PBL Patient case 12
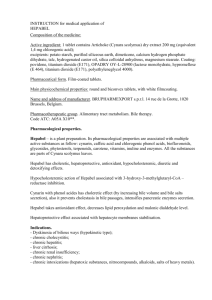
advertisement

PBL Patient case 12: Obstructive Jaundice Basic Anatomy Signs and Symptoms - N+V Fever Abdo pain – o RUQ, radiating to R shoulder, back Local peritonism GB mass +ve Murphy’s sign Sites of Obstruction 1. - Gall Bladder or Cystic Duct ASx (70%) RUQ Pain (++ fatty foods) Biliary Colic (Colicky epigastric P) Cholecystitis (RUQ P + Fever) - Empyema of GB - Porcelain GB (Calcification) - Rarely perforation – biliary peritonitis 2. CBD (Choledocholithiasis) - Cholestatic Jaundice - Ascending Cholangitis (Rigors, Jaundice, RUQ pain) 3. Pancreatitis - Migration of stones down CBD thru ampulla of Vater - Epigastric Pain radiating to back Risk Factors of Cholesterol Stones Female Forties (unusual < 30 yrs) Fat Multiparity Diet (High animal fat) Contraceptive pill Ileal disease or resection Diabetes Acromegaly Rx with octreotide Consequences of Gall Stones 1. Asymptomatic gallstones 2. In Gall Bladder - Biliary Colic o Obstruction at any part of billary tree (cystic duct to Sphincter of Oddi) o Severe constant pain RUQ radiate shoulder/subscapular, N&V, fevers, rigors, - Cholecystitis (Acute and Chronic) o Can cause empyema – spread infection or burst (but rare due to dual blood supply) - Empyema/Mucocele o Obstructed GB fills with pus/mucous - Carcinoma - Mirizzi’s Syndrome o Jaundice with acute cholecystitis without CBD stone put compression of CBD due to stone in cystic duct 3. In the bile ducts - Cholangitis - Pancreatitis - Obstructive jaundice 4. In the gut - Gallstone Ileus – SB obstruction o Large stone erodes through GB into duodenum can obstruct T.I. @ ileocecal valve o (X-ray: pneumobilia, small bowl fluid levels, stone) Bile Consists of: - Bile acids - Cholesterol - Phospholipids - Conjugated bilirubin - Water and electrolytes Synthesis of Bile Acids - Bile acids are not present in the diet, and are synthesized in the liver by enzymes - Primary bile acids are synthesized in the liver from cholesterol (cholic acid and chenodeoxycholic acid) - Secondary bile acids are synthesized from primary bile acids in the intestine by colonic bacterial enzymes (deoxycholic acid and lithocholic acid) - Bile acids will be conjugated to form tauro or glyco- conjugated bile acids secreted into duodenum in bile Synthesis of Conjugated Bilirubin - Produced mainly from breakdown of mature RBC in the Kupffer cells of the liver and RES - Biliverbin is formed from haem and is reduced to form bilirubin - Br is unconjugated and water- insoluble transported to liver attached to albumin - Bilirubin dissociates from albumin and taken up by hepatic cells where it is conjugated with glucuronic acid and excreted into bile Role of Bile in Digestion - Bile acids help to emulsify fats in food by forming micelles increases surface area for the action of pancreatic lipase (digestion) - Increases absorption of fat soluble vitamins (A,D,E,K) - Bile also serves as a route of excretion for bilirubin (RBC degradation by- product) - Neutralizes excess stomach acid before entering ileum - Bile salts also act as bacteriocides kills bacteria that may be present in food Enterohepatic Circulation - Primary bile acids are synthesized in the liver from cholesterol conjugated pass into duodenum and aid digestion and absorption of fat - Reabsorption of bile acids occur mainly in the ileum by an active transport mechanism return back to the liver via the portal vein (enterohepatic circulation) - 95-98% of total circulating bile acids are absorbed each day - Only a small quantity escapes reabsorption and is excreted in the faeces - To maintain status quo, the liver will then synthesize enough bile acids to match the faecal loss - At the terminal ileum, free Br is reduced to urobilinogen some will be excreted as stercobilinogen and urobilinogen remainder will be reabsorbed and passed to the liver via E.C Pathophysiology Types of Gallstones - Cholesterol gallstones (80% in western countries) - Pigment stones (predominantly calcium bilirubinate or polymer- like complexes with calcium, copper and some cholesterol) Cholesterol Gallstones Due to cholesterol crystallization from gall bladder bile 1. Excess of cholesterol and deficit of bile salts in bile imbalance between ratio of cholesterol and bile salts 2. Crystallization- promoting factors within bile 3. Motility of gall bladder Bile Pigment Gallstones Black pigment stones: - Seen in patients with haemolytic conditions eg sickle cell disease excessive secretion of Br Brown Pigment stones: - Presence of bile stasis and/ or biliary infection Obstructive Jaundice Gradual Obstruction of CBD over weeks/months - Gallstones - Carcinoma of CBD - Carcinoma of head of pancreas - Inflammatory stricture of CBD • • • • • • Biliary obstruction causes progressive dilatation of intrahepatic bile ducts as intrabiliary pressures rise Hepatic bile flow is suppressed reabsorption and regurgitation of conjugated Br into the blood stream Leads to jaundice accompanied by dark urine and light- colored stools ALP is raised with only slight elevation in aminotransferases If biliary obstruction persists, there is a risk the static bile will become infected causing acute cholangitis and eventually liver abscesses Lack of bile in small intestine causes malabsorption of fat and fat- soluble substances Investigations Liver Function Tests: • Serum bilirubin – elevated • AST, ALT – normal or slightly elevated • ALP – elevated (4-10x normal) • Albumin – usually normal • GGT – elevated • PTT, INR – usually normal Abdominal Ultrasound - Size of biliary tracts - Degree of obstruction - Can determine cause of obstruction Abdominal CT - Can visualise biliary tree - Very good at detecting calcified stones and malignancies ERCP (Endoscopic retrograde cholangiopancreatography) An endoscope is passed through the mouth, esophagus and stomach to the 2nd part of the duodenum. A catheter is passed up the ampulla of vater into the CBD, and dye is injected. - Allows visualisation and access to the biliary and pancreatic ducts - Sphincterotomy and stone extraction can be performed - Has a significant risk of pancreatitis (5%) - Current gold standard imaging for pancreatobiliary tree. MRCP (Magnetic resonance cholangiopancreatography) An MRI method of visualising the pancreatobiliary tree. - Non-invasive (no contrast is required) Management Cholelithiasis - Asymptomatic stones: attempt dissolution (ursodeoxycholic acid). o Reduce Risk factors - Symptomatic stones : laparoscopic cholecystectomy. Complications - Cholecystitis - Choledocolithiasis, - Cholangitis - Fistula formation - Pancreatitis. Prognosis Asymptomatic gallstones become symptomatic at about 2%/year, once symptoms (biliary colic) begin they recur at 40%/year and progress to a complication at 2%/year. Choledocolethiasis Endoscopic Retrograde Cholangiopancreatography Indications: Cholangitis, jaundice + dilated intrahepatic ducts, jaundice + normal calibre ducts + non-diagnositic liver biopsy, recurrent pancreatitis, post-cholecystectomy pain Therapeutic ERCP: Sphincterotomy (CBD stones), Stenting of malignant strictures Prophylaxis: o Check LFTs clotting + platelets o Antibiotics (Ciprofloxacin) o Analgesic (Morphine/Metoclopramide) o Sedation (Midazolam) Complications: o Pancreatitis, bleeding, cholangitis, perforation Acute Cholecystitis Medical: NBM nil by mouth, Pain relief, IVI + Cefuroxime (1.5g/8h IV) Surgical: consider cholescystectomy (laporoscopic) within 72hours OR after 6/12 weeks Mortality < 1% Relapse (18%) - if not within time frame Complications Gall bladder perforation/rupture Ascending cholangitis Pancreatitis Peritonitis Prevention Removal of the gallbladder and gallstones will prevent further attacks. Following a low-fat diet if prone to gallstone attacks. Cholangitis Quick diagnosis and treatment are very important. Antibiotics to cure infection are tried first for most patients. ERCP or other surgical procedure is done when the patient is stable. Patients who are very ill or are quickly getting worse may need surgery right away. Complications Sepsis Prevention Treatment of gallstones, tumors, and infestations of parasites may reduce the risk for some people. A metal or plastic stent within the bile system may be needed to prevent recurrence. Patient Case – Mr P Presentation 31 y.o plumber 22/4 – presented to ED ◦ Sudden onset epigastric pain ◦ 8/10, colicky Ix – ◦ ECG: ST elevation in leads II and III ◦ Cardiac enzymes: normal ◦ AST: 44U/L (10-40) ◦ Lipase: 62U/L (10-55), *amylase not done Pain resolved, discharged 23/4 25/4 – presented via ambulance ◦ Epigastric pain ◦ Increasing severity 10/10, radiating to back ◦ SOB (but not O/E) ◦ Noted ‘tingling’ in L arm ◦ N+V (3x) ◦ Jaundiced (not marked) Ix – ◦ FBE, U+Es, LFTs, troponin, CK, amylase, lipase ◦ Upper abdo US DDx Cardiac – ◦ Acute coronary syndrome Abdo – ◦ Pancreatitis ◦ Cholecystitis, Biliary colic ◦ Acute hepatitis ◦ Peptic ulcer disease Resp – ◦ Pneumonia Past Hx Jan 2011 – similar episode of abdo pain 2/52 ago – N+V, ? ‘food poisoning’ 1986 – tonsillectomy 1998 – L shoulder reconstruction Otherwise fit and healthy ◦ NKA ◦ No current Rx FHx Mum ◦ Cholecystectomy 2010 ◦ Hypertension Dad ◦ Thyroidectomy 2009 (benign nodules) Sister – A+W Social Hx Never smoked etOH ◦ 4-6 SDs daily (regular beers) ◦ no AFDs Lives with partner (nurse) Runs own plumbing business Ix Results Cardiac enzymes – normal FBE – mild neutrophilia LFTs: ◦ T Bilirubin – 30 umol/L (4-20) ◦ ALP – 112 U/L (35-110) ◦ GGT – 325 U/L (5-50) ◦ ALT – 182 U/L (5-40) ◦ AST – 264 U/L (10-40) Upper abdo US ◦ Thickened gallbladder wall (4.2mm) ◦ Multiple immobile calculi and sludge ◦ No ductal dilatation Normal CBD (3.9mm) ◦ Mild fatty infiltration of liver ◦ Normal spleen, pancreas and kidneys Rx Surgery: ◦ Laparoscopic cholecystectomy ◦ Intra-op cholangiogram ◦ Umbilical hernia repair (incidental finding on pre-operative Ex) Pt reports some abdominal tenderness, poor appetite, no N+V Dressings over 4x lap ports Mildly jaundiced (skin and sclera) ◦ Pt’s partner reports this is resolving F/U