple myeloma Blood count and PB smear • CBC – normocytic normochromic anemia • PB smear – rouleaux formation of RBC due to ↑ Igs in blood • ↑ Sedimentation rate blood test measures how quickly RBCs settle in a test tube in one hour. The more red cells that fall to the bottom of the test tube in one hour, the higher the sed rate Diagnostic work up of Multiple myeloma Chemistry studies • ↑ BUN, creatinine (kidney function affected by MM) • ↑ Calcium – calcium is usually bound to albumin, unbound or free calcium major cause of symptoms; • ↓ albumin- prognostic criterion in MM • Β2- Microglobulin – most useful predictor of tumor load and ↓ activity – predicts the prognosis for MM • C-reactive protein Diagnostic work up of Multiple myeloma Bone marrow examination • ↑ plasma cells – forms sheets with immature, bi-nucleated, large cells plasmacytoma • Flame cells – large intensely staining (IgA) • Plasmacytosis 10-100% • CD38,CD56,CD138 (+) • sIg, pan-B-cell antigen CD19 (-) • ± CD20, CD52 Diagnostic work up of Multiple myeloma X-rays, CT scans • A series of X-rays are taken to find out whether there is any bone damage. Any sign of bone damage will appear as dark areas in X-ray pictures • If the doctor requires more detailed images an MRI (magnetic resonance imaging) or CT (computerized tomography) scan may be ordered Cytogenetics • Slow to be recognized and implemented • Chromosomal abnormalities found in 30-40% of patients • Monosomy 13, 13q14 deletion and hypodiploidy have worst prognosis • Chromosomal translocations • Gene expression profiling – emerging technology to id subgroups Treatment Waldenström's macroglobulinemia • Lymphoplasmacytic lymphoma • Type of lymphoproliferative disease - shares clinical characteristics with the indolent non-Hodgkin lymphomas • Overproduction of the IgM antibody → hyperviscosity makes it harder for blood to flow through small blood vessels • 1,400 people in the United States are diagnosed every year • Most people with this condition are over age 65, however, it may occur in younger people • The average survival ~ 6.5 years. Some people live more than 10 years • In some people, the disorder may produce few symptoms and progress slowly Waldenström's macroglobulinemia • Physical examination - a swollen spleen, liver, and lymph nodes. An eye exam may show enlarged veins in the retina or retinal bleeding (hemorrhages) • Cryoglobulinemic purpura • CBC - ↓ RBCs and platelets Bleeding of gums and nose Prolonged bleeding time • Blood chemistry – evidence of kidney disease • A serum viscosity test can tell if the blood has become thick Symptoms usually occur when the blood is four times thicker than normal • SPEP shows ↑ of the IgM antibody Levels seen are generally greater than 3 g/dL Waldenström's macroglobulinemia Chemotherapy - primary treatment Alkylators Rituximab – monoclonal Ab against CD20 Amyloidosis • Protein conformation disorder • Protein becomes insoluble → deposition in extracellular matrix of organs • Most common precursor protein that result in amyloidosis – protein derived from Ig light chain fragments (λ secretions) – source plasma cell • Less common – AA amyloidosis – associated with inflammation • Rare and potentially fatal when deposited insoluble proteins impair organ functions • Causes progressive loss of organ function • Chemotherapy or stem cell transplantation and plasmapheresis to eliminate the plasma cell • Similar to Light chain deposition on disease ( LCDD) LCDD do not form amyloid fibrils, and is usually related to κ secretions Lipid storage disease and histiocytosis Lipid storage diseases, lipidoses, lysosomal storage disease • Group of autosomal inherited metabolic disorders • Harmful amounts of fatty materials (lipids) accumulate in various cells and tissues in the body • Caused by enzyme deficiencies - either do not produce enough of one of the enzymes needed to metabolize lipids or have enzyme defects • Over time excessive storage of fats → permanent cellular and tissue damage particularly in the brain, peripheral nervous system, liver, spleen, and bone marrow Lipid storage disease Most widely known: 1. Gaucher’s disease 2. Niemann-Pick disease 3. Tay-Sach’s disease 4. Mucopolysaccharidose – rare Increased incidence of Gaucher’s and Tay-Sach’s in Ashkenazi Jews Wide clinical expression- from asymptomatic to fatal Prenatal detection is the aim of control Enzyme replacement – current effective therapy Gaucher disease Most common of the lipid storage diseases Caused by a deficiency of the enzyme βglucocerebrosidase Mutations in the GBA gene greatly reduce or eliminate the activity of beta-glucocerebrosidase → Accumulation of unmetabolized substrate glucocerebroside in cells • Mainly in the monocyte-macrophage system • Produces the distinctive Gaucher’s cells – histiocytes 20-100µm in diameter with displaced nucleus Clinical Triad • Hepatoslenomegaly • Gaucher’s cells in BM • ↑ serum acid phosphatase Gaucher disease Fatty material can collect in the spleen, liver, kidneys, lungs, brain, and bone marrow. Symptoms may include: • enlarged spleen and liver • liver malfunction • skeletal disorders and bone lesions that may cause pain and fractures • severe neurologic complications • swelling of lymph nodes and (occasionally) adjacent joints • distended abdomen • a brownish tint to the skin, anemia • low blood platelets, and yellow spots in the eyes • Persons affected most seriously may also be more susceptible to infection Gaucher disease Type 1- most common 10-25% of patients No treatment needed Hepatoslenomegaly Type 2 – more uniform presentation than type 1 Type 3 – two distinct subtypes, a and b Gaucher’s disease treatment Enzyme replacement treatment given intravenously every two weeks can dramatically decrease liver and spleen size, reduce skeletal abnormalities, and reverse other manifestations. Successful bone marrow transplantation cures the non-neurological manifestations of the disease – high risk therapy, rarely performed for Gaucher’s disease Niemann-Pick disease Heterogeneous group of disorders Increased incidence in Jewish population This disorder is divided into five main types based on the genetic cause and the signs and symptoms (A,B,C,D,E) Clinical manifestation • Retardation • Hepatoslenomegaly • Lymphadenopathy • Pigmentation • Impaired neurologic function • Niemann-Pick cells – lipid-laden giant foam cells found in affected tissues Niemann-Pick disease Niemann-Pick disease type A Deficiency of the sphingomyelinase enzyme → accumulation of unmetabolized sphingomyelin Sphingomyelin – sphingophospholipd - constituent of the cell membrane • Known as infantile or classic Niemann Pick • Appears during infancy • Characterized by Hepatoslenomegaly • Failure to thrive • Progressive deterioration of the nervous system. • Known as the neurological type. • Children affected by this condition generally do not survive past early childhood Niemann-Pick disease Niemann-Pick disease type B • Deficiency of the sphingomyelinase enzyme • Chronic or adult form • Features include Hepatoslenomegaly • Growth retardation • Problems with lung function including frequent lung infections. • Decreased platelets • Niemann-Pick disease type B is also known as the non-neurological type because the nervous system is not usually affected • Live longer than type A – Type B usually survive into adulthood Niemann-Pick disease Niemann-Pick disease type C • Mutations in either the NPC1 or NPC2 gene • The NPC1 gene involve with cholesterol transport within cells Cholesterol and sphingomyelin accumulates • Most common form with onset in early childhood • Severe liver disease • Breathing difficulties • Developmental delay • Neurologic abnormalities • Can survive into adulthood • Types C1 and C2, caused by NPC1 and NPC2, respectively Infantile or juvenile and Adolescent or adult form Niemann-Pick disease No effective treatment for Niemann-Pick allogeneic BM transplant done for type B with encouraging results Splenectomy rarely required – death usually occurs before Prognosis of type A – very poor Type B – may survive into childhood or adult life Type C – die usually in second decade of life Tay-Sachs disease • Also known as GM2 gangliosidosis • Rare autosomal recessive sphingolipidosis as a result of hexosaminidase A deficiency • Most common variant - infantile Tay–Sachs disease • Causes a progressive deterioration of nerve cells and of mental and physical abilities • Starts at ~ 6mths of age • Results in death by the age of four • Accumulation of harmful quantities of gangliosides in almost all tissues → the premature death Affects central nervous system and eye Cherry red spot in macula of each eye Macrocephaly • 1in 30 carrier rate in the Ashkenazi Jewish population Tay-Sachs disease Diagnosis • Peripheral blood contains vacuolated lymphocytes • Prenatal detection • Detection of hexosaminidase A levels in serum, plasma, leukocytes and cultured fibroblasts of infants • Mass screening of adults Prognosis and treatment • Fatal before age 4 • Attempting enzyme replacement, results not yet known • Supportive treatment – manage hydration, infections, seizures Mucopolysaccharidoses (MPS) • Rare disorder • Caused by the absence or malfunctioning of lysosomal enzymes needed to break down mucopolysaccharides – long chains of sugar carbohydrates in each of our cells that help build bone, cartilage, tendons, corneas, skin and connective tissue. • Mucopolysaccharides (also called glycosaminoglycans) are also found in the joint fluid • Deficiency of one of the enzymes involved in mucopolysaccharide metabolism • Glycosaminoglycans collect in the cells, blood and connective tissues → permanent, progressive cellular damage which affects appearance, physical abilities, organ and system functioning, and, in most cases, mental development • Arranged into seven categories Mucopolysaccharidoses (MPS) Histiocytosis Abnormal proliferation and accumulation of mature histiocytes or Langerhans's cells Sea blue histiocyte syndrome Striking blue color of histiocytes after staining with Wright’s stain Isolated in young adults with enlarged spleen Abnormalities of the eye, skin, nervous system, lung Laboratory findings confined to the blood Thrombocytopenia Most have normal life spans