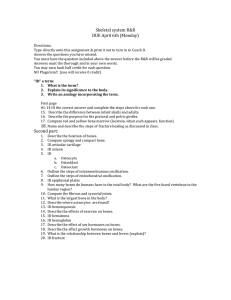
skeletal system
advertisement

The Skeletal System Functions of the Skeletal System • • • • • • • Support Permission of movement Blood cell formation (hematopoiesis) Protection Detoxification (removal of poisons) Provision for muscle attachment Mineral storage Bone Classification • Bones are classified according to shape • Long bones are long with expanded ends, Ex: forearm and thigh bone • Short bones are cube like, Ex: wrist, ankle • Flat bones are broad and plate like, Ex: ribs, scapulae, and some skull bones • Irregular bones vary in shape, Ex: vertebrae • Sesamoid or round bones are small bones embedded in tendons, Ex: kneecap (patella) Parts of Bone • Epiphysis: end of the bone which articulates (forms a joint) with another bone. • The epiphyses are composed of spongy bone and covered with hyaline cartilage called articular cartilage. Figure 7.2 Parts of Bone • Diaphysis: shaft of the bone between the epiphyses, composed of compact bone with a medullary cavity in the center. Parts of Bone • Periosteum: fibrous tissue covering of the bone. Compact Bone • Osteocytes and layers of intercellular material lie in concentric rings around an osteonic canal. • This unit is called an osteon or Haversian system. • Osteonic canals contain blood vessels and nerve fibers and are interconnected by transverse perforating (Volkmann’s) canals. Microscopic Structure of Bone: Compact Bone Figure 6.6a, b Spongy Bone • Osteocytes lie within trabeculae, branching bony plates. • Nutrients diffuse into canaliculi that lead to the trabeculae. Bone Growth and Development • The skeletal system begins to form during the first weeks of prenatal development. • Some bones originate within sheets of connective tissue (intramembranous bones). • Some bones begin as models of hyaline cartilage that are replaced by bone (endochrondral bones). Intramembranous Bones • Broad, flat skull bones are intramembranous bones. • During osteogenesis layers of primitive, connective tissue supplied with blood vessels appear at the site of future bone. Intramembranous Bones • Cells differentiate into osteoblasts (bonebuilding cells) which deposit spongy bone. • Osteoblasts become osteocytes when surrounded by bony matrix in lacunae. Intramembranous Bones • Connective tissue on the surface of the bone forms the periosteum. • Osteoblasts on the inside of the periosteum deposit compact bone over spongy bone. • This process is called intramembranous ossification. Endochondral Bones • Hyaline cartilage forms a model of the bone during embryonic development. • Cartilage degenerates, periosteum forms. • Periosteal blood vessels and osteoblasts invade the bone forming a primary ossification center in the diaphysis. • Secondary ossification centers develop in the epiphyses. Endochondral Bones • Osteoblasts form spongy bone in the space occupied by cartilage. • Osteoblasts become osteocytes when bony matrix surrounds them. Endochondral Bones • Osteoblasts beneath the periosteum deposit compact bone around spongy bone. • A band of cartilage remains between the diaphysis and epiphyses as the epiphyseal disk. Bone Growth • Growth of long bones occurs along four layers of cartilage in the epiphyseal disk. • First Layer: resting cells that do not grow. • Second Layer: young mitotic cells. • Third Layer: older cells that enlarge. • Fourth Layer: dead cells and calcified intercellular substances. Formation of the Bony Skeleton • Begins at week 8 of embryo development • Intramembranous ossification – bone develops from a fibrous membrane • Endochondral ossification – bone forms by replacing hyaline cartilage Intramembranous Ossification • Formation of most of the flat bones of the skull and the clavicles • Fibrous connective tissue membranes are formed by mesenchymal cells Stages of Intramembranous Ossification • An ossification center appears in the fibrous connective tissue membrane • Bone matrix is secreted within the fibrous membrane • Woven bone and periosteum form • Bone collar of compact bone forms, and red marrow appears Stages of Intramembranous Ossification Figure 6.7.1 Stages of Intramembranous Ossification Figure 6.7.2 Stages of Intramembranous Ossification Figure 6.7.3 Stages of Intramembranous Ossification Figure 6.7.4 Endochondral Ossification • Begins in the second month of development • Uses hyaline cartilage “bones” as models for bone construction • Requires breakdown of hyaline cartilage prior to ossification Stages of Endochondral Ossification • Formation of bone collar • Cavitation of the hyaline cartilage • Invasion of internal cavities by the periosteal bud, and spongy bone formation • Formation of the medullary cavity; appearance of secondary ossification centers in the epiphyses • Ossification of the epiphyses, with hyaline cartilage remaining only in the epiphyseal plates Stages of Endochondral Ossification Secondary ossification center Epiphyseal blood vessel Deteriorating cartilage matrix Hyaline cartilage Spongy bone formation Primary ossification center Bone collar Articular cartilage Spongy bone Medullary cavity Epiphyseal plate cartilage Blood vessel of periostea l bud 1 Formation of bone collar around hyaline cartilage model. 2 Cavitation of the hyaline cartilage within the cartilage model. 3 Invasion of internal cavities by the periosteal bud and spongy bone formation. 4 Formation of the medullary cavity as ossification continues; appearance of secondary ossification centers in the epiphyses in preparation for stage 5. 5 Ossification of the epiphyses; when completed, hyaline cartilage remains only in the epiphyseal plates and articular cartilages Figure 6.8 Postnatal Bone Growth • Growth in length of long bones – Cartilage on the side of the epiphyseal plate closest to the epiphysis is relatively inactive – Cartilage abutting the shaft of the bone organizes into a pattern that allows fast, efficient growth – Cells of the epiphyseal plate proximal to the resting cartilage form three functionally different zones: growth, transformation, and osteogenic Functional Zones in Long Bone Growth • Growth zone – cartilage cells undergo mitosis, pushing the epiphysis away from the diaphysis • Transformation zone – older cells enlarge, the matrix becomes calcified, cartilage cells die, and the matrix begins to deteriorate • Osteogenic zone – new bone formation occurs Long Bone Growth and Remodeling • Growth in length – cartilage continually grows and is replaced by bone as shown • Remodeling – bone is resorbed and added by appositional growth as shown Long Bone Growth and Remodeling Figure 6.10 Appositional Growth of Bone Central canal of osteon Periosteal ridge Artery Periosteum 1 Osteoblasts beneath the periosteum secrete bone matrix, forming ridges that follow the course of periosteal blood vessels. Penetrating canal 2 As the bony ridges enlarge and meet, the groove containing the blood vessel becomes a tunnel. 3 The periosteum lining the tunnel is transformed into an endosteum and the osteoblasts just deep to the tunnel endosteum secrete bone matrix, narrowing the canal. 4 As the osteoblasts beneath the endosteum form new lamellae, a new osteon is created. Meanwhile new circumferential lamellae are elaborated beneath the periosteum and the process is repeated, continuing to enlarge bone diameter. Figure 6.11 Bone Remodeling • Remodeling units – adjacent osteoblasts and osteoclasts deposit and resorb bone at periosteal and endosteal surfaces Bone Homeostasis • After bone formation, osteoclasts and osteoblasts continue to remodel the bone. • Resorption and deposition are regulated to keep bone mass constant. Nutrition and Bone Development • Vitamin D is necessary to absorb calcium in the small intestine. • Vitamin D deficiency leads in rickets in children and osteomalacia in adults. Nutrition and Bone Development • Vitamin A is necessary for osteoblast and osteoclast activity. • Vitamin C is necessary for collagen synthesis. Hormones and Bone • Growth Hormone (GH) stimulates epiphyseal cartilage cell division. • Deficiency of G H: pituitary dwarfism. Excess GH: pituitary gigantism in children and acromegaly in adults. Hormones and Bone • Thyroid hormone stimulates cartilage replacement in the epiphyseal disks. • Sex steroids promote formation of bone tissue close the epiphyseal disk. Physical Factors Affecting Bone • Physical stress stimulates bone growth. • Weight bearing exercise stimulates bone tissue to thicken and strengthen (hypertrophy). • Lack of exercise leads to bone wasting (atrophy). Bone Function • Bones shape, support, and protect body structures. • Bones act as levers to create body movement with muscles. • Bones house blood cell producing tissue. • Bones store inorganic salts. Support and Protection • Bones give shape to the head, face, chest, and limbs. • Bones of the skull protect structures like the eyes, ears, and brain. • Bones of the rib cage and shoulder protect the heart and lungs. • Bones of the pelvic girdle protect the abdominal and reproductive organs. Body Movement • When body parts move, bones and muscle act as levers. Body Movement • A lever has four parts: a bar, a fulcrum, an object moved, a force to supply energy. • There are three classes of levers. Figure 7.13 Body Movement Body Movement Body Movement Figure 7.14 Body Movement Fracture Repair • Blood escapes from damaged blood vessels and forms a hematoma. • Spongy bone forms in regions near blood vessels and fibrocartilage forms farther away. • A bony callus replaces the fibrocartilage. • Osteoclasts remove excess bony tissue, restoring new bone much like the original. Blood Cell Formation • Blood cell formation (hematologists) occurs in yolk sac in early development. • Later it occurs in the liver and spleen. • In the adult red and white blood cells are formed in the red bone marrow. Blood Cell Formation • Red marrow fills the cavity in the diaphesis of the long bones in infants. In adults it is replaced with yellow marrow (fat). • Adult red marrow is found in spongy bone of the skull, ribs, sternum, vertebrae, pelvis. Inorganic Salt Storage • Salts account for 70% of the bone matrix. • These salts are mostly calcium phosphate crystals called hydroxyapatite. Inorganic Salt Storage • Parathyroid hormone stimulates osteoclasts to break down bone when Ca levels are low. • Calcitonin stimulates osteoblasts to build bone when Ca levels are high. • Bone contains Mg, Na, K, and carbonate ions. Axial Skeleton • The skeleton has two divisions: the axial and the appendicular skeleton. • The axial skeleton consists bones that support organs of the head, neck, and trunk. • Skull :cranium and facial bones. • Hyoid bone. • Vertebral column. • Thoracic cage: ribs and sternum. Appendicular Skeleton • The appendicular skeleton consists of the bones of the limbs and bones that anchor the limbs to the axial skeleton. • Pectoral girdle: scapula, clavicle. • Upper limbs: humerus, radium, ulna, carpals, metacarpals, phalanges. • Pelvic girdle: coxal bones. • Lower limbs: femur, tibia, fibula, patella, tarsals, metatarsals, phalanges. Figure 7.17 Figure 7.17 Cranium • • • • • • Frontal bone: forehead Parietal bones: top of the skull Occipital bone: back of the skull Temporal bones: side of skull, near ears Sphenoid bone:base of the cranium Ethmoid bone: roof of the nasal cavity Figure 7.19 Figure 7.19 Figure 7.21 Figure 7.21 Figure 7.22 Figure 7.22 Facial Skeleton • • • • • • • • Maxillary bones: upper jaw, hard palate Palatine bones: hard palate, nasal cavity Zygomatic bones: cheek bones Lacrimal bones: orbit of the eye Nasal bones: bridge of the nose Vomer bone: nasal septum Nasal conchae:walls of the nasal cavity Mandible: lower jaw Figure 7.29 Figure 7.29 Figure 7.29 Infantile Skull • The skull at birth is not fully developed. • Fibrous membranes, fontanels, connect the cranial bones. • The fontanels allow movement of the bones to enable the skull to pass through the birth canal. • The fontanels close as cranial bones grow. Figure 7.33 Figure 7.33 Vertebral Column • Cervical vertebrae: seven vertebrae of the neck, includes atlas and axis • Thoracic vertebrae: twelve vertebrae that articulate with the ribs • Lumbar vertebrae: five vertebrae that make up the small of the back Vertebral Column • Sacrum: five vertebrae that fuse in early adulthood, part of the pelvis • Coccyx: four small fused vertebrae Figure 7.34 Thoracic Cage • Ribs: twelve pair of ribs attached to each thoracic vertebrae. • Seven pairs: true ribs and attach to the sternum by costal cartilage. • Two pairs: false ribs that attach to cartilage. Thoracic Cage • Two pairs: floating ribs that do not attach to the sternum or its cartilage. • Sternum: the manubrium, the body, and the xyphoid process. Pectoral Girdle • Clavicles: collar bones that attach the sternum to the shoulder anteriorly. • Scapulae: shoulder blades with two processes. • Acromion process: tip of the shoulder. • Coracoid process: attaches to the clavicle and provides attachments for muscles. • Glenoid fossa articulates with the humerus. Figure 7.42 Upper limb • Humerus: upper arm bone, articulates with the glenoid fossa of the scapula Upper limb • Radius: thumb side of the forearm, articulates with the capitulum of the humerus and the radial notch of the ulna • Ulna: longer bone of the forearm, olecranon and coronoid processes articulate with the humerus Hand • Carpal bones: eight small bones of the wrist. • Metacarpal bones: five bones, the framework of the palm. • Phalanges: finger bones, three in each finger (proximal, middle, distal phalanx), two in the thumb. Figure 7.47 Pelvic Girdle • Coxal bones: two hips bones composed of three fused bones. • Ilium: superior part of the coxal bone. • Ischium: lowest portion of the coxal bone. • Pubis: anterior part of the coxal bone. The two pubic bones joint at the symphysis pubis. Figure 7.49 Figure 7.49 Male and Female Pelvis • Female iliac bones are more flared. • The female pubic arch angle is greater. • There is a greater distance between the ischial spines and tuberosities in the female. • The sacral curvature is shorter and flatter. • The differences create a wider pelvic cavity. Figure 7.51 Lower Limb • Femur: thigh bone, longest bone • Patella: kneecap, located in a tendon, femur, tibia, and patella form the knee joint • Tibia: shinbone, lateral malleolus forms the ankle • Fibula: slender bone lateral to the tibia, not part of the knee joint Figure 7.52 Foot • Tarsal bones: seven small bones in the ankle. The calcaneus (heel bone) is the largest, located below the talus. • Metatarsal bones: elongated bones that form the arch of the foot. • Phalanges: each toe has three except the great tow which has two. Figure 7.55 Life-Span Changes • Calcium levels fall through life and the skeleton loses strength. • Osteoclasts outnumber osteoblasts. Life-Span Changes • By age 35, everyone loses bone mass. Women lose bone mass faster between menopause and age seventy. • Trabecular bone is lost before compact bone.